Atelectasis, or the partial or complete collapse of lung tissue, is a fundamental topic that frequently appears on the NBRC TMC and Clinical Simulation Exams. Whether it’s identifying the condition on a chest radiograph, recognizing clinical signs in a post-operative patient, or recommending effective lung expansion therapy, understanding atelectasis is key to exam success—and more importantly, to competent respiratory care.
Since atelectasis can arise from various causes like hypoventilation, mucus plugging, or external compression, exam questions often test your ability to analyze clinical data and choose the most appropriate intervention.
In this article, we’ll break down essential concepts, common exam traps, and smart test-taking strategies to help you confidently tackle any atelectasis-related scenario on the boards.
Take our free course to learn essential tips, insights, and strategies to pass the TMC Exam on your first (or next) attempt.
What is Atelectasis?
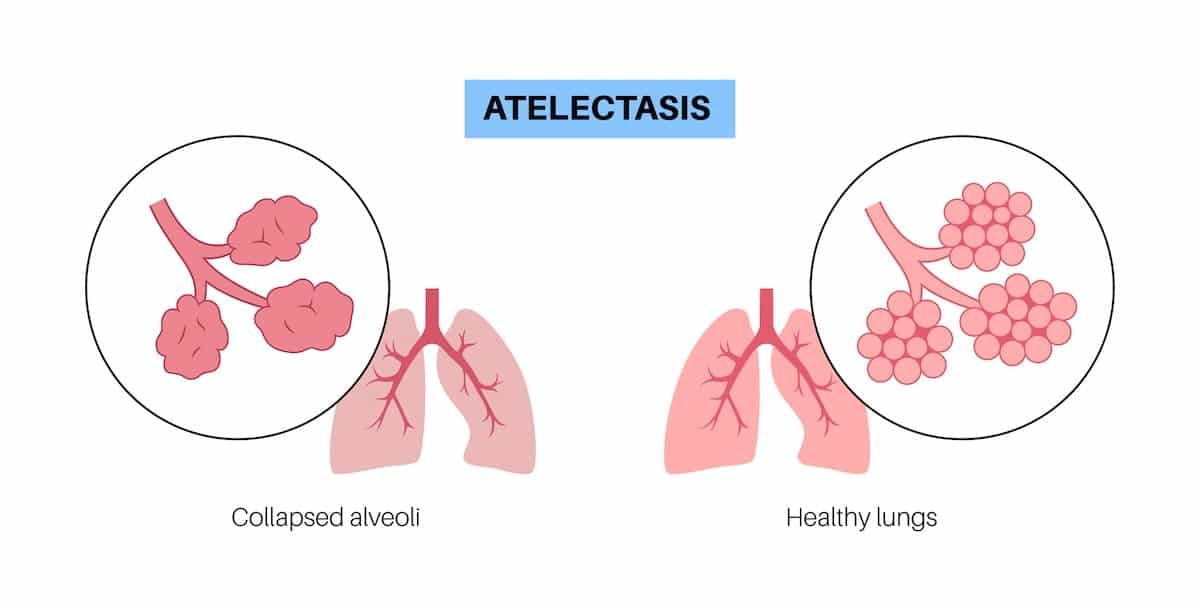
Atelectasis refers to the collapse or closure of alveoli, which results in reduced or absent gas exchange in a portion of the lung. It’s not a disease itself, but a clinical condition or complication that can arise from a variety of causes.
On the board exam, you’ll often see atelectasis described in the context of post-operative patients, airway obstruction, or conditions that limit deep breathing like sedation or chest trauma.
There are several types of atelectasis, each with different underlying mechanisms:
- Obstructive (Resorptive) Atelectasis: Occurs when the airway is blocked—commonly by mucus plugs, foreign bodies, or tumors—preventing air from reaching the alveoli. The trapped air gets absorbed, leading to alveolar collapse.
- Compressive Atelectasis: Caused by external pressure on the lung (e.g., pleural effusion, pneumothorax, or a tumor), squeezing the tissue and causing collapse.
- Postoperative Atelectasis: Common in surgical patients due to shallow breathing, pain, or sedation, leading to underinflation of alveoli.
- Adhesive Atelectasis: Seen in conditions like ARDS, where surfactant deficiency causes alveoli to collapse due to increased surface tension.
On a chest X-ray, atelectasis appears as an area of increased density (whiteness) with signs like tracheal deviation toward the affected side, elevation of the hemidiaphragm, and narrowing of rib spaces. Recognizing these findings is a high-yield skill for the TMC and CSE exams.
Understanding the types and mechanisms of atelectasis will help you not only answer direct questions on the board exam, but also reason through clinical simulations involving patients with poor ventilation or impaired airway clearance.
Exam Tip #1: Tracheal Shift for Atelectasis vs. Pneumothorax
On the TMC exam, tracheal deviation is a classic clue—but make sure you interpret it correctly. If the trachea shifts toward the affected side, it usually indicates volume loss from atelectasis. If it shifts away, think of volume gain, like in a tension pneumothorax.
Note: These subtle distinctions are test favorites and can help you quickly narrow down your choices.
Exam Tip #2: Think Incentive Spirometry for Post-Op Patients
On both the TMC and CSE exams, postoperative atelectasis is frequently tested. When you see a patient who recently had abdominal or thoracic surgery and is experiencing decreased breath sounds, low SpO₂, and diminished chest expansion, incentive spirometry (IS) is usually the best initial therapy.
Note: Don’t overthink it—early mobilization and IS are often the most appropriate first steps in these cases.
Exam Tip #3: Know When to Escalate Therapy
If a patient isn’t responding to basic lung expansion techniques like incentive spirometry, especially if they are lethargic or uncooperative, the next step may be intermittent positive pressure breathing (IPPB) or positive expiratory pressure (PEP) therapy.
On the CSE exam, watch for signs like shallow breathing, low vital capacity, or worsening chest X-ray findings—these are cues to escalate care. Think of it like a step ladder: IS → PEP → IPPB → CPAP, depending on the patient’s condition and alertness.
Exam Tip #4: Mucus Plug? Suction or Bronchoscopy
If the question scenario suggests sudden drop in breath sounds, oxygen saturation, or signs of lung collapse, especially in a ventilated or post-op patient, mucus plugging should be high on your differential.
In those cases, therapeutic suctioning is often the first move. If suctioning is unsuccessful or the patient is unresponsive to basic interventions, diagnostic or therapeutic bronchoscopy may be indicated. This is especially important in cases where you must act on changes in patient status quickly.
Exam Tip #5: Atelectasis Causes a Shunt-Like Effect
When alveoli collapse, they are perfused but not ventilated—leading to intrapulmonary shunting. This results in refractory hypoxemia, which means the patient’s oxygen levels may not significantly improve with just increased FiO₂.
Note: On the TMC exam, recognize that lung expansion therapy, not simply more oxygen, is key to resolving hypoxemia caused by atelectasis.
Exam Tip #6: Monitor for Decreased Compliance on the Ventilator
In mechanically ventilated patients, the development of atelectasis may show up as increasing peak and plateau pressures, indicating reduced lung compliance. If you see this pattern, assess breath sounds and chest movement, and consider atelectasis—especially if imaging supports it.
Note: Lung recruitment maneuvers or adjusting PEEP may be required, depending on the patient’s condition and ABG results.
Exam Tip #7: Atelectasis in Newborns? Think Surfactant Deficiency
In neonatal cases, especially preterm infants, atelectasis is often caused by a lack of surfactant, leading to infant respiratory distress syndrome (IRDS).
If you see ground-glass appearance on chest X-ray, nasal flaring, and retractions in a premature baby, suspect IRDS with associated atelectasis. The correct intervention may be exogenous surfactant administration and/or CPAP to keep alveoli open.
Exam Tip #8: Look for Underlying Causes—Don’t Just Treat the Collapse
Atelectasis is often a symptom of an underlying problem. On the CSE, you may need to go beyond treating the collapse itself. For example, if the patient has signs of poor pain control, consider recommending better analgesia to improve deep breathing.
If the collapse is from foreign body aspiration, bronchoscopy may be the right call. Always ask: why did the atelectasis occur? Addressing the root cause is key to getting full credit on decision-making steps.
Exam Tip #9: Know When Not to Use CPAP
While CPAP can be effective in treating atelectasis by helping recruit collapsed alveoli, it’s not appropriate for every patient. On the TMC or CSE, avoid CPAP if the patient is hypoventilating, heavily sedated, or has excessive secretions. These patients may not generate enough effort to trigger the device—or may even need invasive support.
Note: Always consider the patient’s alertness and ability to cooperate before choosing CPAP.
Exam Tip #10: Re-Check After Intervention
On the CSE, after you initiate a therapy like incentive spirometry or IPPB, you’ll often be given a chance to reassess. Don’t forget this step! Look for improved breath sounds, increased SpO₂, or better chest expansion.
If there’s no improvement, it’s your cue to escalate therapy. Reassessment is your chance to show clinical judgment and can earn crucial points on the simulation.
Exam Tip #11: Sudden Atelectasis After Intubation? Check Tube Placement
If a patient suddenly develops signs of atelectasis after being intubated—like decreased breath sounds on the left, uneven chest rise, or tracheal shift—think right mainstem intubation.
This is a common cause of unilateral atelectasis. The fix? Pull the endotracheal tube back slightly and re-confirm placement (usually at 21–23 cm at the teeth). This is a classic CSE scenario.
Integrating Study Resources for Exam Preparation
Preparing for the TMC and CSE exams requires more than memorization—it requires the ability to apply knowledge to real-world clinical situations. Utilize the following resources to strengthen your skills:
- TMC Test Bank: Practice interpreting patient scenarios with over 640 premium questions designed to mimic real exam questions.
- TMC Exam Hacks: Watch strategy-focused videos that break down key exam topics, including patient data evaluation.
- Daily Practice Questions: Reinforce your skills daily by reviewing practice questions on various topics, such as ABG interpretations, lab results, imaging studies, and more.
- CSE Boost Course: Build confidence in your decision-making abilities through simulation-based learning to prepare for the unique exam format.
Note: By dedicating time to mastering the components of the patient medical record and practicing with real-life scenarios, you’ll be better prepared to handle the complexities of the TMC and CSE exams—and ultimately provide high-quality, evidence-based respiratory care.
Get instant access to four premium courses designed to help you pass the TMC/CSE exams—CSE Boost Course, TMC Test Bank, TMC Exam Hacks, and Daily Practice Questions. Bundle and save with everything you need for exam success.
Final Thoughts
Atelectasis is a frequently tested topic on both the TMC and CSE exams, and for good reason—it’s a common, clinically significant condition that respiratory therapists must recognize and manage confidently.
From identifying radiographic signs and understanding underlying causes to selecting the right therapeutic interventions, your ability to think critically about atelectasis will be key to passing the boards and succeeding in real-world practice.
By mastering the tips in this guide and practicing clinical reasoning, you’ll be well-equipped to handle any atelectasis-related question that comes your way on exam day.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Grott K, Chauhan S, Sanghavi DK, et al. Atelectasis. [Updated 2024 Feb 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.



