In sudden cardiac emergencies, every second counts, and having the right tools available can mean the difference between life and death. One of the most important of these tools is the Automated External Defibrillator (AED)—a portable device designed to restore a normal heart rhythm in patients experiencing sudden cardiac arrest.
While AEDs are often associated with first responders and public access locations, they are also highly relevant in the field of respiratory care.
For respiratory therapists, understanding and using AEDs is essential, as respiratory and cardiac crises are closely linked, making rapid intervention a critical part of patient survival.
What is an AED?
An Automated External Defibrillator (AED) is a portable, life-saving medical device designed to analyze the heart’s rhythm and deliver an electrical shock, if necessary, to restore a normal rhythm during sudden cardiac arrest (SCA). These devices are user-friendly, providing visual and voice prompts that guide rescuers step-by-step through the process, even if they have no medical training.
By delivering defibrillation quickly, an AED can drastically increase survival rates in patients who experience life-threatening arrhythmias such as ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT).
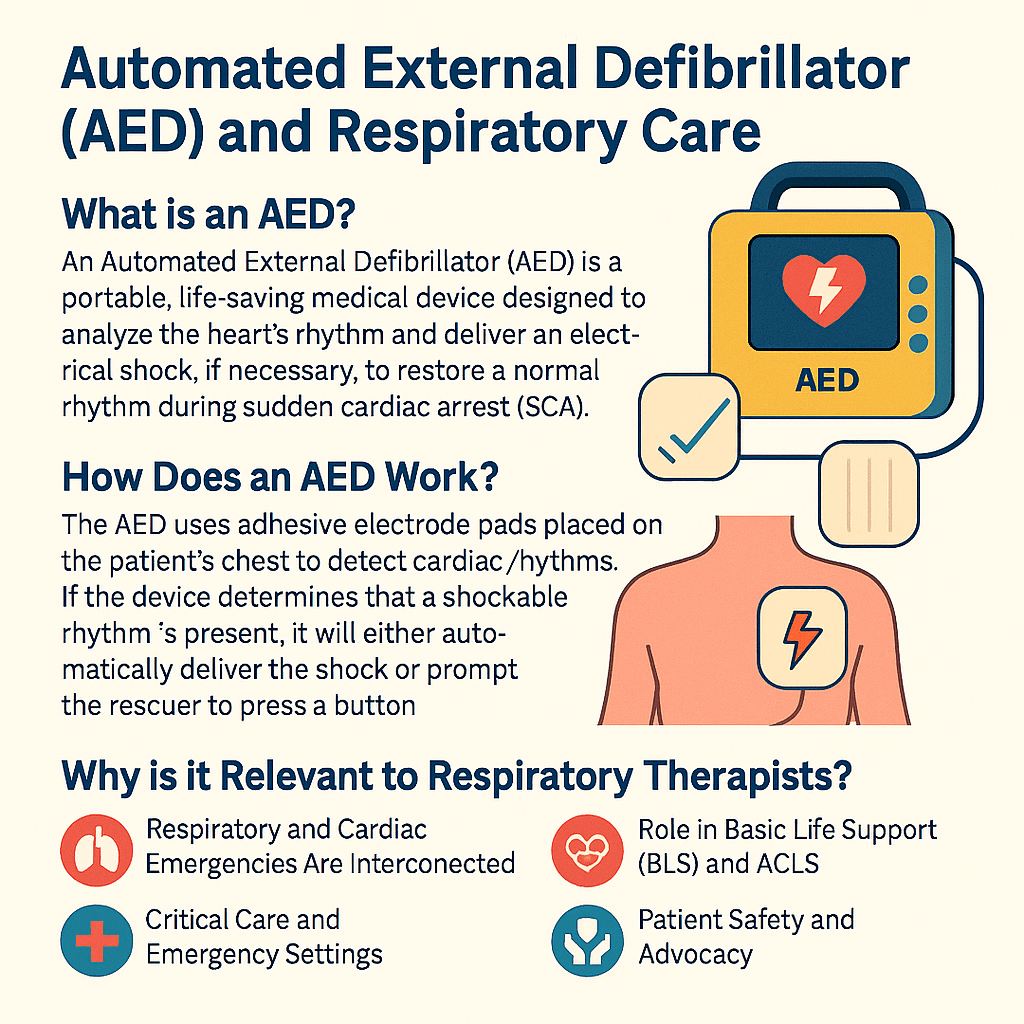
How Does an AED Work?
The AED uses adhesive electrode pads placed on the patient’s chest to detect cardiac rhythms. If the device determines that a shockable rhythm is present, it will either automatically deliver the shock or prompt the rescuer to press a button.
This shock depolarizes the heart muscle, interrupting the chaotic electrical activity and allowing the heart’s natural pacemaker to reestablish a normal rhythm.
The entire process takes only minutes and can mean the difference between life and death, as the likelihood of survival decreases by about 7–10% for every minute that defibrillation is delayed.
Why is it Relevant to Respiratory Therapists?
- Respiratory and Cardiac Emergencies Are Interconnected: Patients with severe respiratory compromise—such as hypoxemia, hypercapnia, or airway obstruction—are at increased risk of developing cardiac arrest. An RT who can quickly recognize this and apply an AED ensures continuity of life-saving care until advanced cardiac life support (ACLS) can be initiated.
- Critical Care and Emergency Settings: Respiratory therapists often work in intensive care units (ICUs), emergency departments, and during code blue situations. In these environments, rapid response to cardiac arrest is essential. AEDs provide RTs with the ability to act immediately, even in situations where advanced defibrillators may not be immediately available.
- Role in Basic Life Support (BLS) and ACLS: RTs are frequently certified in BLS and ACLS, both of which emphasize early defibrillation. Knowing how to use an AED is not just an expectation but a professional necessity.
- Patient Safety and Advocacy: As part of the healthcare team, RTs are patient advocates. Ensuring that AEDs are accessible, functional, and properly used contributes to a safer hospital and community environment.
Importance in the Field of Respiratory Care
AEDs reinforce the core mission of respiratory care: preserving and restoring life. Just as mechanical ventilators support breathing, AEDs support circulation in a cardiac emergency. Together, they represent two critical aspects of resuscitation—airway and breathing (managed by RTs) and circulation (supported by defibrillation).
Furthermore, respiratory therapists are increasingly involved in community education, teaching CPR and AED use to the public. This outreach extends the impact of respiratory care beyond the hospital walls, empowering communities to respond to emergencies effectively.
Automated External Defibrillator (AED) Practice Questions
1. What is the primary function of an Automated External Defibrillator (AED)?
It analyzes the heart’s rhythm and delivers an electrical shock to help restore an effective heartbeat.
2. When should an AED be used on a patient?
When the patient is unresponsive, not breathing, and has no detectable pulse.
3. Why should AED pads not be placed directly over a pacemaker or ICD?
Because it may interfere with the delivery of the electrical shock.
4. What must you do if the patient is in or near water before using an AED?
Move the patient to a dry area, remove wet clothing, dry the chest, then apply the AED pads.
5. How should transdermal medication patches be handled when using an AED?
Remove any patches with a gloved hand and never place AED pads directly on top of them.
6. What should be done if the patient has chest hair that interferes with AED pad placement?
Apply the pads, analyze the rhythm, and if there’s a pad error, rip them off to remove some hair, shave if needed, and reapply new pads.
7. Can AED pads be placed over body piercings or jewelry?
No, pads should be placed away from any metal jewelry or piercings, but the items do not need to be removed.
8. Through which chambers does the heart’s electrical signal travel?
From the atria (upper chambers) to the ventricles (lower chambers).
9. What happens when the heart’s electrical system is disrupted by damage?
It can cause an abnormal rhythm, stopping effective blood circulation.
10. What is cardiac arrest?
A condition where the heart stops beating or beats ineffectively, preventing blood flow to the brain and vital organs.
11. What are two main findings in cardiac arrest?
The heart has either stopped beating or has a chaotic rhythm like ventricular fibrillation.
12. What is ventricular fibrillation (V-Fib)?
A life-threatening abnormal rhythm where the ventricles quiver instead of contracting normally.
13. What are three key features of ventricular fibrillation?
Quivering ventricles, poor blood ejection, and chaotic electrical activity in the heart.
14. How is a heart attack defined?
Blockage of arteries and blood vessels supplying the heart.
15. What is the most common cause of cardiac arrest?
A heart attack.
16. What are common causes of V-Fib?
Heart attacks, electrocution, hypothermia, and trauma.
17. What is ventricular tachycardia (V-Tach)?
A rhythm where the ventricles contract too quickly, impairing blood flow.
18. Is ventricular tachycardia common, and what’s its effect?
It’s less common but prevents the heart from pumping blood effectively.
19. What is asystole?
A flatline—complete absence of electrical activity in the heart.
20. What does AED stand for, and what does it do?
Automated External Defibrillator; it analyzes the heart rhythm and delivers a shock if needed.
21. What is the minimum age and weight to use a standard AED?
Age 8 and up or over 55 pounds.
22. What is defibrillation?
An electrical shock used to interrupt abnormal heart rhythms and help restore normal heart function.
23. What are the four main steps in using an AED?
Turn on the AED, apply pads, allow rhythm analysis, and deliver shock if prompted.
24. What arrhythmia most commonly causes sudden cardiac arrest (SCA)?
Ventricular fibrillation (V-Fib).
25. How does an AED inform the user that a shock is required?
It uses voice prompts to guide when to deliver the shock.
26. AEDs are primarily used to treat which medical emergency?
Sudden cardiac arrest (SCA)
27. For every minute defibrillation is delayed during SCA, the chance of survival decreases by how much?
Approximately 10% per minute
28. True or False? An AED should never be used on a person who is receiving CPR.
False
29. What type of electrical issue in the heart often leads to abnormal rhythms?
Arrhythmias
30. True or False? Untrained bystanders can use an AED in an emergency situation.
True
31. How many reports of AEDs harming bystanders are reported nationwide each year?
None
32. What is SCA (sudden cardiac arrest)?
A condition where the heart unexpectedly stops beating, halting blood flow to vital organs.
33. Which two abnormal heart rhythms can lead to sudden cardiac arrest?
Ventricular fibrillation (V-Fib) and Ventricular tachycardia (V-Tach)
34. True or False? An AED works by delivering a shock to help restore a normal heart rhythm.
True
35. True or False? An AED might give a shock even if the heart is beating normally.
False
36. About what proportion of cardiac arrest victims require defibrillation due to fibrillation?
About 50%
37. How many AED pads must be correctly placed on a victim’s chest?
2 pads must be correctly positioned
38. What should you do if the AED advises a shock?
Ensure no one is touching the patient, then press the shock button when prompted
39. What is the next step after an AED delivers a shock?
Immediately resume CPR, starting with chest compressions
40. Name one scenario in which a young child might benefit from an AED.
Cardiac arrest from drowning or poisoning.
41. Where should AED pads be placed if the patient has an implanted pacemaker?
Several inches away from the pacemaker, never directly on it
42. What should be done if a medication patch is on the patient’s chest?
Remove the patch with a gloved hand before applying the AED pads
43. What happens to the heart during ventricular fibrillation?
The ventricles quiver instead of pumping blood effectively
44. When does an AED deliver a shock?
When the shock button is pressed after being prompted by the AED
45. What should you do before using an AED?
Confirm unresponsiveness, start CPR, place the AED next to the patient, and turn it on
46. How should AED pads be positioned on the chest?
Exactly as shown in the diagram on the AED unit
47. What must be avoided while the AED is analyzing heart rhythm?
Do not touch the victim
48. If the AED advises “No shock needed,” what is the next step?
Resume CPR, starting with chest compressions
49. What is the most common arrhythmia that an AED is used to treat?
Ventricular fibrillation (V-Fib)
50. What is the main purpose of defibrillation?
To stop abnormal heart rhythms and allow the heart to reset and beat normally
51. What type of AED pads should be used for a child between 1–8 years old?
Special pediatric pads
52. When assisting a victim of hypothermia with an AED, what is the correct action?
Handle the victim very carefully
53. AEDs are used to treat which life-threatening emergency?
Sudden cardiac arrest (SCA)
54. What is the most common arrhythmia that leads to sudden cardiac arrest?
Ventricular fibrillation (V-Fib)
55. When using an AED, what guides the user to deliver a shock if needed?
Voice prompts
56. Which two actions can significantly improve survival in someone experiencing SCA?
Using an AED and giving CPR
57. True or False? Untrained bystanders can use an AED to help save a life.
True
58. What is an AED?
A lightweight, portable device used to check heart rhythm and deliver a shock if needed
59. What is SCA (sudden cardiac arrest)?
A condition where the heart suddenly and unexpectedly stops beating
60. What are arrhythmias?
Problems that cause abnormal heart rhythms
61. What percentage of people who experience sudden cardiac arrest die from it?
95%
62. How many reports are there each year of AEDs delivering inappropriate shocks?
Zero
63. What is cardiac arrest?
A condition where the heart stops beating
64. How does a defibrillator work?
It delivers an electrical shock to clear abnormal activity and restore normal rhythm
65. What best describes the “chain of survival”?
Early access to help, Early CPR, Early defibrillation, Early advanced care
66. True or False? It is dangerous to attach an AED to a person who is breathing.
False
67. True or False? AED pads can be placed directly over clothing.
False
68. Why might an AED include a small towel?
To dry the chest of the casualty
69. What must be ensured before delivering a shock with an AED?
Everyone is clear of the casualty
70. True or False? You should not use an AED near flammable fumes or gases.
True
71. True or False? If you are alone, using an AED takes priority over starting CPR.
True
72. How should you check if an unconscious person is breathing?
Put your face near their nose or mouth
73. Which of the following is most correct regarding AED usability?
AEDs are generally pretty easy to use
74. What is the main difference between automatic and semi-automatic AEDs?
An automatic AED delivers the shock automatically; a semi-automatic prompts the user to push the button
75. What should you do if the unconscious person’s airway is blocked?
Clear the airway
76. Which of the following statements about AED pads is INCORRECT?
They’re both exactly the same
77. When checking for responsiveness in an adult, what should you do?
Try talking loudly and/or yell to get a response
78. Which of the following is true when using an AED on someone?
CPR should be performed in conjunction with AED use
79. What should you do if an AED advises that no shock is needed?
Check the airway and provide rescue breathing if the person is not breathing
80. Which of the following statements about AEDs is true?
They include instructions, often have voice prompts, and are user-friendly
81. What is the key difference between an automatic and a semi-automatic AED?
An automatic AED delivers the shock on its own; a semi-automatic requires user action to deliver the shock
82. If two people are available to help during a cardiac emergency, what should be done?
One person should use the AED while the other performs CPR
83. What is an AED primarily designed to do?
Restore a heart with an abnormal rhythm back to a normal rhythm
84. After the AED analyzes the heart rhythm, it will do all of the following EXCEPT:
Restart a stopped heart
85. When should emergency medical services be called for someone who collapses and is unresponsive?
Immediately or as soon as possible
86. If you are alone and a person needs both CPR and an AED, what should you do?
Alternate between using the AED and performing CPR
87. Which of the following is one of the two main types of AEDs?
Semi-automatic AED
88. What is a good source of information for finding AEDs in a building during an emergency?
A 911 operator
89. True or False: An AED is a portable device that diagnoses and treats life-threatening cardiac emergencies.
True
90. In which of the following situations would an AED NOT be helpful?
If someone’s heart has completely stopped beating
91. How do you check if an unconscious person is breathing?
Look for chest rise, listen for airflow, and feel for breath on your cheek
92. Which AED pad placement adjustment is appropriate in a wet environment?
Move the person to a dry area before applying the AED
93. Which of the following is true about AED pads?
Each pad has a diagram showing proper placement on the chest
94. How should you check responsiveness in an unconscious adult?
Shake or gently tap their shoulder and shout
95. What is the correct rate of chest compressions per minute in CPR?
100–120 compressions per minute
96. True or False: During an emergency, 911 may be able to tell you where an AED is located.
True
97. What is an AED programmed to do during a cardiac emergency?
Analyze the heart’s rhythm and deliver a shock if necessary
98. An AED would be helpful in all of the following situations EXCEPT:
If the heart has stopped beating with no electrical activity (asystole)
99. All of the following are true about using an AED EXCEPT:
They require certification to operate
100. What should you do immediately after delivering a shock with an AED?
Resume CPR, starting with chest compressions
Final Thoughts
The Automated External Defibrillator (AED) is more than just an emergency tool—it is a vital bridge between respiratory and cardiac life support. For respiratory therapists, proficiency with AEDs is essential, as respiratory failure and cardiac arrest are closely linked in clinical practice.
Whether in a hospital, clinic, or public setting, the ability to recognize a cardiac emergency and act swiftly with an AED can save lives. In the broader scope of respiratory care, AEDs underscore the therapist’s role as a frontline responder, educator, and patient advocate.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Liddle R, Davies CS, Colquhoun M, Handley AJ. ABC of resuscitation. The automated external defibrillator. BMJ. 2003.