A laryngoscope is one of the most important tools in airway management and critical care, allowing healthcare professionals to directly visualize the larynx and vocal cords. Most commonly used during endotracheal intubation, it helps secure the airway and ensure effective ventilation in patients who are unable to breathe on their own.
From emergency situations to routine surgical procedures, the laryngoscope has become an essential instrument in modern medicine.
For respiratory therapists in particular, understanding its function and mastering its use is vital, as it directly supports their role in maintaining and protecting the patient’s airway.
What is a Laryngoscope?
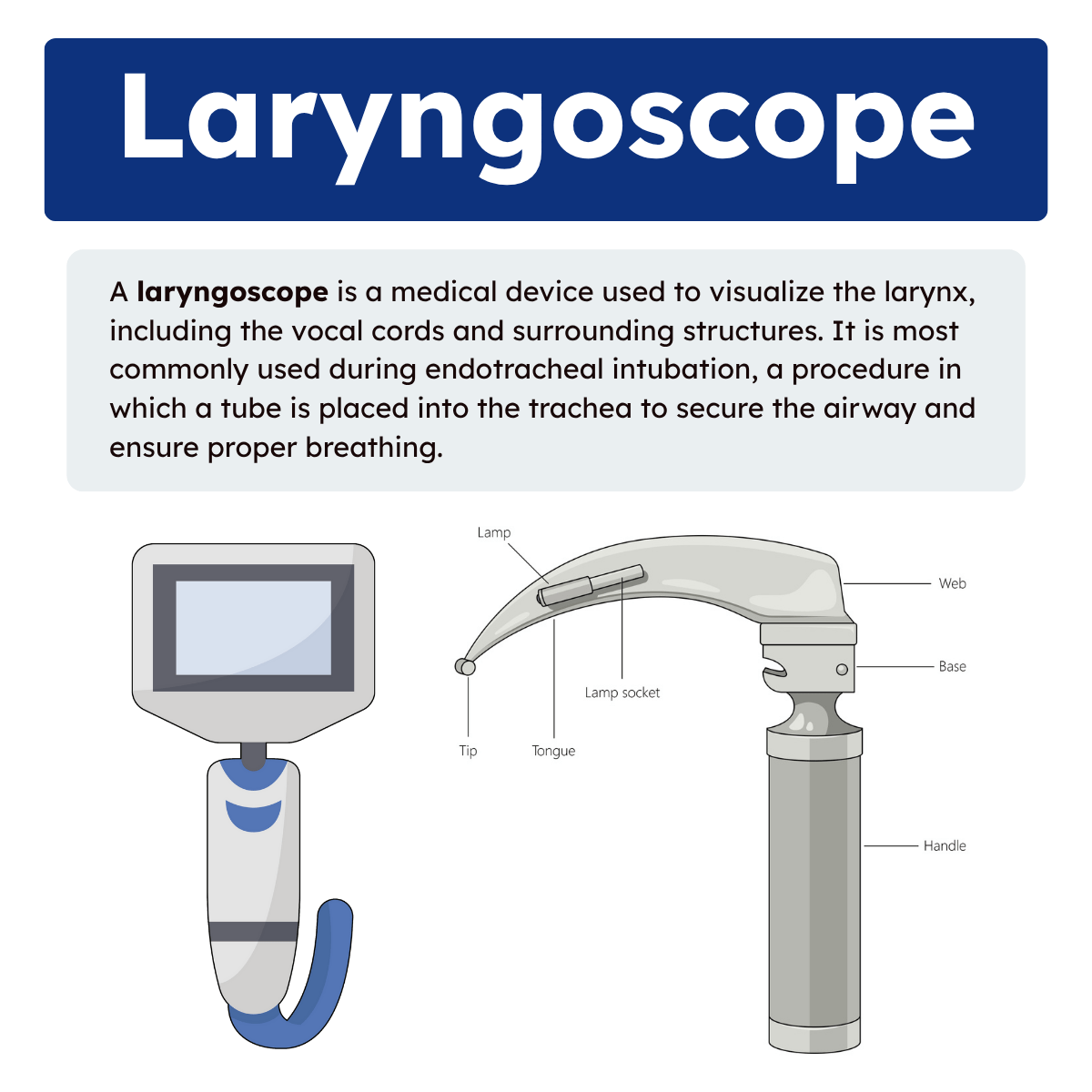
A laryngoscope is a medical device used to visualize the larynx, including the vocal cords and surrounding structures. It is most commonly used during endotracheal intubation, a procedure in which a tube is placed into the trachea to secure the airway and ensure proper breathing.
The instrument has two main components: a handle, which houses the power source for illumination, and a blade, which lifts the tongue and epiglottis for a clear view of the airway.
Blades come in various designs, with the Macintosh (curved) and Miller (straight) being the most widely used. Modern versions include video laryngoscopes, which provide enhanced visualization, making intubation easier and safer, especially in patients with difficult or compromised airways.
Parts of a Laryngoscope
The laryngoscope typically consists of two main parts:
- Handle – contains the power source, usually batteries or a rechargeable unit, that lights the blade.
- Blade – the part inserted into the patient’s mouth to lift the tongue and epiglottis, allowing direct visualization of the vocal cords. Blades come in different types, the most common being Macintosh (curved) and Miller (straight).
Types of Laryngoscope Blades
When it comes to direct laryngoscopy, the two most widely used blade types are the Macintosh and Miller. Each has unique features that make it better suited for certain patients and clinical scenarios.
The Macintosh blade is curved and designed to fit into the vallecula, the space just above the epiglottis. Lifting the epiglottis indirectly provides a clear view of the vocal cords. This blade is often preferred in adults because it offers good visualization while minimizing trauma to surrounding tissues.
In contrast, the Miller blade is straight and inserted beneath the epiglottis to lift it directly. This design is particularly useful in infants, small children, or patients with a floppy epiglottis, where indirect lifting may not provide an adequate view.
Note: Both blade types remain essential in respiratory care. Understanding when to use Macintosh versus Miller allows respiratory therapists and clinicians to optimize intubation success and patient safety.
Why is the Laryngoscope Relevant to Respiratory Therapists?
Airway management is one of the core responsibilities of respiratory therapists. Whether in an emergency department, intensive care unit, or during transport, ensuring that a patient’s airway remains open and secure is critical.
The laryngoscope plays a key role in this process by allowing RTs and other healthcare professionals to:
- Perform intubation during respiratory failure, cardiac arrest, or when mechanical ventilation is required.
- Assess airway anatomy in patients with suspected obstruction, trauma, or anatomical abnormalities.
- Assist in advanced procedures such as bronchoscopy or tracheostomy support.
Importance in Respiratory Care
For respiratory therapists, proficiency with a laryngoscope is not only a technical skill but also a life-saving competency. Quick and accurate intubation can mean the difference between effective ventilation and severe hypoxia. Additionally, as respiratory therapists often work alongside anesthesiologists, emergency physicians, and critical care teams, their expertise with airway equipment makes them invaluable in high-stakes scenarios.
The introduction of video laryngoscopy has further strengthened the respiratory therapist’s role in airway management. It reduces the risk of complications, improves success rates in difficult intubations, and provides teaching opportunities by allowing multiple clinicians to view the procedure simultaneously.
Laryngoscope Practice Questions
1. What is a laryngoscope?
A medical device used to visualize the larynx and vocal cords, most often during endotracheal intubation.
2. What are the two main components of a laryngoscope?
The handle (power source) and the blade (used to lift the tongue and epiglottis).
3. What is the primary function of the laryngoscope during intubation?
To provide a clear view of the airway for placement of an endotracheal tube.
4. What powers the light source of a traditional laryngoscope handle?
Batteries or a rechargeable unit.
5. What are the two most commonly used types of laryngoscope blades?
Macintosh (curved) and Miller (straight).
6. How does the Macintosh blade visualize the vocal cords?
By fitting into the vallecula and indirectly lifting the epiglottis.
7. Why is the Macintosh blade often preferred in adult patients?
It provides good visualization while minimizing trauma to airway tissues.
8. How does the Miller blade visualize the vocal cords?
By lifting the epiglottis directly.
9. In which patient population is the Miller blade particularly useful?
Infants, small children, or patients with a floppy epiglottis.
10. What is the role of a video laryngoscope?
It provides enhanced visualization through a camera, improving success in difficult intubations.
11. How does video laryngoscopy improve patient safety?
It increases intubation success rates and reduces complications in difficult airways.
12. Why is proficiency with the laryngoscope important for respiratory therapists?
It is a life-saving skill required for airway management in emergencies.
13. In which clinical scenarios is a laryngoscope most commonly used?
Respiratory failure, cardiac arrest, trauma, and when mechanical ventilation is required.
14. Besides intubation, what other purpose can a laryngoscope serve?
It can be used to assess airway anatomy for obstruction or trauma.
15. What is the clinical significance of the vallecula during Macintosh blade use?
It is the space above the epiglottis where the blade is positioned to lift indirectly.
16. Why is direct lifting of the epiglottis sometimes necessary?
Because indirect lifting may not provide adequate visualization, especially in children.
17. What advantage does video laryngoscopy provide for teaching?
It allows multiple clinicians to observe the airway view simultaneously.
18. Which healthcare professionals most commonly use laryngoscopes?
Respiratory therapists, anesthesiologists, emergency physicians, and critical care providers.
19. How can respiratory therapists assist in procedures involving the laryngoscope beyond intubation?
By providing airway visualization support in bronchoscopy or tracheostomy.
20. Why is quick and accurate laryngoscope use critical in respiratory care?
Because it can mean the difference between effective ventilation and severe hypoxia.
21. What is the primary purpose of a laryngoscope in airway management?
To improve visibility of the larynx during endotracheal tube placement.
22. What are the three main parts of a laryngoscope?
The handle, the blade, and the light source.
23. What is the function of the handle on a laryngoscope?
It houses the power source, usually batteries, for illumination.
24. What is the function of the blade on a laryngoscope?
It depresses the tongue and epiglottis to expose the vocal cords.
25. What is the function of the light source on a laryngoscope?
To illuminate the airway for visualization during intubation.
26. Small animal or neonatal laryngoscope blades are available in sizes ranging from what to what?
From size 0 (smallest) to size 5 (largest).
27. Large animal or specialty laryngoscope blades may measure up to how many inches in length?
Up to 18 inches.
28. What are the two most commonly used types of laryngoscope blades?
Miller (straight) and Macintosh (curved).
29. Which type of laryngoscope blade is straight and lifts the epiglottis directly?
The Miller blade.
30. Which type of laryngoscope blade is curved and lifts the epiglottis indirectly via the vallecula?
The Macintosh blade.
31. What are the four general handle sizes available for laryngoscopes?
Large, medium, stubby, and penlite (mini).
32. Which laryngoscope handle sizes are most commonly used in adults?
Large and medium
33. In which patients is a stubby handle often preferred?
Patients with thick necks, obesity, or in labor and delivery settings.
34. In which patient population is a penlite (mini) handle most often used?
Pediatrics
35. Laryngoscopes may come with or without what additional feature?
A fiber-optic light source.
36. Where may the fiber-optic light source be located on a laryngoscope?
In the handle or in the blade.
37. What color feature often distinguishes fiber-optic handles?
They typically have a green connection system.
38. What color are most laryngoscope blades with an integrated light source?
Silver
39. What are laryngoscope blades used for during intubation?
To visualize the larynx and guide endotracheal tube placement.
40. Are laryngoscope blades reusable, disposable, or both?
They can be either reusable or disposable.
41. What is the most widely used straight laryngoscope blade?
The Miller blade.
42. What special design feature does the Miller blade have to minimize trauma?
A reduced flange on the side of the blade.
43. What feature of the Miller blade helps lift the epiglottis?
Its extended and slightly curved tip.
44. Why is the Miller blade often used in difficult airways?
It provides greater exposure of the larynx by directly lifting the epiglottis.
45. What size Miller blade is commonly used for neonates?
Size 0
46. What size Miller blade is typically used for infants?
Size 1
47. What size Miller blade is typically used for children?
Size 2
48. What size Miller blade is typically used for teenagers and adults?
Size 3
49. What size Miller blade is typically used for large adults?
Size 4
50. What complication may occur if an endotracheal tube is accidentally placed in the esophagus instead of the trachea?
The patient may aspirate gastric contents.
51. True or False: Laryngoscopy can be performed for either direct or indirect visualization of the larynx.
True
52. What is indirect laryngoscopy, and when is it commonly used?
It uses a laryngeal mirror in the awake patient’s mouth to visualize the larynx and may be used for biopsy or polyp excision.
53. What is direct laryngoscopy?
A procedure performed under local or general anesthesia in which a laryngoscope is passed over the tongue to expose the vocal cords.
54. Which laryngoscope blade is curved and designed to fit into the vallecula?
The Macintosh blade.
55. Which laryngoscope blade is straight and directly lifts the epiglottis?
The Miller blade.
56. Besides Macintosh and Miller, what are two other less common laryngoscope blade types?
The Phillips blade and the Wisconsin blade.
57. How many sizes are Miller blades available in, and which patients are they suited for?
Five sizes (0–4), suited for neonates through large adults.
58. How should a Miller blade be held during intubation?
In the left hand.
59. What is the main design feature of the Macintosh blade?
It is curved and designed for indirect lifting of the epiglottis.
60. What is the most common error when using a Macintosh blade?
Selecting a blade that is too small.
61. What is a rigid laryngoscope?
A non-flexible laryngoscope used to directly visualize the vocal cords during intubation.
62. What is the most common type of intubation using a laryngoscope?
Oral intubation
63. Why is patient positioning important during oral intubation?
Proper positioning aligns airway structures, improving the view and increasing the chance of successful intubation.
64. What is the ideal head position for intubation with a laryngoscope?
The sniffing position, which aligns the pharyngeal and laryngeal axes.
65. How should the patient’s mouth be opened for laryngoscopy?
By using the right hand in a scissor technique: thumb on the lower teeth/jaw and index finger on the upper teeth/jaw.
66. How should a Macintosh blade be inserted and positioned?
Insert from the right side, sweep the tongue left, and place the tip in the vallecula.
67. Why should you avoid inserting a Macintosh blade in the center of the mouth?
The tongue may herniate around the blade, obstructing the view.
68. Where should the tip of the Miller blade be positioned during laryngoscopy?
Beneath the epiglottis to lift it directly, being careful not to advance too deep.
69. What is the purpose of applying cricoid pressure (Sellick’s maneuver) during laryngoscopy?
To reduce the risk of gastric aspiration by compressing the esophagus.
70. Which laryngoscope blade is often preferred for patients with limited mouth opening?
The straight Miller blade.
71. Why is it important to avoid placing the laryngoscope blade on the patient’s teeth?
To prevent dental trauma, especially in the upper incisors.
72. What is the primary advantage of video laryngoscopes in emergency airway management?
They improve visualization in patients with difficult or distorted airways.
73. Which feature of a laryngoscope handle helps clinicians identify whether it is fiber-optic compatible?
A green standard marking on the handle.
74. What does the Mallampati classification assess?
The ratio of tongue size to the oral cavity to predict ease of intubation.
75. What is nasal intubation, and when might it be used?
A method of intubation through the nasal passage, often used when oral intubation is not feasible.
76. What is the gold standard for confirming proper endotracheal tube placement?
Capnography (end-tidal CO₂ monitoring).
77. Besides capnography, what are other methods to verify proper tube placement?
Observation of bilateral chest rise, auscultation, tube depth markings, pulse oximetry, bronchoscopy, and chest X-ray.
78. What ancillary equipment is often required during laryngoscopy and intubation?
Magill forceps (for nasal intubation), suction, tooth protectors, and a stylet.
79. What is rapid-sequence induction (RSI)?
A method of securing the airway quickly with pre-oxygenation and immediate intubation, minimizing aspiration risk.
80. What are key preparation steps for RSI before intubation?
Pre-oxygenate with 100% O₂ for 3–5 minutes, prepare airway equipment and suction, ensure a stylet is in the tube, and have an assistant apply cricoid pressure (Sellick’s maneuver).
81. What is the primary purpose of a laryngoscope during airway management?
To visualize the larynx and guide endotracheal tube placement.
82. Which type of laryngoscope provides an indirect, video-assisted view of the vocal cords?
Video laryngoscope
83. How does video laryngoscopy improve success in difficult airways compared to direct laryngoscopy?
It provides a magnified, indirect view of the glottis without requiring alignment of oral, pharyngeal, and laryngeal axes.
84. What is the main power source used in modern laryngoscope handles?
Rechargeable batteries or disposable batteries.
85. Why is illumination important in laryngoscopy?
It allows clear visualization of airway structures such as the epiglottis and vocal cords.
86. What size Macintosh blade is typically used for average adult patients?
Size 3
87. Which laryngoscope blade type is generally preferred for neonates and infants?
The Miller (straight) blade.
88. Why might a stubby laryngoscope handle be preferred in obese patients?
It provides better maneuverability in patients with large chests or thick necks.
89. What is the role of the flange on a laryngoscope blade?
To help sweep the tongue to the side during insertion.
90. What complication can occur if the laryngoscope blade is inserted too deeply?
Esophageal visualization or trauma to airway structures.
91. In which clinical situation is nasal fiberoptic laryngoscopy especially useful?
When oral intubation is not possible, such as with maxillofacial trauma.
92. What does a “Grade IV” view on the Cormack–Lehane scale indicate?
No laryngeal structures are visible.
93. Why should laryngoscope blades always be checked before use?
To confirm secure attachment, adequate light, and absence of damage.
94. Which intubation adjunct is often used with a laryngoscope to guide the tube into the trachea?
A stylet or bougie
95. What is the main advantage of disposable laryngoscope blades?
They reduce infection risk by eliminating the need for sterilization.
96. What positioning aid may improve visualization during laryngoscopy in obese patients?
A ramped position using blankets or pillows to align the ear with the sternal notch.
97. Why is the “sniffing position” recommended for most adult laryngoscopies?
It aligns the oral, pharyngeal, and laryngeal axes for optimal visualization.
98. What is the risk of using excessive force with a laryngoscope blade?
Dental trauma or soft tissue injury.
99. Which blade type is most effective for patients with a floppy epiglottis?
The Miller blade
100. What training benefit does video laryngoscopy offer in education?
It allows instructors and learners to view the airway simultaneously for teaching and feedback.
Final Thoughts
The laryngoscope is a fundamental tool in airway management, providing clinicians with a direct view of the larynx to support safe and effective intubation. Both Macintosh and Miller blades serve important roles, with each design suited to different patient needs and clinical situations.
For respiratory therapists, understanding how and when to use these blades is an essential part of their role in maintaining the airway. With the addition of video laryngoscopy, the tool has become even more versatile, reinforcing its continued importance in modern respiratory care.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Peterson K, Ginglen JG, Desai NM, et al. Direct Laryngoscopy. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.

