Beta-2 agonists play a vital role in treating respiratory conditions marked by airway obstruction or bronchoconstriction. Commonly used in patients with asthma, COPD, and related disorders, these bronchodilators help restore airflow and ease breathing.
For respiratory therapists, a solid grasp of how beta-2 agonists function, when they are indicated, and how to monitor their effects is essential for providing safe, effective, and timely care across both acute and chronic care settings.
Take our free course to learn essential pharmacology tips, insights, and strategies to pass the TMC Exam on your first (or next) attempt.
What Are Beta-2 Agonists?
Beta-2 agonists are bronchodilator medications that target beta-2 adrenergic receptors in the smooth muscles of the airways. When these receptors are stimulated, the airway muscles relax, resulting in bronchodilation (i.e., widening of the air passages), which improves airflow and eases breathing. These medications are commonly used to treat respiratory conditions such as asthma, chronic obstructive pulmonary disease (COPD), and bronchospasm.
Beta-2 agonists are typically delivered via inhalers or nebulizers and are categorized into short-acting and long-acting types, depending on their duration of action. Their fast and targeted effects make them essential in both emergency and maintenance respiratory therapy.
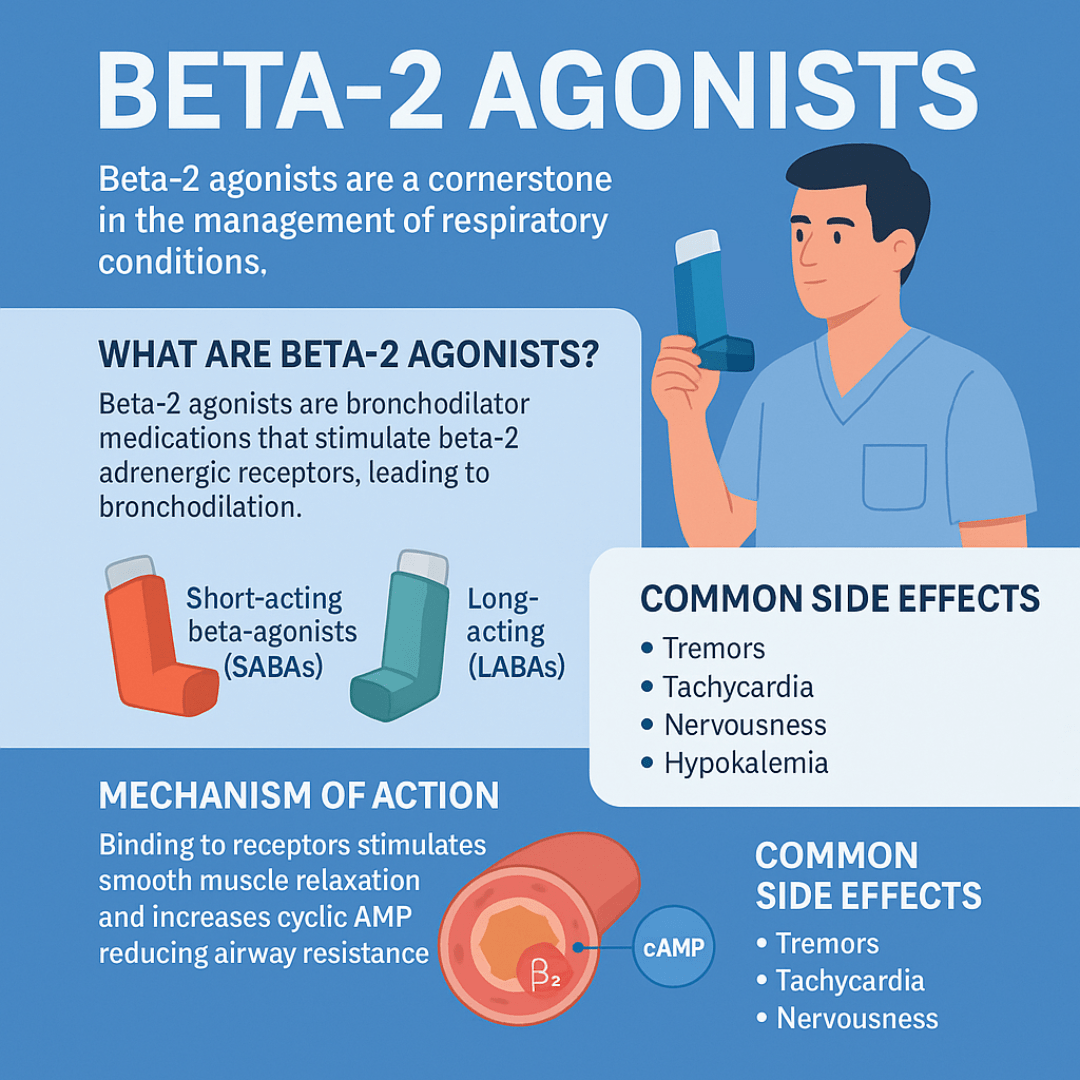
Mechanism of Action
Beta-2 agonists bind to the beta-2 adrenergic receptors primarily located in the bronchial smooth muscle. This binding activates adenylate cyclase, which increases cyclic AMP (cAMP) levels. Elevated cAMP leads to smooth muscle relaxation and inhibition of inflammatory mediator release from mast cells. The result is reduced airway resistance and improved airflow.
Clinical Applications
Beta-2 agonists are used in a variety of clinical settings, including:
- Emergency care: SABAs are the first-line treatment for acute asthma exacerbations and bronchospasm in COPD.
- Chronic management: LABAs are often prescribed alongside inhaled corticosteroids (ICS) for long-term control of asthma and COPD.
- Pre-treatment for procedures: Beta-2 agonists may be administered before exercise or bronchoprovocation testing to prevent induced bronchospasm.
Types of Beta-2 Agonists
Beta-2 agonists are generally classified based on how quickly they act and how long their effects last. This classification helps guide their use in both emergency and maintenance settings.
1. Short-Acting Beta-Agonists (SABAs)
These medications provide rapid relief from acute bronchospasm by relaxing airway smooth muscles within minutes. They are commonly referred to as “rescue inhalers” due to their fast onset of action. SABAs typically last for 4–6 hours.
Examples include:
- Albuterol (Salbutamol) – the most widely used SABA
- Levalbuterol – a more selective isomer of albuterol with potentially fewer side effects
Note: SABAs are used during asthma attacks, before exercise to prevent exercise-induced bronchospasm, and in other acute respiratory situations.
2. Long-Acting Beta-Agonists (LABAs)
LABAs offer extended bronchodilation, usually lasting 12 hours or more. Unlike SABAs, they are not used for quick relief but are taken on a regular schedule to maintain open airways over time.
Examples include:
- Salmeterol – often used in combination with inhaled corticosteroids
- Formoterol – has a quicker onset than salmeterol but a similar duration
- Arformoterol – a derivative of formoterol, often used in nebulized form for COPD
Note: LABAs are particularly beneficial for patients with moderate to severe asthma or COPD, but they must be used carefully, especially in asthma, because using LABAs without a corticosteroid can increase the risk of severe exacerbations.
3. Ultra-Long-Acting Beta-Agonists (ULABAs)
These newer agents offer 24-hour bronchodilation and are primarily used in the treatment of COPD. They are not approved for asthma in many regions due to safety concerns.
Examples include:
- Indacaterol
- Olodaterol
- Vilanterol (often combined with other agents like fluticasone or umeclidinium)
Note: Understanding the type and duration of each beta-2 agonist is crucial for tailoring treatment plans to individual patient needs and ensuring safe, effective care.
Why Beta-2 Agonists Are Relevant in Respiratory Care
For respiratory therapists, beta-2 agonists are among the most frequently administered medications. Their rapid action and direct impact on airway patency make them essential tools in both acute and chronic care settings.
RTs are responsible not only for delivering these medications, often via nebulizer or metered-dose inhaler (MDI), but also for assessing their effectiveness and monitoring for side effects.
Understanding the pharmacodynamics and proper delivery techniques ensures that patients receive maximum benefit from their treatment. Additionally, therapists must educate patients on proper inhaler use, recognize signs of overuse or diminished response, and participate in decisions regarding escalation or de-escalation of therapy.
Common Side Effects
While beta-2 agonists are widely used and generally considered safe, they are not without potential side effects, particularly when administered in high doses or over extended periods. Most adverse effects result from the stimulation of beta receptors in tissues beyond the lungs, especially the cardiovascular and nervous systems.
Some of the most commonly reported side effects include:
- Tremors: Fine muscle tremors, especially in the hands, are one of the most frequently observed effects. This is due to beta-2 receptor stimulation in skeletal muscle.
- Tachycardia: An increased heart rate may occur as a result of both beta-2 and incidental beta-1 receptor activation, particularly at higher doses.
- Nervousness or anxiety: Patients may experience a jittery or restless feeling shortly after inhalation, especially when using short-acting agents.
- Hypokalemia: Prolonged or repeated use, especially with continuous nebulization, can lower potassium levels, potentially leading to muscle weakness or arrhythmias.
- Palpitations: Sensations of a racing or pounding heart may be distressing to some patients and should be monitored, especially in those with a cardiac history.
These side effects are typically mild and transient but can become clinically significant in vulnerable populations, such as critically ill patients or those with underlying heart conditions.
Note: It is essential for respiratory therapists to closely monitor patients receiving beta-2 agonists, particularly when high doses or continuous administration are involved. Regular assessment of heart rate, blood pressure, serum potassium levels, and patient symptoms can help prevent complications and ensure safe, effective treatment.
Beta-2 Agonists Practice Questions
1. What is the primary indication for administering beta-2 agonists?
To prevent or relieve bronchospasms associated with asthma, bronchitis, or other pulmonary diseases
2. What is the mechanism of action of beta-2 agonists?
They stimulate beta-2 adrenergic receptors in bronchial smooth muscle, resulting in bronchodilation
3. What are common adverse effects associated with beta-2 agonist use?
Tachycardia, angina, and tremors
4. In which clinical scenario is levalbuterol preferred over albuterol?
When the patient experiences tachycardia or is sensitive to albuterol-induced tachycardia
5. What are some contraindications for using beta-2 agonists?
Tachycardia, uncontrolled diabetes, hypertension, angina, heart disease, and hyperthyroidism
6. Which of the following are examples of beta-2 agonists?
Albuterol, levalbuterol, formoterol, and salmeterol
7. What is a primary indication for long-acting beta-2 agonists (LABAs)?
To provide maintenance therapy and prevent exacerbations in patients with COPD
8. Which medication is classified as a long-acting beta-2 agonist used in asthma and COPD?
Salmeterol
9. In which situation is albuterol commonly used as a rescue medication?
During acute asthma attacks due to its rapid onset of bronchodilation.
10. What is an appropriate use of salmeterol in respiratory care?
For daily control of severe persistent asthma when combined with an inhaled corticosteroid
11. Which of the following is a short-acting beta-2 agonist used for quick relief of bronchospasm?
Albuterol
12. What is the indication for the short-acting beta-2 agonist terbutaline?
Asthma, due to its fast-acting bronchodilatory effects within 15 minutes, lasting up to 6 hours
13. What is the primary action of beta-2 adrenergic agonists?
They promote bronchodilation by activating beta-2 receptors in bronchial smooth muscle
14. Which beta-2 agonist is classified as a short-acting inhaled medication used for acute bronchospasm?
Albuterol
15. What is the onset and duration of action for the long-acting beta-2 agonist formoterol?
Onset: 1 to 3 minutes; Duration: approximately 10 hours
16. How often should salmeterol be used for long-term asthma control?
Every 12 hours; it should not be used more frequently.
17. What is a unique, nonlabeled use for the beta-2 agonist terbutaline?
It may be used off-label for the management of preterm labor
18. Which patient condition is contraindicated with beta-2 agonist use?
Tachydysrhythmias
19. What medication class may reduce the effectiveness of beta-2 agonists?
Beta blockers
20. Which drug interaction increases the effects of beta-2 agonists and may raise the risk of side effects?
Monoamine oxidase inhibitors (MAOIs)
21. What are the common side effects of beta-2 agonist medications?
Tachycardia, palpitations, and tremors
22. What is the therapeutic role of salmeterol in asthma management?
It is used as a long-acting bronchodilator for daily asthma control, not for acute relief
23. What is the key therapeutic use of beta-2 agonists?
To provide long-term control and prevention of asthma symptoms
24. How do beta-2 agonists help relieve bronchospasm?
By stimulating beta-2 receptors, causing smooth muscle relaxation and bronchodilation
25. What cardiovascular adverse effects may result from beta-2 agonist use?
Tachycardia, palpitations, and angina
26. What effect can beta-2 agonists have on blood glucose levels?
They may increase blood glucose levels, requiring dosage adjustments for diabetic patients
27. What patient education should be provided regarding tremors caused by beta-2 agonists?
Monitor tremors and report them to a healthcare provider if persistent or worsening
28. Why should patients with cardiac disease use beta-2 agonists with caution?
Because these medications can exacerbate heart-related symptoms such as tachycardia or angina
29. What is the recommended timing of albuterol use in relation to steroid inhalers?
Albuterol should be used first to open the airways before using inhaled corticosteroids
30. Why is salmeterol not appropriate for acute asthma symptom relief?
Because it has a delayed onset and is intended for maintenance therapy, not emergency use
31. What is the primary mechanism of action for beta-2 adrenergic agonists?
They stimulate beta-2 receptors in bronchial smooth muscle, causing bronchodilation and improved airflow.
32. Why is the mechanism of beta-2 agonists especially important in treating asthma?
It directly relaxes airway muscles, helping to relieve bronchospasm and improve breathing.
33. What is albuterol primarily indicated for?
Acute asthma attacks and as a pre-treatment before inhaled corticosteroids
34. What is salmeterol used for?
Long-term control of asthma symptoms and prevention of exercise-induced bronchospasm
35. Which of the following medications is NOT used for acute relief of asthma symptoms?
Salmeterol
36. What is a common mnemonic to remember the side effects of albuterol?
“Tossing & Turning” — referring to tachycardia, tremors, and insomnia
37. Why should patients avoid using NSAIDs and beta blockers while taking beta-2 agonists?
Because they can reduce the effectiveness of beta-2 agonists
38. What should a patient do before using an albuterol inhaler?
Shake the inhaler well to ensure proper medication delivery.
39. If a patient uses albuterol three times with no relief, what should they do next?
Notify their healthcare provider immediately.
40. How often should salmeterol be taken?
Every 12 hours, with a maximum of two doses per day
41. What is an expected indicator that beta-2 agonist therapy is working?
A decreased respiratory rate and oxygen saturation ≥ 90%
42. Why is it important to monitor respiratory rate and oxygen saturation when using beta-2 agonists?
To assess treatment effectiveness and monitor the patient’s respiratory status
43. What is the correct sequence for using a bronchodilator and a steroid inhaler?
Use the bronchodilator (e.g., albuterol) first, then the steroid after 5 minutes.
44. Why should patients rinse their mouth after using a steroid inhaler but not after using albuterol?
To prevent oral thrush, which can result from steroid use, but not from beta-2 agonists
45. What is the primary difference between short-acting and long-acting beta-2 agonists?
Short-acting agents provide rapid relief during acute episodes, while long-acting agents are for maintenance.
46. What respiratory conditions are beta-2 agonists commonly used to treat?
Asthma and chronic obstructive pulmonary disease (COPD)
47. What are the two main categories of beta-2 agonist medications?
Short-acting and long-acting
48. What is albuterol classified as?
A short-acting beta-2 adrenergic agonist and bronchodilator
49. What is the therapeutic effect of albuterol in asthma management?
It relieves bronchospasm and reduces airway resistance.
50. What is the drug of choice for fast symptom relief in asthma?
Short-acting inhaled beta-2 agonists such as albuterol.
51. Which type of medication should NOT be taken with beta-2 adrenergic agonists?
Beta-adrenergic blockers
52. What is a serious but rare adverse reaction to beta-2 agonist use?
Paradoxical bronchospasm
53. Which of the following is a common cardiovascular side effect of beta-2 agonists?
Tachycardia and palpitations
54. What are some nervous system-related side effects of beta-2 agonists?
Nervousness, anxiety, and tremors
55. What patient teaching should be included regarding inhaler technique during an acute asthma attack?
Exhale fully, compress the chamber, inhale deeply, and hold the breath.
56. What side effects may patients commonly experience after using albuterol?
Increased heart rate and jitteriness
57. What lifestyle modifications should be suggested to patients using beta-2 agonists?
Increase fluid intake and avoid caffeine to reduce jittery side effects.
58. What is the onset time of action for inhaled albuterol?
Approximately 5 minutes
59. How long does the effect of inhaled albuterol typically last?
About 4 to 6 hours
60. What is the preferred route of administration for beta-2 agonists during an acute asthma attack?
Inhalation via metered-dose inhaler or nebulizer
61. Why is the inhaled route preferred for beta-2 agonists?
It delivers the drug directly to the lungs, providing faster and more targeted relief.
62. Which beta-2 agonist is sometimes used off-label to delay premature labor?
Terbutaline
63. Why must beta-2 agonists be used with caution in patients with diabetes?
They can increase blood glucose levels.
64. How can beta-2 agonists affect potassium levels?
They may cause hypokalemia by shifting potassium into cells.
65. Which symptom may indicate overuse or toxicity of beta-2 agonists?
Severe tremors and persistent tachycardia
66. Why are long-acting beta-2 agonists (LABAs) not used alone in asthma treatment?
Because they do not treat acute symptoms and may increase the risk of asthma-related death without an inhaled corticosteroid.
67. What is the black box warning associated with salmeterol?
Increased risk of asthma-related death if used without a corticosteroid
68. What is the clinical significance of combining LABAs with inhaled corticosteroids (ICS)?
It provides both bronchodilation and inflammation control for long-term asthma management.
69. What type of patient should avoid oral beta-2 agonists due to systemic side effects?
Patients with cardiac disease or hypertension
70. How should the effectiveness of beta-2 agonist therapy be evaluated?
Improvement in peak expiratory flow rate (PEFR) and reduced wheezing
71. What should a patient do if symptoms persist after using a beta-2 agonist inhaler?
Seek medical attention promptly.
72. What is a common sign that a patient is developing tolerance to beta-2 agonists?
Decreased effectiveness in relieving bronchospasm
73. Can beta-2 agonists be used prophylactically before exercise?
Yes, especially short-acting types like albuterol to prevent exercise-induced bronchospasm.
74. What respiratory rate trend suggests a beta-2 agonist is working effectively?
A decrease in respiratory rate toward the normal range
75. What cardiac condition is a contraindication for beta-2 agonist use?
Uncontrolled tachyarrhythmias
76. Why should patients avoid caffeine while using beta-2 agonists?
Caffeine can worsen side effects like jitteriness and palpitations.
77. What is the role of beta-2 agonists in COPD management?
They reduce airway resistance and improve airflow in chronic bronchitis and emphysema.
78. Which formulation of beta-2 agonist is used for long-term maintenance therapy in COPD?
Inhaled long-acting beta-2 agonists like formoterol or salmeterol
79. How should beta-2 agonists be stored to maintain potency?
At room temperature, away from heat and direct sunlight
80. What is the expected change in oxygen saturation after beta-2 agonist use?
An increase in SpO2 levels due to improved ventilation and oxygen exchange
81. What is the primary benefit of using beta-2 agonists in bronchial asthma?
They relieve bronchospasm by relaxing bronchial smooth muscle.
82. Why is levalbuterol considered more selective than albuterol?
It contains only the R-enantiomer, which is more active and has fewer side effects.
83. What is the maximum recommended daily usage of salmeterol?
Two inhalations every 12 hours
84. How do beta-2 agonists affect mucociliary clearance?
They enhance ciliary movement, improving mucus clearance from the airways.
85. Which beta-2 agonist is most commonly used in metered-dose inhalers (MDIs)?
Albuterol
86. In what setting is continuous nebulization of albuterol most commonly used?
Severe asthma exacerbation in emergency or critical care settings
87. Why should patients be advised to use a spacer with their beta-2 agonist inhaler?
To improve drug deposition in the lungs and reduce oropharyngeal side effects
88. What is the typical pediatric dose of albuterol via nebulizer?
2.5 mg every 4–6 hours as needed
89. How does formoterol differ from salmeterol in the onset of action?
Formoterol has a faster onset, around 1 to 3 minutes.
90. Which class of medications may antagonize the effects of beta-2 agonists?
Non-selective beta-blockers (e.g., propranolol)
91. What symptom should be reported immediately when using beta-2 agonists?
Chest pain or palpitations
92. What condition may result from excessive beta-2 agonist use due to stimulation of Na+/K+ pumps?
Hypokalemia
93. How are long-acting beta-2 agonists typically scheduled in asthma management?
Taken twice daily at regular intervals, not as needed
94. Why is salmeterol not appropriate for acute asthma attacks?
Its delayed onset makes it ineffective for immediate symptom relief.
95. What should a patient do immediately after using a beta-2 agonist inhaler without symptom relief?
Wait 20 minutes, then repeat a dose if prescribed; if still no relief, seek medical help.
96. Why might beta-2 agonists be less effective in smokers?
Chronic inflammation and airway remodeling can reduce receptor sensitivity.
97. What non-respiratory condition may terbutaline be used for?
Prevention of premature labor due to uterine smooth muscle relaxation.
98. What patient education is essential when starting a beta-2 agonist?
Understand dosage limits and proper inhaler technique to avoid overuse.
99. What is a key difference in receptor selectivity between beta-1 and beta-2 agonists?
Beta-2 agonists primarily target the lungs, while beta-1 agonists affect the heart.
100. Which condition requires caution when prescribing beta-2 agonists due to the risk of arrhythmia?
Hyperthyroidism
Final Thoughts
Beta-2 agonists are vital medications in the arsenal of respiratory care, offering quick and effective relief of bronchospasm and supporting long-term disease management.
For respiratory therapists, a deep understanding of these drugs—their pharmacology, delivery methods, indications, and potential complications—is crucial for optimizing patient outcomes and ensuring safe, effective care.
As frontline providers in pulmonary medicine, RTs play a key role in the administration and monitoring of beta-2 agonist therapy in diverse clinical settings.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Hsu E, Bajaj T. Beta2-Agonists. [Updated 2023 Jun 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.