Bilevel positive airway pressure (BiPAP) is a form of noninvasive ventilatory support that delivers two levels of pressure to help patients breathe more effectively. It plays a critical role in the management of various respiratory conditions, especially those that cause hypoventilation or obstructive breathing patterns.
For respiratory therapists and healthcare professionals, understanding how BiPAP works—and when to use it—is essential to providing effective care to patients in both acute and chronic settings.
Take our free course to master the basics of mechanical ventilation with clear explanations and helpful practice questions.
What is BiPAP?
BiPAP is a type of noninvasive positive pressure ventilation (NPPV) that provides two different levels of airway pressure:
- Inspiratory Positive Airway Pressure (IPAP): Applied during the inhalation phase, IPAP supports the patient’s breathing effort and increases the tidal volume delivered. It functions similarly to the peak airway pressure in traditional mechanical ventilation. Adjusting the IPAP setting directly affects the volume of air the patient inhales with each breath.
- Expiratory Positive Airway Pressure (EPAP): Applied during the exhalation phase, EPAP helps keep the airways open and improves oxygenation. It operates similarly to positive end-expiratory pressure (PEEP) in traditional mechanical ventilation. Increasing the EPAP setting enhances the patient’s oxygenation by maintaining positive pressure at the end of expiration.
This dual-pressure approach helps patients take in adequate air during inhalation while preventing airway collapse during exhalation.
Unlike continuous positive airway pressure (CPAP), which delivers a single continuous pressure, BiPAP offers greater flexibility and support, especially for patients with ventilatory failure or those who cannot tolerate the constant pressure of CPAP.
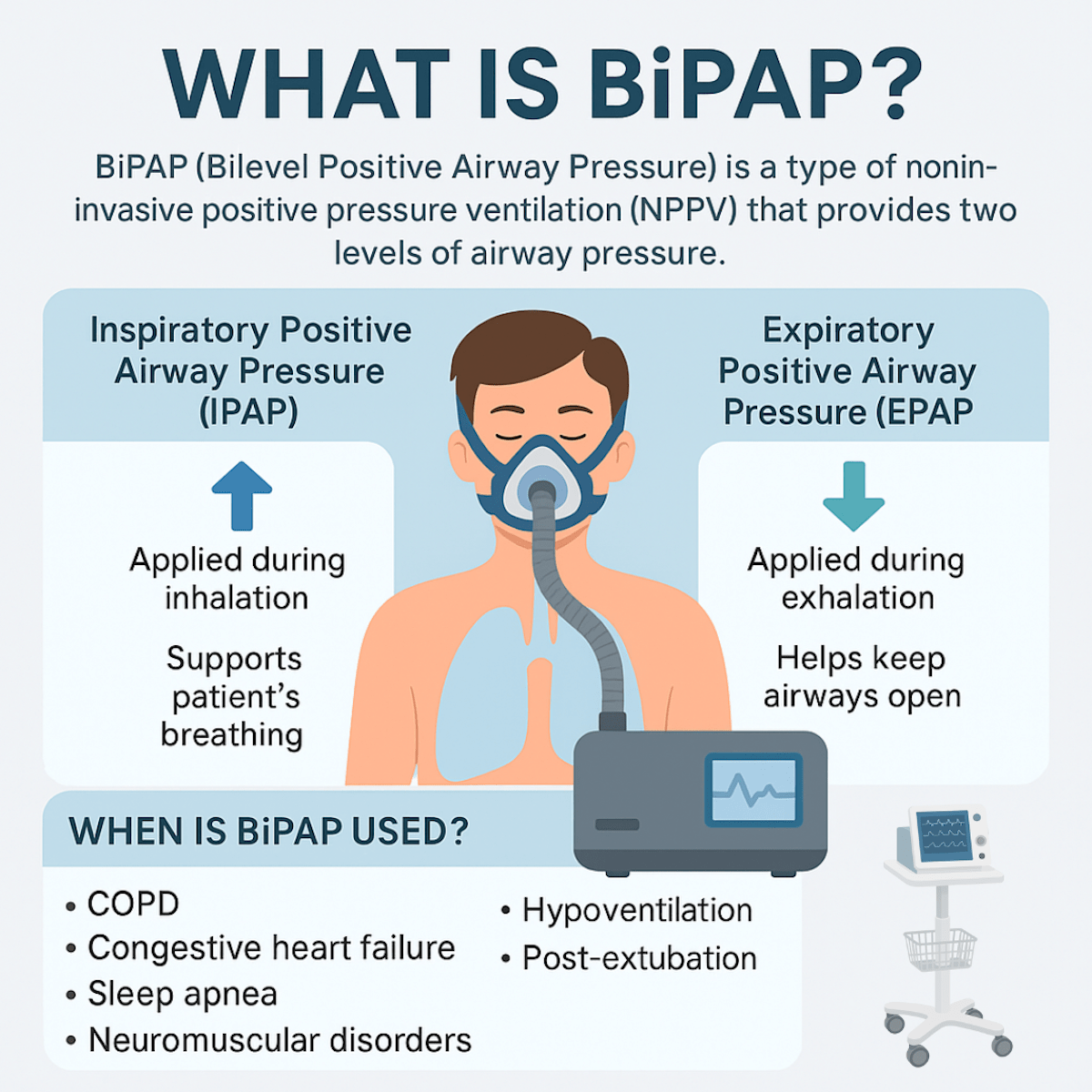
When is BiPAP Used?
BiPAP is commonly indicated for patients with:
- Chronic obstructive pulmonary disease (COPD) exacerbations
- Congestive heart failure (CHF) with pulmonary edema
- Obstructive sleep apnea (OSA) with high pressure needs or poor CPAP tolerance
- Neuromuscular disorders like ALS or muscular dystrophy
- Hypoventilation syndromes
- Post-extubation support in high-risk patients
- COVID-19 and other acute respiratory infections with hypoxemic or hypercapnic respiratory failure (in select, carefully monitored cases)
Why is BiPAP Important in Respiratory Care?
For respiratory therapists, BiPAP is a powerful tool that can prevent intubation, improve gas exchange, and reduce the length of hospital stays when used appropriately. It’s particularly beneficial in managing acute-on-chronic respiratory failure, a common issue in patients with advanced COPD.
By assisting with ventilation, BiPAP helps decrease the patient’s work of breathing, stabilize their blood gases, and often improve their comfort and compliance with treatment.
RTs are responsible for setting the appropriate pressures, monitoring patient tolerance and response, and troubleshooting common issues such as air leaks, skin breakdown, or mask discomfort. Understanding the physiology behind IPAP and EPAP helps in customizing therapy for individual needs.
Key Responsibilities for Respiratory Therapists
- Initiating and titrating BiPAP settings
- Monitoring ABG results and vital signs
- Educating patients on device use and mask fit
- Recognizing when BiPAP is failing and escalation to invasive ventilation is needed
- Ensuring proper interface selection and humidification to enhance patient comfort
BiPAP Practice Questions
1. What does BiPAP stand for, and what is its primary purpose?
BiPAP stands for bilevel positive airway pressure and is used to improve ventilation by providing two levels of pressure to support breathing.
2. How does BiPAP differ from CPAP therapy?
BiPAP delivers two levels of pressure (IPAP and EPAP), while CPAP provides a single continuous pressure throughout the breathing cycle.
3. What does IPAP stand for, and what is its clinical role in BiPAP therapy?
IPAP, or Inspiratory Positive Airway Pressure, helps reduce hypoxemia and/or hypercapnia by assisting with inhalation.
4. What is a typical pressure range for IPAP?
2–30 cmH₂O
5. What does EPAP stand for, and how does it assist breathing?
EPAP, or Expiratory Positive Airway Pressure, helps maintain airway patency and functional residual capacity during exhalation.
6. What is a common pressure range for EPAP?
2–20 cmH₂O
7. What is a key indication for using BiPAP in patients with COPD?
To prevent intubation by providing ventilatory support in cases of chronic respiratory failure.
8. How are IPAP and EPAP adjusted during titration?
IPAP is increased above EPAP in 2.5 cmH₂O increments based on apnea or hypopnea; EPAP is increased if events persist.
9. When would you increase IPAP without adjusting EPAP?
For issues such as snoring, arousals, or non-apneic oxygen desaturation.
10. How can BiPAP be used as CPAP?
By setting IPAP and EPAP to the same pressure level.
11. In Spontaneous mode, how does the BiPAP device operate?
It detects the patient’s inspiratory effort and delivers a breath in response.
12. What additional feature does Spontaneous-Timed (ST) mode include?
A backup respiratory rate that delivers breaths if the patient becomes apneic.
13. In Timed mode, what determines the breath rate?
A set respiratory rate determined by the machine, independent of patient effort.
14. What is the function of inspiratory time in BiPAP’s Timed mode?
It determines the duration of inspiration based on either a percentage of the respiratory cycle or a fixed time.
15. What does an Auto-Titrating BiPAP device do?
Automatically adjusts pressures throughout the night in response to changes in airway resistance.
16. What is the purpose of the Ramp Pressure setting?
Gradually increases pressure over time to enhance comfort as the patient falls asleep.
17. What is the typical ramp duration for BiPAP devices?
5–45 minutes, with 1–3 cmH₂O pressure increments.
18. What should be done before starting a BiPAP or CPAP therapy session?
Ensure a proper mask fit, attach the circuit, and start with low pressures while coaching the patient on breathing.
19. How soon should an ABG be checked after initiating BiPAP?
Within 1 hour of starting therapy.
20. What is a key advantage of NPPV over invasive ventilation?
It enables patients to communicate and eat orally while receiving respiratory support.
21. What are three common indications for Noninvasive Positive Pressure Ventilation?
COPD exacerbation, acute cardiogenic pulmonary edema, and acute hypoxemic respiratory failure.
22. What criteria suggest a patient may benefit from NPPV in acute care?
Respiratory rate >25, pH <7.35, and PaCO₂ >45 mmHg with respiratory distress.
23. How does BiPAP assist in managing failed extubation?
It supports alveolar ventilation and reduces the work of breathing post-extubation.
24. What is a hazard of using noninvasive ventilation?
Aspiration pneumonia due to improper mask fit or reduced consciousness.
25. What should be assessed if the patient’s CO₂ remains elevated during BiPAP?
Ensure FiO₂ is not too high and target oxygen saturation around 90%.
26. What can cause rebreathing of CO₂ during BiPAP therapy?
Inadequate exhalation port function or low EPAP pressure.
27. If alveolar ventilation is inadequate, what BiPAP adjustment is indicated?
Increase IPAP to deliver higher tidal volumes.
28. What should be done if oxygenation is low but PaCO₂ has improved?
Increase FiO₂ or consider increasing IPAP to improve oxygenation.
29. What is a common cause of excessive air leak during BiPAP?
Poor mask fit, missing dentures, or circuit disconnection.
30. What is a precaution when using BiPAP in preload-sensitive patients?
Ensure intravascular volume is adequate to avoid hypotension.
31. If the patient is becoming confused or agitated during BiPAP, what should be done?
Draw an ABG to evaluate for worsening hypercapnia and reassess therapy.
32. What does the use of abdominal muscles during inspiration suggest?
Inappropriate pressure settings or excessive leak; reduce IPAP if tidal volume is adequate.
33. What should be done to prevent pressure sores from the BiPAP mask?
Regularly check skin integrity and use barrier products, such as Duoderm.
34. What is a recommended intervention for gastric distention during BiPAP use?
Insert a nasogastric (NG) tube to relieve pressure.
35. What causes eye irritation during BiPAP therapy?
Excessive air leaks from the mask, requiring adjustment.
36. What is a solution for dry secretions during BiPAP therapy?
Add a heated humidifier to the circuit.
37. What type of mask is best for claustrophobic patients?
Nasal mask
38. What type of BiPAP interface increases the risk of aspiration?
Full face mask
39. What is a total face mask?
A hard acrylic mask that covers the entire face with an inflatable seal.
40. What is the benefit of nasal pillows as an interface?
They are inserted into the nares and are minimally invasive.
41. When should BiPAP be the first-line therapy over CPAP?
In patients with hypercapnic respiratory failure and increased work of breathing.
42. When is CPAP preferred over BiPAP?
In patients with pulmonary edema and hypoxemia without hypercarbia.
43. What does the early application of BiPAP during cardiogenic pulmonary edema help achieve?
Faster improvement in oxygenation, CO₂ levels, and reduced risk of intubation.
44. What is one limitation of current research regarding BiPAP outcomes?
The effect of BiPAP on long-term clinical outcomes remains inconclusive.
45. What is one goal of titrating BiPAP in sleep-disordered breathing?
To reduce apneas, hypopneas, and desaturation events.
46. How does EPAP help in treating obstructive events?
It splints the airway open during expiration to prevent collapse.
47. What is one possible complication from excessive BiPAP pressures?
Barotrauma, such as pneumothorax
48. What is the difference between Spontaneous and Timed modes in BiPAP?
Spontaneous mode relies on patient effort; Timed mode uses preset intervals regardless of effort.
49. What should be done if the patient is showing signs of respiratory fatigue despite BiPAP?
Consider transitioning to invasive mechanical ventilation.
50. What is the role of BiPAP in DNR/DNI patients with respiratory failure?
It provides supportive care to relieve dyspnea without invasive intubation.
51. Why must a BiPAP or CPAP system deliver up to 80–100 L/min of inspiratory flow?
To prevent airway pressure from dropping during the respiratory cycle and ensure patient comfort.
52. What is a critical step during the initiation of noninvasive respiratory support?
Clear, timely, and detailed communication with the patient about the treatment plan.
53. What is the recommended PEEP level for CPAP therapy?
Start low and slowly increase to 8–12 cm H₂O based on patient tolerance.
54. What is the typical PEEP level range for BiPAP therapy?
6–8 cm H₂O during BiPAP based on clinical need and tolerance.
55. What is the target tidal volume when titrating pressure support in BiPAP?
6–7 mL/kg of ideal body weight.
56. When might NPPV be used following extubation?
To alleviate shortness of breath in patients with chronic respiratory needs or during weaning.
57. How can NPPV benefit patients receiving comfort-focused care?
By reducing the work of breathing and improving respiratory comfort at end-of-life.
58. What is a key consideration when using NPPV for palliative purposes?
Clarifying that the goal is comfort, not recovery, to align care with patient values.
59. How can NPPV improve end-of-life communication for patients?
It may help patients maintain alertness and the ability to speak during their final moments.
60. Why is patient comfort crucial when adjusting BiPAP or CPAP settings?
To ensure that NPPV provides relief rather than becoming a burden to the patient.
61. What is essential during terminal weaning from a mechanical ventilator?
Ongoing, transparent communication with the patient’s family throughout the process.
62. What is the primary goal of CPAP therapy?
To improve oxygenation by applying continuous positive airway pressure.
63. What is the primary goal of BiPAP therapy?
To support both oxygenation and ventilation with separate pressures.
64. Which settings can be adjusted on a BiPAP device?
IPAP, EPAP, respiratory rate, inspiratory time, rise time, FiO₂, and pressure support.
65. What does IPAP stand for and control?
Inspiratory Positive Airway Pressure; it improves ventilation and tidal volume.
66. What is the function of IPAP in BiPAP therapy?
It increases tidal volume and reduces carbon dioxide levels.
67. What does EPAP stand for and control?
Expiratory Positive Airway Pressure; it helps improve oxygenation.
68. How does EPAP enhance oxygenation?
By increasing functional residual capacity and preventing alveolar collapse.
69. What does RR stand for, and how is it used in BiPAP?
Respiratory rate; it is monitored and set below the patient’s spontaneous breathing rate.
70. Why should the set RR on BiPAP be lower than the patient’s spontaneous rate?
To encourage spontaneous breathing and patient-ventilator synchrony.
71. What is I-time, and when is it used?
Inspiratory time; it may be adjusted to improve oxygenation in critical cases.
72. What can decreasing I-time lead to in BiPAP settings?
It may create an inverse I:E ratio and improve oxygenation temporarily.
73. What can increasing I-time potentially cause?
Air trapping, especially in patients with obstructive lung disease.
74. What is the purpose of the rise time in BiPAP settings?
To enhance patient comfort by controlling the speed of pressure rise during inspiration.
75. What is FiO₂, and what does it control?
Fraction of inspired oxygen; it adjusts the oxygen concentration delivered to the patient.
76. What does pressure support refer to in BiPAP therapy?
The difference between IPAP and EPAP; it determines the level of ventilatory support.
77. How is pressure support calculated on a BiPAP machine?
Pressure Support = IPAP – EPAP
78. What is the “60/60 rule” in oxygenation assessment?
PaO₂ > 60 mmHg on an FiO₂ < 60% suggests adequate oxygenation.
79. When should you switch from adjusting FiO₂ to adjusting EPAP on BiPAP?
When the FiO₂ is greater than 60% and oxygenation is still inadequate.
80. What noninvasive device is appropriate for a patient with asthma?
CPAP is recommended to help keep the airways open during bronchoconstriction.
81. What noninvasive device is preferred for a patient with CHF?
CPAP, as it helps reduce preload and improve oxygenation in pulmonary edema.
82. What noninvasive device is best for a patient with COPD?
BiPAP, as it supports both oxygenation and ventilation by assisting with CO₂ clearance.
83. What does AVAPS stand for in ventilatory support?
Average Volume Assured Pressure Support.
84. What are the key settings in AVAPS?
Target tidal volume, PEEP, respiratory rate, and FiO₂.
85. What does PRVC stand for?
Pressure Regulated Volume Control.
86. Why is CPAP the first-line noninvasive mode for asthma exacerbations?
It helps keep airways open during bronchoconstriction by providing continuous pressure.
87. True or False: Increasing BiPAP from 10/5 to 12/7 increases pressure support.
False – pressure support remains the same at 5 cmH₂O.
88. True or False: Inspiratory time can be adjusted as a last resort for oxygenation.
True – increasing I-time can improve oxygenation by prolonging inspiratory phase.
89. If a patient’s primary issue is ventilation, which BiPAP setting should be adjusted?
IPAP – to increase tidal volume and improve CO₂ clearance.
90. What initial setting would you use for an asthmatic patient with SpO₂ of 86% on NRB?
CPAP at 6 cmH₂O with 100% FiO₂.
91. A patient on BiPAP 10/5 complains of too much pressure. What adjustment may improve comfort?
Increase the rise time to slow the delivery of inspiratory pressure.
92. A patient on CPAP 5 and FiO₂ 60% has ABG 7.38/42/55/23. What should you do?
Increase CPAP to improve oxygenation.
93. What are the two primary pressures set in BiPAP therapy?
IPAP and EPAP.
94. What is IPAP and its purpose?
Inspiratory Positive Airway Pressure – used to improve ventilation.
95. What is EPAP and its purpose?
Expiratory Positive Airway Pressure – used to enhance oxygenation.
96. Which patient conditions are commonly treated with BiPAP?
COPD, CHF, sleep apnea, pulmonary hypertension, IPF, ALS.
97. What are the therapeutic goals of BiPAP use?
Reduce work of breathing, lower CO₂, improve sleep and comfort.
98. What is a key limitation of BiPAP therapy?
It is not intended for life-sustaining respiratory support.
99. What should you check if there’s a large leak from a BiPAP setup?
Inspect and adjust mask, tubing, or device for proper fit or damage.
100. Can oxygen be used with BiPAP therapy?
Yes, oxygen can be bled into the system through a bleed-in valve.
101. How does BiPAP assist with breathing?
By alternating pressures to reduce CO₂ and improve oxygenation.
102. How is an appropriate tidal volume calculated for BiPAP?
Ideal Body Weight (kg) × 5–8 mL per breath.
103. What is tidal volume in BiPAP therapy?
The volume of air delivered per breath, measured in mL or L.
104. Are standard BiPAP settings used for all patients?
No, settings must be tailored, but minimum is typically 10/5 cmH₂O.
105. What are contraindications for BiPAP use?
Apnea, altered consciousness, facial trauma, and inability to protect the airway.
106. What are common indications for BiPAP in acute care?
Hypercapnia with pH 7.20–7.35, hypoxia on FiO₂ >60%, COPD, CHF, OHS.
107. Name two complications of BiPAP therapy.
Aspiration and skin breakdown from mask pressure.
108. Why is skin breakdown a concern with BiPAP masks?
Prolonged pressure can cause ulcers, especially in immobile patients.
109. What tool is used to assess skin integrity in BiPAP patients?
Braden Scale.
110. What are typical initial BiPAP settings?
10/5 or 12/6 cmH₂O.
111. How is pressure support (PSV) calculated in BiPAP?
PSV = IPAP – EPAP.
112. If a patient has low pH and high PaCO₂, what changes should be made?
Increase IPAP to enhance ventilation and reduce CO₂.
113. What is ramp in BiPAP therapy?
The time over which the pressure gradually increases to set levels.
114. What is C-Flex used for?
To provide pressure relief during exhalation in CPAP therapy.
115. Name two common BiPAP machines used in clinical settings.
V60 and Vision.
116. Which BiPAP machine is used for transport?
V60.
117. Can BiPAP be used for a DNR patient?
Yes, for comfort care until the patient becomes unresponsive or ALOC occurs.
118. Can BiPAP be used for a DNI patient?
Yes, especially in reversible conditions like CHF or COPD exacerbations.
119. What is a key requirement for a patient to use CPAP or BiPAP effectively?
The patient must be able to breathe spontaneously on their own.
120. What are the three primary benefits of positive airway pressure therapy?
It maintains airway patency, reduces apnea and oxygen desaturation, and improves sleep quality and cognitive function.
121. What are common indications for CPAP therapy?
Obstructive sleep apnea, chronic heart failure, and airway support using one continuous pressure during spontaneous breathing.
122. What patient conditions are best treated with BiPAP?
COPD, intolerance to CPAP, and any condition requiring separate pressures for inhalation and exhalation to assist with ventilation and oxygenation.
123. How can you determine if BiPAP therapy is effective?
If the patient can exhale comfortably and their SpO₂ improves without further desaturation.
124. What is a nasal mask in the context of positive airway pressure therapy?
A mask shaped like a triangle that fits from the bridge of the nose to just above the upper lip.
125. What are nasal pillows used for in NPPV?
They rest just beneath the nose and offer minimal facial contact, making them more comfortable and less intrusive.
126. What is the purpose of a full face mask?
To cover both the mouth and nose for patients who are mouth breathers or need higher pressure settings.
127. Who is the nasal mask best suited for?
Patients who primarily breathe through their nose.
128. What is a nursing consideration for nasal masks?
Monitor the bridge of the nose for skin breakdown due to constant mask contact.
129. Who are nasal pillows most appropriate for?
Nose breathers, claustrophobic patients, those who read or watch TV in bed, patients with facial hair, and active sleepers.
130. What is an important nursing consideration for patients using nasal pillows?
Monitor for nasal dryness and nosebleeds since the device rests inside the nostrils.
131. Who benefits most from a full face mask?
Mouth breathers, patients with nasal congestion, those requiring high pressure, and BiPAP users.
132. What should nurses monitor with full face masks?
Ensure a proper seal, check for dry mouth, assess for leaks, and encourage good oral hygiene.
133. What are the potential complications of continuous positive airway pressure?
Stomach bloating, dry mouth, eye irritation from air leaks, and reduced pressure delivery due to leaks.
134. What is a red flag that may indicate an improper breathing technique or poor mask fit?
Eye irritation, which often signals a mask leak.
135. What are the pros and cons of full face masks in NPPV?
Advantages: good seal and effective for mouth breathers. Disadvantages: claustrophobia, aspiration risk, and need for alarm systems.
136. What does NPPV stand for, and how is it defined?
Noninvasive positive pressure ventilation; it provides ventilatory support without an artificial airway.
137. What complications can be avoided by using NPPV instead of mechanical ventilation?
Tracheal injury, infections, ventilator-associated pneumonia, barotrauma, and extended hospital stays.
138. What is CPAP in noninvasive ventilation?
Continuous positive airway pressure; it provides one constant airway pressure during spontaneous breathing without mechanical breaths.
139. How is CPAP pressure described in terms of IPAP and EPAP?
In CPAP, IPAP equals EPAP, creating a single continuous pressure.
140. What is BiPAP, and how does it differ from CPAP?
BiPAP (Bilevel Positive Airway Pressure) allows for separate inspiratory (IPAP) and expiratory (EPAP) pressures, aiding both oxygenation and ventilation.
141. What does IPAP control in BiPAP?
It regulates the peak airway pressure during inspiration to assist with ventilation.
142. What does EPAP regulate in BiPAP?
EPAP controls the airway pressure at the end of expiration and functions like PEEP (positive end-expiratory pressure).
143. What physiological effects does IPAP have during NPPV?
IPAP increases tidal volume and minute ventilation, directly affecting PaCO₂ levels and improving ventilation.
144. What physiological effects does EPAP have during NPPV?
EPAP functions similarly to PEEP by increasing functional residual capacity (FRC) and relieving upper airway obstruction, thereby improving oxygenation.
145. How can oxygenation and ventilation be assessed during NPPV?
Use PaO₂ or SpO₂ to assess oxygenation and PaCO₂ or PetCO₂ to assess ventilation effectiveness.
146. What are the primary indications for NPPV use?
Worsening alveolar hypoventilation (e.g., COPD), muscle weakness, refractory hypoxemia, or post-extubation difficulty.
147. What are contraindications for NPPV?
Apnea, inability to sustain life-supporting ventilation, vomiting risk, inability to handle secretions, confusion, mask intolerance, or facial trauma.
148. What are the key considerations when using a nasal mask for NPPV?
Minor leaks are acceptable if ventilation and oxygenation are maintained; mouth closure is required to avoid leaks.
149. What are the benefits of NPPV over invasive ventilation?
Patients can eat, speak, and avoid complications related to intubation.
150. What interfaces are commonly used with NPPV?
Nasal masks, full face masks, nasal pillows, and total face masks.
Final Thoughts
Bilevel positive airway pressure (BiPAP) is a cornerstone of noninvasive respiratory support. Its ability to deliver targeted pressure support makes it invaluable in both chronic and acute care settings.
For respiratory therapists, mastering the use of BiPAP is not just about knowing the machine—it’s about applying clinical judgment to improve outcomes, enhance comfort, and support the respiratory system in times of distress.
By staying updated on best practices and patient management strategies, respiratory care professionals can ensure BiPAP therapy is used effectively and safely in their clinical practice.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Khayat S, Ali M, Almasoudi L, Fatani A, Albarnawi W, Bsooki M, Ismail M. The Impact of BiLevel Positive Airway Pressure (BiPAP) Application Timing on Emergency Room Length of Stay in Patients With Pulmonary Edema: A Single-Center, Retrospective Cohort Study. Cureus. 2022.


