Coughing is a natural reflex that helps clear the airways of irritants, mucus, and foreign particles, but when it becomes severe or prolonged, it can place significant strain on the lungs and chest. While most coughing spells are harmless, in rare cases, they may trigger serious complications.
One such complication is a collapsed lung, or pneumothorax, which occurs when air escapes from the lung into the chest cavity. This article explores how coughing can potentially cause a collapsed lung, who is most at risk, and why it’s important to recognize the warning signs early.
Download our free guide that has over 100+ of the best tips for healthy lungs.
Can Coughing Cause a Collapsed Lung?
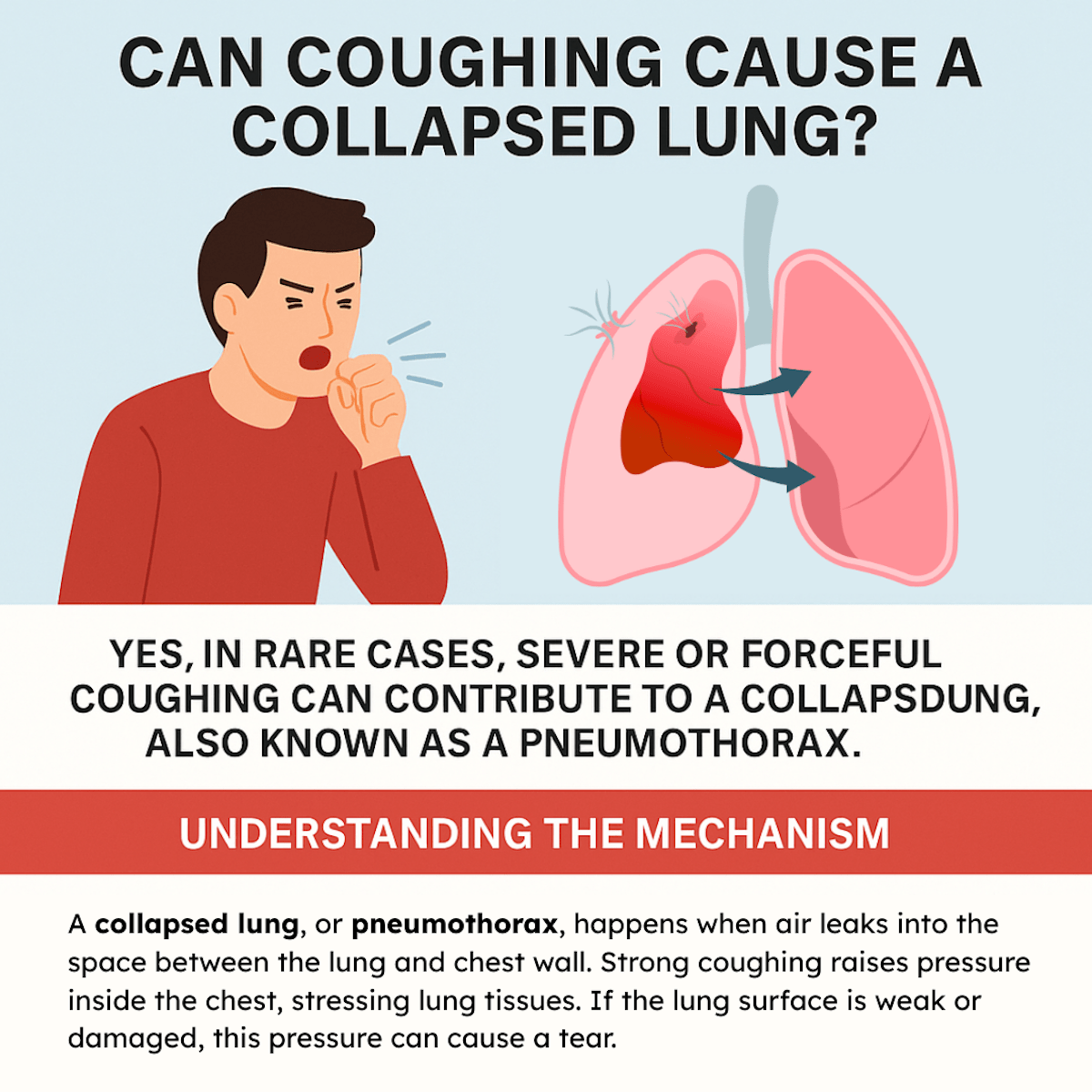
Yes, in rare cases, severe or forceful coughing can contribute to a collapsed lung, also known as a pneumothorax. This happens when the pressure from repeated or violent coughing causes a weak area in the lung to rupture, allowing air to leak into the space between the lung and chest wall.
People with underlying lung diseases, such as COPD, asthma, or emphysema, are at higher risk. For otherwise healthy individuals, coughing alone rarely causes this condition, but if sudden chest pain or shortness of breath follows intense coughing, prompt medical evaluation is necessary.
Understanding the Mechanism
A collapsed lung, or pneumothorax, happens when air leaks into the space between the lung and chest wall. Strong coughing raises pressure inside the chest, stressing lung tissues. If the lung surface is weak or damaged, this pressure can cause a tear.
This tear allows air to escape from the lung into the pleural space, causing part or all of the lung to collapse. People with preexisting lung diseases, such as COPD or asthma, are more vulnerable due to fragile lung tissue. Healthy lungs generally withstand coughing without collapsing.
Medical Evidence and Case Studies
Cases linking coughing to pneumothorax often involve severe or chronic coughs. Medical reports frequently note that patients with lung weakness, like emphysema, experience collapsed lungs after intense coughing spells.
For example, some case studies document spontaneous pneumothorax triggered by coughing fits in smokers or individuals with lung infections. However, isolated incidents in healthy individuals without underlying issues are extremely rare. Medical literature supports that coughing is more commonly a contributing factor rather than a direct cause.
Common Causes and Risk Factors
Certain conditions and habits increase the likelihood of a lung collapse related to coughing. These involve the strength and persistence of coughs, underlying lung health, and lifestyle choices that affect lung integrity.
Intense or Chronic Coughing Episodes
Frequent or severe coughing can raise pressure inside the chest, sometimes causing small tears in lung tissue. This can lead to air escaping from the lung into the space between the lung and chest wall, resulting in a collapsed lung, or pneumothorax.
People with prolonged respiratory infections or chronic bronchitis often experience these strong coughs, which heighten the risk. Sudden violent coughing fits, even in otherwise healthy individuals, can also trigger this condition by straining fragile lung areas.
Preexisting Lung Conditions
Diseases like chronic obstructive pulmonary disease (COPD), asthma, or cystic fibrosis weaken lung tissue and make it more prone to rupture. Bullae, which are air-filled sacs in the lungs, commonly occur in emphysema and can burst under coughing stress.
Individuals with past lung infections or trauma may have scar tissue, which is less elastic and more vulnerable to damage when coughing intensely. These preexisting conditions significantly raise the chance that coughing might lead to a pneumothorax.
Impact of Smoking and Lifestyle Factors
Smoking damages lung tissue, causing inflammation and reduced elasticity, which increases susceptibility to lung collapse during coughing. Nicotine and other chemicals weaken the lung’s defense mechanisms, prolonging lung healing and repair.
Lifestyle factors such as poor nutrition and exposure to environmental pollutants further degrade lung function. Smoking combined with vigorous, chronic coughing creates a higher risk profile for developing a collapsed lung.
Symptoms of a Collapsed Lung After Coughing
Signs of a collapsed lung can range from mild discomfort to severe, life-threatening conditions. Recognizing these symptoms early can lead to prompt medical attention and reduce complications.
Early Warning Signs
The first symptoms often include sudden, sharp chest pain localized on one side. This pain typically worsens with deep breaths or coughing. Shortness of breath may appear, even during minimal exertion or at rest. The person might experience mild difficulty breathing, a rapid heartbeat, or feeling lightheaded.
Coughing might intensify these symptoms, especially if the lung collapse is small but progressing. These early signs should not be ignored, as they indicate lung distress requiring evaluation.
Severe Presentations
If the lung collapse worsens, symptoms become more pronounced. Severe chest pain spreads and becomes constant. Breathing difficulty escalates, causing gasping or rapid, shallow breaths. Cyanosis, or bluish lips and fingers, may appear due to low oxygen levels.
In some cases, blood may be coughed up. A collapsed lung can cause a shift in the chest, visible as uneven chest movement during breathing. Immediate emergency care is necessary to prevent critical complications such as respiratory failure.
Diagnostic Methods
Diagnosing a collapsed lung caused by coughing involves careful assessment of symptoms and targeted imaging to confirm the condition. Both physical evaluation and visual confirmation play essential roles in identifying the issue accurately.
Clinical Evaluation
The clinician begins with a detailed history, focusing on the onset of symptoms, such as sudden chest pain or difficulty breathing, following a severe coughing episode. Physical examination includes checking for decreased breath sounds or uneven chest expansion on the affected side.
Signs such as low oxygen saturation or rapid breathing may also indicate lung collapse. Listening with a stethoscope can reveal abnormal sounds, including absent or diminished breath sounds where the lung has collapsed.
Imaging Techniques
Chest X-rays are the primary imaging method to confirm a pneumothorax. They show the presence of air in the pleural space and how much lung tissue has collapsed. Usually, an upright chest X-ray provides the best view.
In some cases, a CT scan is used for more detailed images, especially if the X-ray results are inconclusive or complications are suspected. Ultrasound can also be employed at the bedside to detect pneumothorax quickly in emergency settings.
Treatment and Recovery
Treatment for a collapsed lung caused by coughing depends on the size and severity of the pneumothorax. Recovery often involves medical procedures to remove air and prevent lung collapse from worsening.
Immediate Medical Interventions
If the lung collapse is small, doctors may monitor the patient and provide oxygen to help the lung re-expand naturally. Larger collapses require removal of the trapped air using a needle or chest tube connected to a suction device.
In emergency cases, surgery might be necessary to repair lung damage or prevent repeated collapses. Pain management and preventing infection are also important during this phase to support breathing and comfort.
Long-Term Management
Patients typically need follow-up chest X-rays for several weeks to ensure the lung heals fully. Avoiding activities that increase lung pressure, like heavy lifting or intense coughing, is advised during recovery.
Doctors may recommend breathing exercises or pulmonary rehabilitation to restore lung function. In some cases, lifestyle adjustments and treating underlying lung conditions are necessary to prevent recurrence.
Prevention and Reducing Risk
To lower the risk of a collapsed lung caused by coughing, it is important to manage coughs effectively. Persistent or severe coughing should be evaluated by a healthcare provider to avoid complications.
- Avoid smoking and exposure to lung irritants, as these increase lung vulnerability. Maintaining good lung health through regular exercise and avoiding respiratory infections also helps reduce risk.
- If someone has underlying lung conditions, following prescribed treatments closely is crucial. Using medications such as inhalers or cough suppressants as directed can minimize strain on the lungs.
- Staying hydrated and using humidifiers may ease coughing. Practicing gentle coughing techniques rather than forceful coughing can also decrease pressure on the lung tissue.
Note: Promptly addressing chest pain or shortness of breath after coughing is important. Early medical intervention can prevent a minor issue from developing into a collapsed lung.
FAQs About Coughing and Collapsed Lungs
Can Coughing Too Much Collapse a Lung?
Yes, in rare cases, excessive or violent coughing can contribute to a collapsed lung, also known as pneumothorax. This happens when the pressure from forceful coughing ruptures a weak spot in the lung, allowing air to leak into the chest cavity.
While this is uncommon in healthy individuals, people with lung diseases like COPD, asthma, or emphysema are at higher risk. If you experience sudden chest pain or shortness of breath after intense coughing, you should seek medical attention immediately.
What Is the Most Common Cause of a Collapsed Lung?
The most common cause of a collapsed lung is the rupture of a small air blister, called a bleb, on the lung’s surface. This can occur spontaneously, especially in tall, thin young men or people with underlying lung conditions.
Trauma, such as a rib fracture or chest injury, is another frequent cause. Medical procedures involving the chest can also increase the risk.
Note: While coughing can play a role, most cases of pneumothorax are unrelated to coughing alone.
Are There Warning Signs Before Your Lung Collapses?
A collapsed lung often happens suddenly, but some people may notice early warning signs. These can include sharp chest pain that worsens with deep breathing or coughing, sudden shortness of breath, rapid heart rate, or a feeling of tightness in the chest.
In mild cases, symptoms may be subtle and mistaken for anxiety or muscle strain. Because the condition can quickly worsen, any sudden chest pain or breathing difficulty should be taken seriously and evaluated by a healthcare professional right away.
Can Your Lungs Recover If They Collapse?
Yes, in many cases, the lungs can recover fully after collapsing, especially with proper treatment. A small pneumothorax may heal on its own over time, as the air trapped in the chest cavity gets reabsorbed. Larger cases may require medical intervention, such as inserting a chest tube to remove the air and allow the lung to re-expand.
Recovery time depends on the severity and underlying health, but most people regain normal lung function once healing is complete, provided no major complications occur.
Can a Collapsed Lung Get Worse?
Yes, a collapsed lung can worsen if it is left untreated. When more air leaks into the chest cavity, the pressure against the lung increases, making it harder to breathe. In severe cases, this can develop into a life-threatening condition called tension pneumothorax, where pressure also affects the heart and blood vessels.
Symptoms such as severe shortness of breath, low oxygen levels, or sudden changes in blood pressure require emergency medical attention. Prompt treatment is critical to prevent further complications and stabilize breathing.
Can Being Sick Cause a Collapsed Lung?
Yes, being sick can increase the risk of a collapsed lung, especially when illnesses involve persistent coughing or respiratory strain. Severe infections, asthma flare-ups, or conditions that weaken the lung tissue can make rupture more likely.
For example, people with pneumonia, tuberculosis, or chronic obstructive pulmonary disease (COPD) may be more vulnerable. While most illnesses don’t directly cause pneumothorax, the strain from coughing or inflamed lung tissue can raise the chances.
Note: Monitoring symptoms closely during illness is important for those at higher risk.
Would You Be Able to Tell If You Had a Collapsed Lung?
Often, yes, you would notice symptoms of a collapsed lung, though they can vary in severity. Common signs include sudden, sharp chest pain, shortness of breath, rapid breathing, and, in some cases, a bluish tint to the lips or skin due to low oxygen.
However, mild cases may only cause slight discomfort or breathlessness that can be mistaken for another issue. Because symptoms can progress quickly, anyone experiencing sudden chest pain and difficulty breathing should seek immediate medical evaluation to confirm or rule out pneumothorax.
Final Thoughts
Although it is uncommon, severe or persistent coughing can play a role in causing a collapsed lung, especially in individuals with underlying respiratory conditions or weakened lung tissue.
For most people, coughing is simply a protective reflex with no lasting harm, but for those at higher risk, the pressure generated during intense coughing fits can be enough to create complications.
Understanding the connection between coughing and pneumothorax highlights the importance of seeking medical care if sudden chest pain, shortness of breath, or other alarming symptoms develop. Early recognition and treatment are key to preventing further health issues.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- McKnight CL, Burns B. Pneumothorax. [Updated 2023 Feb 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.