For many respiratory therapy students, interpreting arterial blood gases (ABGs) and making an accurate diagnosis can feel like one of the most intimidating hurdles on the path to board exam success—and even more so in real-world clinical practice.
It’s not just about recognizing whether the pH is acidotic or alkalotic, or whether CO₂ is elevated or low. The real challenge comes next: understanding what to do after identifying the problem. Knowing the causative issue is only the first piece of the puzzle. The next crucial step is making the right clinical decisions to correct the imbalance and improve patient outcomes.
This is where many students get stuck—not at recognizing the problem, but at confidently deciding on the appropriate action. In this article, we’ll break down a clear, practical approach to ABG interpretation and diagnosis, then guide you through the essential steps to take after you’ve pinpointed the issue.
Whether you’re preparing for the TMC or CSE exams, or simply aiming to strengthen your clinical reasoning, this roadmap will help turn ABG anxiety into ABG mastery.
Take our free course to master the basics of ABG interpretation with clear explanations and helpful practice questions.
How to Interpret an ABG?
To interpret an ABG, follow a step-by-step approach. First, assess the pH to determine if the blood is acidotic (<7.35), alkalotic (>7.45), or normal. Next, examine PaCO₂ (35–45 mmHg) to evaluate the respiratory component and HCO₃⁻ (22–26 mEq/L) for the metabolic component.
Use the ROME method—Respiratory Opposite, Metabolic Equal—to identify the primary imbalance. Then, check for compensation: if the other value is adjusting in the expected direction, compensation is occurring. Finally, assess oxygenation status via PaO₂ and SaO₂ levels.
Always interpret results within the clinical context, considering symptoms and underlying conditions. Accurate ABG interpretation helps guide treatment decisions for conditions like COPD, DKA, and drug overdose.
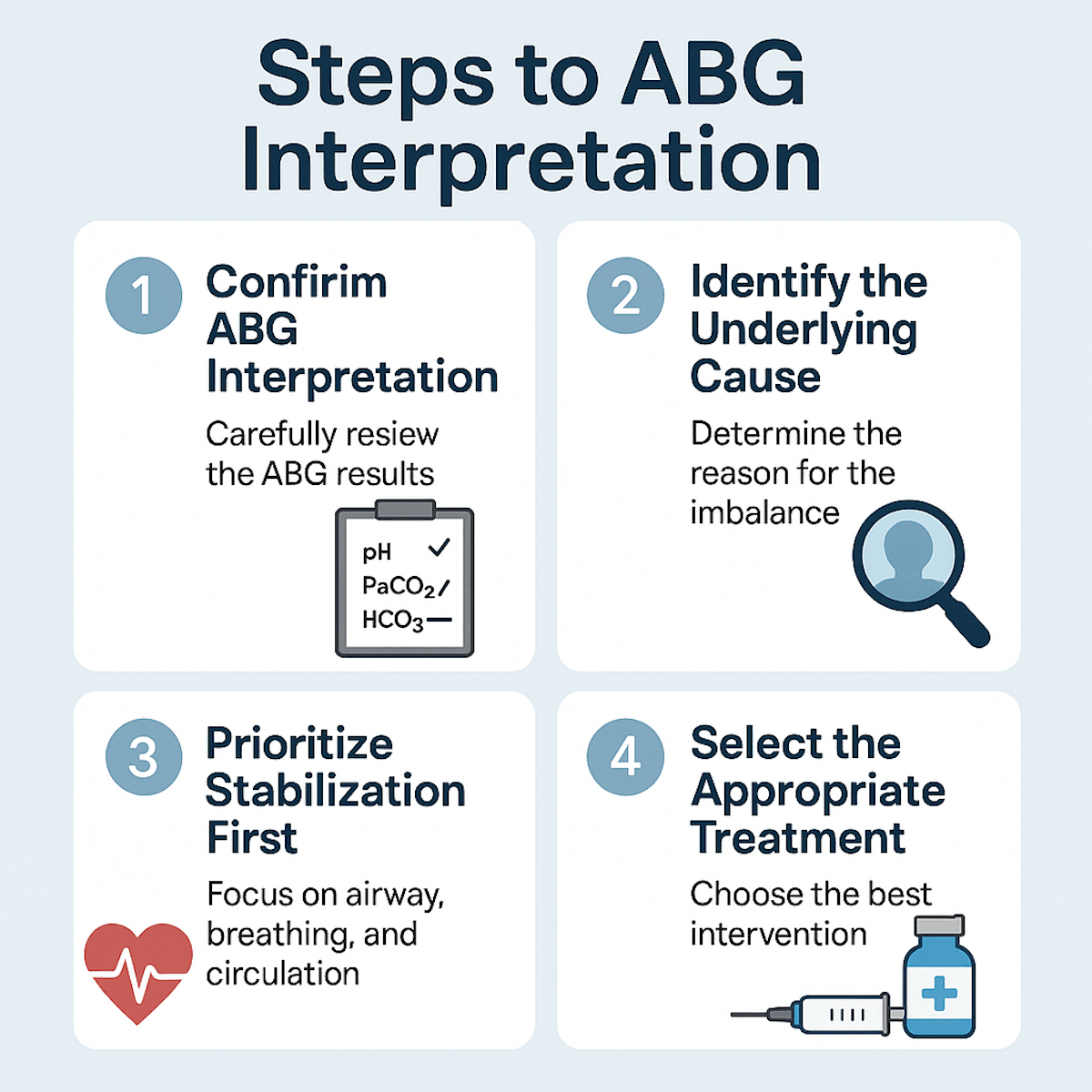
Step 1: Confirm Your ABG Interpretation Before Taking Action
Before jumping to treatment decisions, pause and double-check your ABG analysis. Many mistakes happen not because students don’t know the correct intervention—but because they misinterpret the initial ABG results. Always work through these questions systematically:
- Is the pH acidotic, alkalotic, or normal?
- Is the primary disturbance respiratory or metabolic?
- Is there evidence of compensation?
- What is the severity of oxygenation status (mild, moderate, severe hypoxemia)?
Use a logical approach like “ROME” (Respiratory Opposite, Metabolic Equal) or follow a flowchart to avoid second-guessing yourself.
Remember, treating the wrong problem—like giving bicarbonate to a fully compensated respiratory acidosis—can worsen the patient’s condition. Confidence begins with a clear and confirmed interpretation.
Step 2: Identify the Underlying Cause, Not Just the Label
It’s easy to stop at “this is respiratory acidosis,” but that’s only part of the story. Ask yourself: Why is the patient hypoventilating? Is it COPD, drug overdose, neuromuscular weakness, or something else entirely?
Each ABG pattern points toward different possible causes:
- Respiratory Acidosis → Hypoventilation (COPD, sedation, neuromuscular issues)
- Respiratory Alkalosis → Hyperventilation (pain, anxiety, hypoxemia, pulmonary embolism)
- Metabolic Acidosis → DKA, lactic acidosis, renal failure, diarrhea
- Metabolic Alkalosis → Vomiting, diuretics, hypokalemia
Note: Your treatment choices depend on this root cause. For example, increasing ventilation is helpful in CO₂ retention from COPD exacerbation, but not in metabolic acidosis from DKA, where insulin therapy is needed.
Step 3: Prioritize Stabilization First
No matter how sharp your ABG interpretation skills are, patient safety comes first. If the ABG shows severe hypoxemia or life-threatening pH changes, oxygenation and ventilation support are your immediate priorities—even while you work on the root cause.
- Severe hypoxemia → Administer oxygen, consider non-invasive ventilation (BiPAP), or intubate if needed.
- Acute ventilatory failure with rising CO₂ and worsening pH → Prepare for mechanical ventilation.
- Metabolic acidosis with severe acidemia (pH < 7.1) → Manage the underlying cause but consider bicarbonate cautiously if indicated.
Note: Always stabilize the airway, breathing, and circulation (ABCs) first. Treatment plans can wait—life support cannot.
Step 4: Select the Appropriate Treatment Based on the Diagnosis
Once you’ve identified the primary problem and its cause, your next move is choosing the correct intervention. This is where critical thinking truly shines, and where many students either over-treat or miss the mark by reaching for the wrong tool.
For a COPD exacerbation with CO₂ retention, treatment focuses on the use of bronchodilators and corticosteroids, along with oxygen therapy administered cautiously. Noninvasive ventilation such as BiPAP is often recommended, with mechanical ventilation considered if necessary.
In the case of an opioid overdose leading to hypoventilation, the priority is to administer naloxone and provide ventilatory support as needed to maintain adequate oxygenation and ventilation.
For diabetic ketoacidosis (DKA), treatment involves administering intravenous fluids, starting an insulin drip, and carefully managing electrolytes, with particular attention to potassium levels.
When dealing with anxiety-induced hyperventilation, the focus is on reassuring the patient, coaching proper breathing techniques, and addressing the underlying cause of the anxiety.
In the event of a pulmonary embolism, treatment includes providing oxygen and initiating anticoagulation therapy. In severe cases, thrombolytic agents may also be considered.
For severe metabolic alkalosis, such as that caused by excessive vomiting, the primary approach involves replacing lost electrolytes like potassium and chloride. In extreme situations, acidifying agents may be considered to help correct the imbalance.
Step 5: Reassess and Monitor Your Intervention
Management doesn’t stop after choosing an intervention. ABG interpretation is not a “one and done” process—it’s dynamic. The next crucial step is to evaluate how your treatment is working and adjust as needed.
- Did oxygenation improve?
- Is CO₂ trending in the right direction?
- Has the pH begun to normalize?
- Are there any signs of over-correction (like oxygen-induced hypoventilation in COPD)?
Rechecking ABGs too soon or too late can lead to missing important changes. Follow institutional guidelines, but typically:
- 30 minutes to 1 hour after major ventilator changes.
- 1–2 hours after initiating non-invasive ventilation.
- Frequent monitoring in unstable patients, or those on continuous sedation/paralytics.
Bonus Tip: Always monitor clinically, not just through labs. Look at respiratory rate, work of breathing, mental status, SpO₂, and hemodynamics. Numbers matter—but so does the whole patient.
Step 6: Common Pitfalls to Avoid
- Jumping to treatment before confirming the problem.
- Treating the ABG numbers instead of the patient.
- Overcorrecting hypoxemia in CO₂ retainers (e.g., severe COPD).
- Ignoring compensation patterns (always treat the primary issue).
- Not reassessing after intervention—ABGs are a snapshot, not a full story.
ROME Method for ABG Interpretation
The ROME method is a simple way to remember how to identify whether an acid-base imbalance is respiratory or metabolic in nature. The word “ROME” stands for:
-
Respiratory = Opposite
-
Metabolic = Equal
Note: This means that in respiratory disorders, the pH and PaCO₂ levels move in opposite directions. In metabolic disorders, the pH and HCO₃⁻ levels move in the same direction.
Here’s how to use the ROME method step-by-step:
1. Check the pH
Start by determining if the pH is within the normal range of 7.35 to 7.45. If the pH is below 7.35, the patient is acidotic. If the pH is above 7.45, the patient is alkalotic.
2. Look at the PaCO₂
The normal range for PaCO₂ is 35 to 45 mmHg. Since PaCO₂ represents the respiratory component, if the pH and PaCO₂ are moving in opposite directions, the problem is respiratory.
For example, if the pH is low (indicating acidosis) and the PaCO₂ is high, this points to respiratory acidosis. If the pH is high and the PaCO₂ is low, this indicates respiratory alkalosis.
3. Look at the HCO₃⁻
The normal range for bicarbonate (HCO₃⁻) is 22 to 26 mEq/L. Because HCO₃⁻ reflects the metabolic component, if the pH and HCO₃⁻ are moving in the same direction, the issue is metabolic.
For example, if the pH is low and the HCO₃⁻ is also low, this is metabolic acidosis. If both the pH and HCO₃⁻ are elevated, this is metabolic alkalosis.
4. Determine if compensation is occurring
Once you’ve identified whether the imbalance is respiratory or metabolic, check for signs of compensation. If only one value (PaCO₂ or HCO₃⁻) is abnormal, the issue is uncompensated.
If both are abnormal but the pH is still outside the normal range, it is partially compensated. If both are abnormal but the pH has returned to the normal range, the patient is fully compensated.
Note: The ROME method is a great way to quickly organize your thought process when interpreting ABGs, especially under exam pressure or in clinical situations. Let me know if you’d like practice examples to help reinforce this method.
How to Approach ABG Questions on the Board Exam
When it comes to the board exam, ABG interpretation questions are rarely just about the numbers. Instead, they typically present a patient scenario and ask you to make a clinical decision based on both the ABG values and the patient’s condition.
This is where many students slip up — not because they can’t interpret the ABG correctly, but because they don’t connect the dots between the ABG results and what’s actually happening with the patient.
Here’s a step-by-step approach to help you confidently tackle ABG questions on the exam:
1. Read the Entire Scenario Carefully Before Looking at the ABG
-
What are the patient’s vital signs?
-
Are there any key symptoms (e.g., dyspnea, confusion, lethargy)?
-
Do they have a known condition like COPD, DKA, or drug overdose?
Note: Jumping straight to the numbers without understanding the context is one of the most common exam mistakes.
2. Use a Systematic ABG Interpretation Method
Apply a reliable method like this:
-
pH: Is it acidotic, alkalotic, or normal?
-
PaCO₂: Respiratory component — does it explain the pH shift?
-
HCO₃⁻: Metabolic component — is it compensating or the primary issue?
-
Oxygenation: Check PaO₂ and SaO₂ — is the patient hypoxemic?
Remember: ROME (Respiratory Opposite, Metabolic Equal) to quickly assess if the disturbance is respiratory or metabolic.
3. Match the ABG to the Clinical Picture
Ask yourself:
-
Does the ABG pattern fit what I’d expect for this patient?
-
Are they hypoventilating (CO₂ retention) or hyperventilating (blowing off CO₂)?
-
Could this be compensation or a mixed disorder?
For example:
-
COPD exacerbation → respiratory acidosis with possible metabolic compensation.
-
DKA → metabolic acidosis with compensatory respiratory alkalosis (Kussmaul respirations).
4. Prioritize Stabilization if Needed
If the patient scenario suggests severe hypoxemia or life-threatening acidosis/alkalosis, your first action should focus on stabilization:
-
Oxygen therapy
-
Non-invasive ventilation (e.g., BiPAP)
-
Mechanical ventilation (if needed)
-
Fluid resuscitation or medications (e.g., insulin for DKA)
Note: The exam may present choices that involve jumping straight to correcting acid-base numbers without stabilizing the patient—avoid this trap.
5. Beware of Common Exam Pitfalls
-
Treating the compensation instead of the primary issue
-
Missing oxygen-induced hypoventilation in CO₂ retainers
-
Choosing interventions without confirming ABG interpretation
-
Forgetting that not all hypoxemia needs maximum oxygen delivery (e.g., COPD patients)
Example Practice Question:
A 66-year-old male with a history of COPD presents with increased work of breathing and confusion. His ABG results are:
- pH: 7.29
- PaCO₂: 60 mmHg
- HCO₃⁻: 30 mEq/L
- PaO₂: 48 mmHg on room air
What is the most appropriate next step?
A. Intubate immediately
B. Administer oxygen via non-rebreather mask at 15 L/min
C. Start non-invasive ventilation (BiPAP) and titrate oxygen cautiously
D. Administer sodium bicarbonate IV push
Rationale: This is a case of acute-on-chronic respiratory acidosis with CO₂ retention and hypoxemia. COPD patients benefit from BiPAP and cautious oxygen therapy to avoid worsening hypercapnia. Intubation may be necessary if BiPAP fails, but it is not the first step here. Bicarbonate is not indicated in compensated respiratory acidosis.
Correct Answer: C. Start non-invasive ventilation (BiPAP) and titrate oxygen cautiously.
Exam Tip: Slow down. The exam isn’t testing how fast you can interpret the ABG—it’s testing your ability to make the right clinical decision based on the complete picture.
Final Thoughts
Interpreting ABGs and making the right clinical decisions doesn’t have to be overwhelming. The key is to stay systematic: interpret the results carefully, identify the true cause, stabilize the patient, select targeted treatments, and always reassess.
Instead of memorizing scattered facts, focus on understanding the “why” behind the “what.” The better you understand the physiology, the easier it becomes to make sound decisions—even under pressure.
Whether you’re preparing for the TMC, CSE, or standing at the bedside, remember: ABG interpretation isn’t just about getting the numbers right—it’s about making the right call for your patient. Stay curious, stay critical, and trust your process.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Castro D, Patil SM, Zubair M, et al. Arterial Blood Gas. [Updated 2024 Jan 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.