Fluid buildup in the lungs is a serious medical issue that can make breathing difficult and put strain on the heart and other organs. The medical term for this condition varies depending on the cause, such as pulmonary edema, pleural effusion, or pneumonia-related fluid. In all cases, the presence of excess fluid can impair oxygen exchange and endanger a patient’s health.
This article explains what causes fluid in the lungs, how doctors remove it, the treatments involved, and what patients can do during recovery.
Download our free guide that has over 100+ of the best tips for healthy lungs.
How to Get Fluid Out of the Lungs
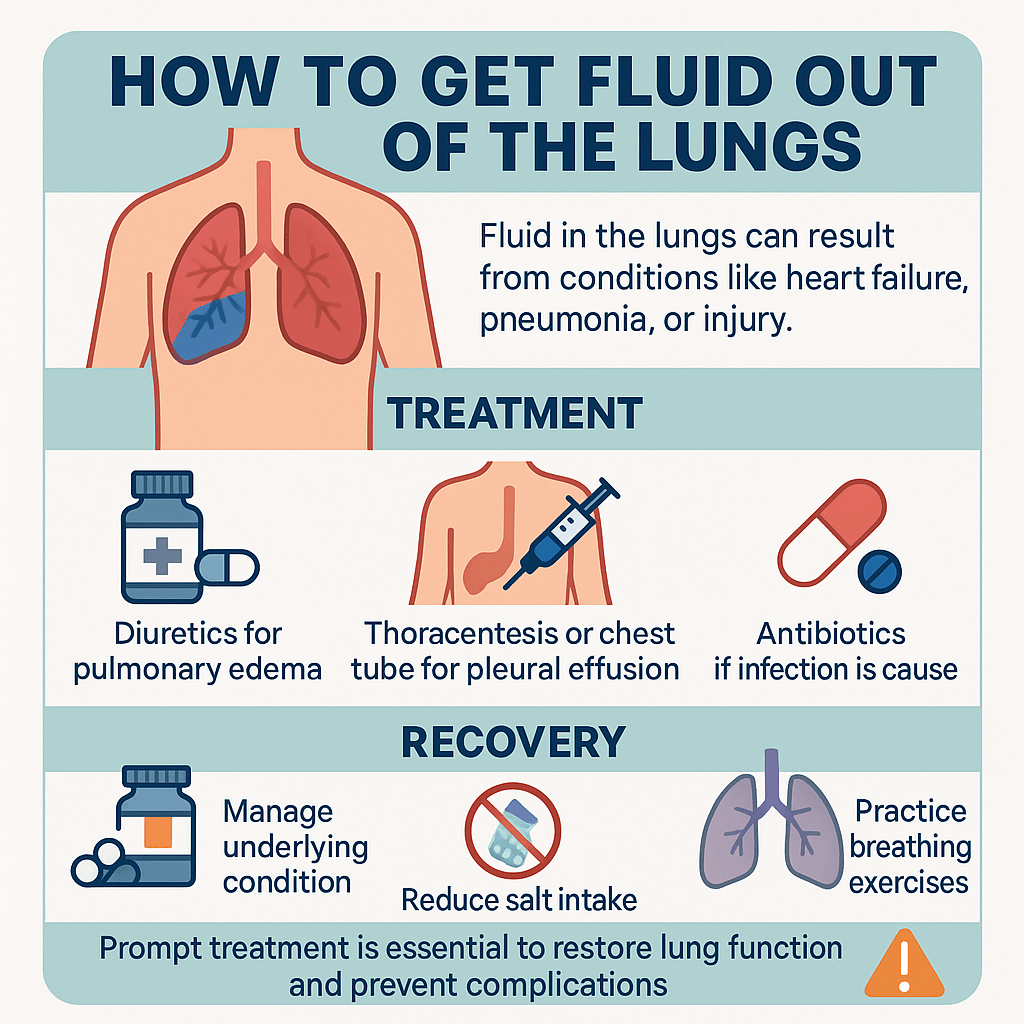
Fluid in the lungs can result from conditions like heart failure, pneumonia, or injury. Treatment depends on the cause and location of the fluid. For pulmonary edema, doctors often prescribe diuretics to help remove excess fluid through urination and may provide oxygen therapy. For pleural effusion, procedures like thoracentesis or chest tube drainage can physically remove the fluid.
Antibiotics are used if infection is the cause. Surgery may be needed for recurrent or complex cases. Recovery includes managing the underlying condition, following medication instructions, reducing salt intake, and practicing breathing exercises.
Prompt treatment is essential to restore lung function and prevent complications, so anyone with sudden shortness of breath or chest discomfort should seek medical care immediately.
Understanding Fluid in the Lungs
Fluid in the lungs disrupts normal breathing by filling spaces meant for air. It results from various medical conditions and presents with distinct symptoms that require prompt attention.
What Causes Fluid Accumulation
Fluid can accumulate in the lungs due to heart problems, infections, or injury. Heart failure is a common cause where the heart cannot pump blood efficiently, leading to fluid buildup in lung tissues.
Pneumonia or other infections cause inflammation, leading to fluid leakage into lung spaces. Kidney failure can also contribute by altering fluid balance in the body.
Trauma to the chest or exposure to toxic substances may result in pulmonary edema. In some cases, cancer or blood clots in the lungs block normal fluid drainage, causing accumulation.
Common Types of Pulmonary Fluid
There are two primary types of fluid in the lungs: pulmonary edema and pleural effusion. Pulmonary edema involves fluid leaking into the air sacs, affecting oxygen exchange. It is often related to heart failure or lung injury.
Pleural effusion is fluid collecting between the lungs and chest wall, usually caused by infections, cancer, or inflammation. This fluid is not inside the lungs but restricts their movement.
The nature of the fluid can be transudate (low protein, often from heart or kidney issues) or exudate (high protein, generally due to infection or inflammation). Identifying the type helps guide treatment.
Signs and Symptoms
Fluid in the lungs leads to shortness of breath, especially when lying down or during physical activity. Patients may experience persistent coughing, sometimes producing frothy or blood-tinged sputum.
Other symptoms include rapid breathing, chest pain, and fatigue. In severe cases, cyanosis (bluish lips or skin) can occur due to low oxygen levels. Listening with a stethoscope may reveal crackling sounds indicating fluid presence.
Diagnosing Fluid in the Lungs
Accurate diagnosis relies on a blend of physical assessments, imaging studies, and lab tests. These methods help identify the presence, amount, and possible causes of lung fluid buildup.
Physical Examination Techniques
The clinician begins with careful observation and auscultation of the chest. Listening with a stethoscope can detect crackling or bubbling sounds known as rales, commonly associated with fluid in the airspaces.
Percussion over the lung fields may reveal dullness where fluid accumulates, differentiating fluid leaks from air-filled spaces. Additionally, examination may include checking for signs like swelling, rapid breathing, and cyanosis, which can indicate fluid overload.
Pulse oximetry measures oxygen saturation, providing indirect evidence of impaired lung function. Vital signs, including heart rate and blood pressure, are also assessed to evaluate the patient’s overall status.
Imaging and Tests
Chest X-rays are the primary imaging tool, showing areas of haziness or whiteness where fluid has pooled. They can distinguish between pleural effusion and pulmonary edema.
Ultrasound may be used at the bedside to detect pleural fluid and guide drainage procedures. CT scans offer more detailed images if initial tests are inconclusive or if complications are suspected.
Laboratory tests include arterial blood gases to assess oxygen and carbon dioxide levels, indicating how well the lungs exchange gases. Blood tests may assess kidney and heart function, often involved in fluid retention.
Differentiating Related Conditions
Distinguishing lung fluid from other causes of respiratory symptoms is critical. For example, pneumonia can cause similar sounds but involves infection rather than fluid accumulation.
Heart failure often leads to pulmonary edema, so evaluating cardiac function via echocardiography helps clarify the cause. Pleural effusion must be differentiated from lung masses or infections by combining imaging with fluid sampling when possible.
Note: Correct diagnosis guides appropriate treatment, so ruling out these related conditions prevents delays in care.
Medical Treatments for Fluid Removal
Fluid buildup in the lungs requires targeted interventions to reduce swelling and improve breathing. Treatments focus on eliminating excess fluid, supporting oxygen levels, and directly draining accumulated fluid when necessary.
Diuretic Medications
Diuretics help the body remove excess fluid by increasing urine output. They are commonly prescribed for conditions like pulmonary edema caused by heart failure or kidney problems.
The most frequently used diuretics include furosemide and thiazides, which reduce fluid volume in lung tissues. Dosage is carefully adjusted based on the patient’s response and kidney function.
Patients may experience side effects such as electrolyte imbalances or dehydration. Close monitoring through blood tests is essential to ensure safety and effectiveness during treatment.
Oxygen Therapy
Oxygen therapy provides supplemental oxygen to improve blood oxygen levels when fluid impairs lung function. It may be delivered via nasal cannula, face mask, or more advanced devices, depending on the severity.
This therapy aids breathing, reduces shortness of breath, and supports vital organs. It does not remove fluid but helps alleviate symptoms while the underlying cause is treated.
Continuous or intermittent oxygen use is decided by the healthcare team, based on oxygen saturation and overall respiratory status.
Thoracentesis Procedure
Thoracentesis is a minimally invasive procedure to drain fluid directly from the pleural space around the lungs. It is often performed when fluid accumulation causes significant breathing difficulty or a diagnostic evaluation is needed.
Using ultrasound guidance, a needle is inserted between the ribs to withdraw fluid safely. The procedure typically takes 30 to 60 minutes.
Risks include infection, bleeding, or lung puncture, but are rare when performed by experienced clinicians. Fluid samples collected can be analyzed to determine the cause of the effusion.
At-Home Care and Lifestyle Adjustments
Effective management of fluid in the lungs involves careful observation of symptoms, smart dietary choices, and specific breathing techniques. Making these adjustments can support treatment and reduce discomfort.
Monitoring Symptoms
It is important to track changes in breathing, coughing, and fatigue regularly. Sudden worsening of symptoms such as increased shortness of breath, chest pain, or a bluish tint on the lips requires immediate medical attention.
Daily recording of symptoms, including the severity and duration, helps healthcare providers adjust treatment plans accurately. Using a pulse oximeter at home can assist in monitoring oxygen levels to detect early signs of distress.
Rest and avoid strenuous activity when symptoms worsen. Promptly reporting new or severe symptoms to a doctor can prevent complications.
Dietary Tips to Reduce Fluid Build-Up
Limiting salt intake is crucial, as sodium causes the body to retain fluid. Patients should avoid processed foods, canned soups, and salty snacks, focusing instead on fresh fruits and vegetables.
Drinking enough water is important, but fluid intake may need to be controlled based on a doctor’s advice to prevent overload. Eating smaller, more frequent meals can help reduce pressure on the lungs.
Foods rich in potassium, such as bananas and spinach, support fluid balance. Consulting a dietitian can provide personalized guidance for managing diet to reduce fluid retention.
Posture and Breathing Strategies
Maintaining an upright position, especially when resting or sleeping, helps ease breathing by allowing gravity to reduce fluid pooling in the lungs. Sitting up at a 45-degree angle is often recommended.
Deep, slow breathing exercises improve lung capacity and promote the expulsion of excess fluid. Techniques like pursed-lip breathing reduce the work of breathing and improve oxygen exchange.
Avoid lying flat for extended periods. Regularly changing positions and gentle mobility can prevent fluid accumulation and support lung function.
Preventing Recurrence of Pulmonary Fluid
Preventing fluid buildup in the lungs requires ongoing attention to health and careful monitoring. Addressing medical causes and maintaining consistent care are vital to reduce risk.
Managing Underlying Medical Conditions
Controlling diseases like heart failure, kidney disease, or pneumonia can help prevent lung fluid accumulation. Medications prescribed to manage these conditions must be taken exactly as directed.
Lifestyle changes such as reducing salt intake and managing blood pressure also support lung health. If heart failure is involved, optimizing cardiac function is essential to avoid fluid congestion.
Early treatment of infections and inflammation reduces complications that cause fluid buildup. Regular assessment of lung function can detect issues before they worsen.
Regular Medical Follow-Up
Consistent follow-up appointments ensure ongoing evaluation of lung health. Healthcare providers monitor symptoms, perform chest X-rays, and adjust treatment plans accordingly.
Routine tests like echocardiograms or blood work track the status of heart and kidney functions. Early identification of fluid recurrence allows prompt intervention.
Patients should report new or worsening symptoms immediately. Timely adjustments in medications or therapies can prevent hospitalization and reduce lung fluid risk.
Duration and Recovery
Recovery from fluid in the lungs varies depending on treatment type and individual health. It often requires ongoing medical care and monitoring to ensure lung function returns to normal.
Expected Recovery Time
The time to recover depends on the cause and severity of fluid accumulation. Mild cases treated with diuretics or medication may resolve within days to a few weeks.
More severe cases needing drainage through thoracentesis or chest tubes might take several weeks to months. Hospitalization is common for close observation and to manage complications.
Recovery involves improved breathing, reduced fluid levels on imaging, and better oxygen levels. Follow-up appointments are important to track progress and prevent recurrence.
Factors Affecting Prognosis
Underlying conditions like heart failure or kidney disease significantly influence outcomes. Effective management of these diseases improves recovery chances.
Age also plays a role; older patients often have slower healing. The extent of lung damage prior to fluid removal is critical for prognosis.
Prompt treatment initiation usually leads to better results. Delayed care can cause infections or permanent lung scarring, reducing lung capacity long-term.
FAQs About Removing Fluid From the Lungs
How Do You Clear Fluid From Your Lungs?
Clearing fluid from the lungs depends on its cause and location. For pulmonary edema, doctors may use diuretics to remove excess fluid via the kidneys and provide oxygen therapy to improve breathing. Pleural effusion may require drainage through thoracentesis or a chest tube.
Treating infections with antibiotics or addressing heart and kidney conditions is essential to prevent recurrence. In all cases, medical evaluation is critical, as untreated fluid can impair oxygen exchange and lead to serious, potentially life-threatening complications.
Can Fluid in the Lungs Go Away by Itself?
Whether fluid in the lungs goes away without treatment depends on the cause and severity. Mild cases related to minor infections or inflammation may resolve as the underlying issue heals. However, most cases—especially those due to heart failure, pneumonia, or cancer—require medical treatment to prevent worsening.
Without care, fluid buildup can compromise oxygen levels and cause dangerous complications. Even if symptoms seem to improve, it is important to have a doctor evaluate the condition to ensure it is fully resolved.
How Can I Get Fluid Out of My Lungs at Home?
Removing fluid from the lungs at home without medical intervention is not recommended, as this can be dangerous. While you can support recovery—such as taking prescribed medications, reducing salt intake, staying upright to improve breathing, and practicing gentle breathing exercises—these steps do not replace professional treatment.
Fluid buildup often requires medical procedures or prescription drugs to address the cause. If you suspect fluid in your lungs, seek medical attention immediately rather than attempting to manage it on your own.
What Helps Relieve Fluid in the Lungs?
Relieving fluid in the lungs typically involves treating the underlying cause. Doctors may prescribe diuretics for heart-related pulmonary edema, antibiotics for infections, or drainage procedures for pleural effusion. Supportive measures include oxygen therapy, maintaining an upright position to ease breathing, and following a low-sodium diet to prevent fluid retention.
While these treatments improve symptoms, addressing the root cause is essential to prevent recurrence. Medical evaluation is necessary to determine the safest and most effective approach for clearing the fluid and restoring lung function.
How Does Fluid Get Out of the Lungs With Pneumonia?
In pneumonia, fluid buildup occurs due to inflammation and infection in the lung tissue and alveoli. Treating pneumonia with antibiotics (for bacterial infections), antivirals, or antifungals allows the infection to resolve, reducing inflammation and enabling the body to reabsorb or expel the fluid.
Supportive care such as oxygen therapy, hydration, and breathing exercises can also help. As the infection clears, coughing often assists in moving fluid and mucus out of the lungs. Prompt treatment is key to preventing complications and restoring normal lung function.
How Do Doctors Get Fluid Out of the Lungs?
Doctors remove lung fluid based on its type and cause. For pulmonary edema, diuretics help the kidneys eliminate excess fluid. For pleural effusion, thoracentesis involves inserting a needle into the pleural space to drain fluid.
In more severe or recurrent cases, a chest tube may be placed for continuous drainage, or surgery may be performed. Infections are treated with antibiotics or other targeted medications. Throughout treatment, oxygen therapy may be used to maintain adequate oxygen levels until breathing improves.
When to See a Doctor for Fluid in the Lungs?
You should see a doctor immediately if you have sudden shortness of breath, chest pain, coughing up pink or frothy sputum, a rapid heartbeat, or signs of low oxygen, such as confusion or bluish lips or fingertips.
Even milder symptoms like persistent coughing, unexplained fatigue, or difficulty breathing when lying flat can indicate fluid buildup. Early medical evaluation helps identify the cause and prevents serious complications. Delaying treatment can lead to worsening breathing problems and, in severe cases, can be life-threatening.
Final Thoughts
Fluid accumulation in the lungs is a serious medical condition that requires prompt recognition and treatment. While the experience can be frightening for patients and families, understanding the condition, its causes, and available treatments can help reduce anxiety and improve outcomes.
The key to successful management lies in early detection, appropriate medical intervention, and ongoing management of underlying conditions. Patients should work closely with their healthcare providers to develop comprehensive treatment plans and should never hesitate to seek emergency care when symptoms worsen.
With proper medical care and adherence to treatment plans, many patients can successfully manage this condition and maintain a good quality of life.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Malek R, Soufi S. Pulmonary Edema. [Updated 2023 Apr 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.
- Krishna R, Antoine MH, Alahmadi MH, et al. Pleural Effusion. [Updated 2024 Aug 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.