Chronic obstructive pulmonary disease (COPD) is a progressive lung condition that makes it difficult to breathe and is a major cause of illness and death worldwide. Most often linked to long-term smoking and exposure to harmful irritants, COPD is not a single disease but rather a group of disorders that cause persistent airflow limitation.
The two primary types—emphysema and chronic bronchitis—present with distinct features but often overlap in patients. Understanding the differences between these conditions, how they are managed, and what to expect during an exacerbation is essential for students preparing for exams and for healthcare providers caring for patients.
This article explores the key characteristics, diagnostic findings, and treatment strategies for both emphysema and chronic bronchitis while highlighting exam tips that can help you master this topic.
Take our free course to master essential pathology concepts with TMC/CSE exam tips and helpful practice questions.
What is COPD?
Chronic obstructive pulmonary disease (COPD) is a chronic, progressive respiratory disorder that causes airflow limitation and makes it difficult for air to move in and out of the lungs. The airflow obstruction is not fully reversible, and symptoms typically worsen over time, especially if exposure to irritants continues.
Causes and Risk Factors
- Environmental exposure: Prolonged exposure to secondhand smoke, dust, chemical fumes, and occupational hazards (e.g., coal dust, silica, or asbestos).
- Air pollution: Chronic exposure to polluted air can aggravate lung damage.
- Genetics: In rare cases, alpha-1 antitrypsin deficiency, an inherited condition, can lead to early-onset COPD.
- Respiratory infections: Frequent childhood lung infections may increase susceptibility later in life.
Exam Tip: Smoking is the most common cause of COPD and should be the first factor that comes to mind. If the question mentions alpha-1 antitrypsin deficiency, think about a younger, nonsmoking patient with COPD symptoms.
Management of COPD
The primary goal of COPD management is to improve the patient’s quality of life, reduce symptoms, prevent hospitalizations, and slow disease progression. Treatment is tailored to the severity of the condition and whether the patient is stable or experiencing an acute exacerbation.
Conservative Management (Stable COPD)
- Low-flow oxygen therapy (e.g., nasal cannula 1–2 L/min) to maintain SpO₂ between 88–92%
- Long-acting bronchodilators to relax the airways and improve airflow
- Inhaled corticosteroids to reduce airway inflammation
- Smoking cessation – the single most important intervention to slow disease progression
- Pulmonary rehabilitation to improve exercise tolerance and overall health
- Patient education on avoiding triggers and recognizing early signs of exacerbations
- Vaccinations – influenza and pneumococcal vaccines help prevent infections that worsen COPD
- Healthy lifestyle habits, including exercise, proper nutrition, and adequate hydration
Management During an Acute Exacerbation
- Increase FiO₂ to correct hypoxemia (target SpO₂: 88–92%)
- Short-acting bronchodilators (e.g., albuterol) and anticholinergics (e.g., ipratropium) for bronchoconstriction
- Systemic corticosteroids to reduce airway inflammation
- Chest X-ray to rule out pneumonia, pneumothorax, or other complications
- Arterial blood gases (ABGs) to monitor ventilation and oxygenation status
- Non-invasive ventilation (BiPAP) for patients in ventilatory failure — preferred over intubation when possible
- Mechanical ventilation if the patient continues to deteriorate despite non-invasive support
Exam Tips: For stable COPD, expect compensated respiratory acidosis on the ABG analysis. For an acute exacerbation, look for uncompensated respiratory acidosis. Also, remember that COPD patients are often difficult to wean from the ventilator.
Signs and Symptoms of an Acute Exacerbation
An acute exacerbation of COPD occurs when symptoms suddenly worsen beyond the patient’s usual day-to-day variation. This flare-up can be triggered by respiratory infections, environmental irritants, or poor adherence to treatment, and it often requires urgent medical attention.
Common Signs and Symptoms
- Dyspnea – sudden increase in difficulty breathing
- Shortness of breath even at rest
- Wheezing due to airway narrowing
- Chest tightness
- Tachypnea (rapid breathing)
- Tachycardia (elevated heart rate)
- Hypoxemia (low blood oxygen)
- Cyanosis (bluish discoloration of lips or skin)
- Persistent cough with increased frequency
- Increased mucus production that may be thick or purulent
- Use of accessory breathing muscles to aid ventilation
- Peripheral edema due to right-sided heart strain (cor pulmonale)
Key Clinical Considerations
- Always evaluate ABGs to check for worsening acidosis and CO₂ retention.
- A chest X-ray may be necessary to rule out pneumonia or other complications.
- Exacerbations increase the risk of hospitalization and may accelerate lung function decline.
Exam Tip: If a patient with COPD presents with worsening shortness of breath, wheezing, and hypoxemia, the correct answer will usually involve: administering supplemental oxygen (with SpO₂ goal of 88–92%), giving a short-acting bronchodilator, considering systemic steroids, and recommending BiPAP if there is ventilatory failure.
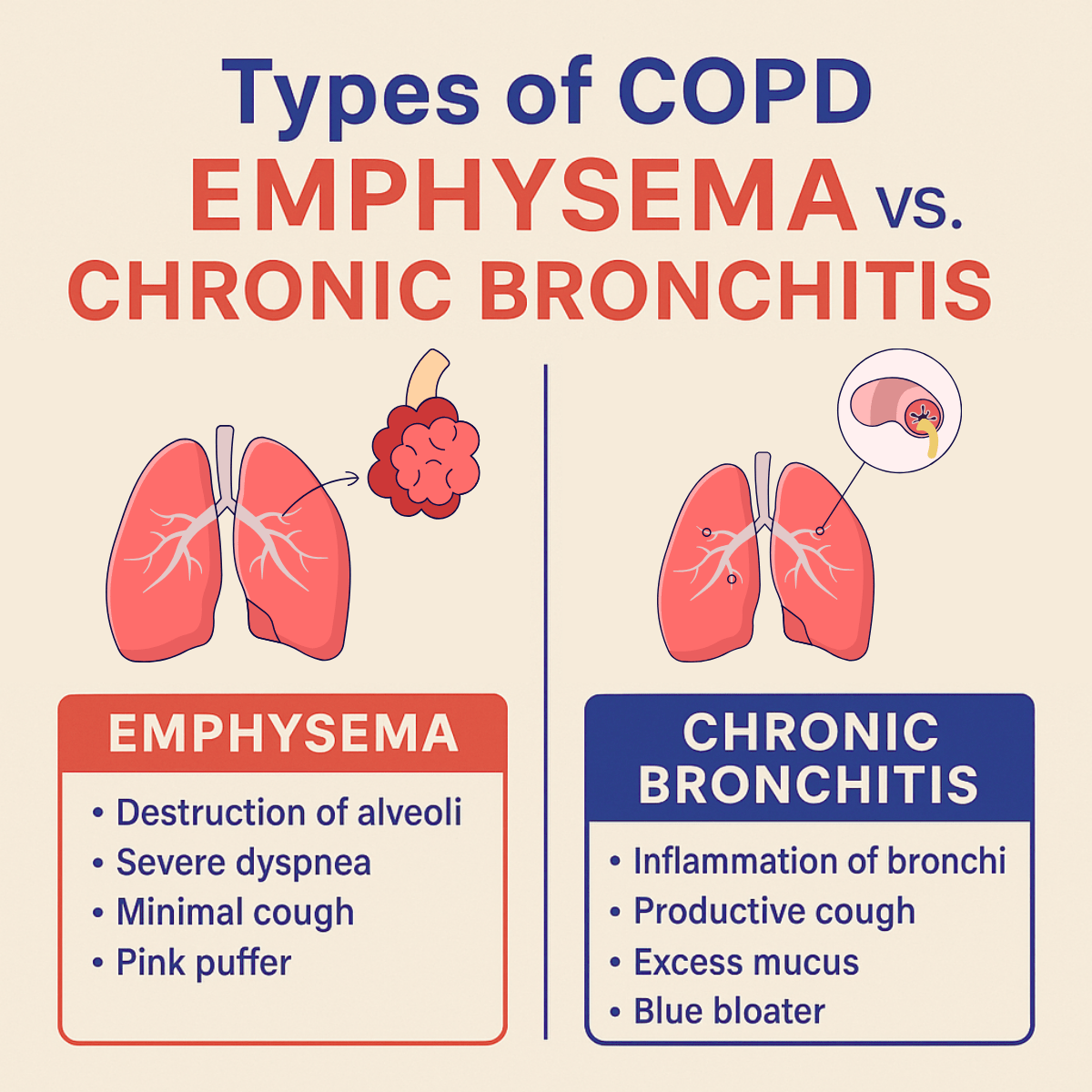
Types of COPD: Emphysema vs. Chronic Bronchitis
COPD primarily presents in two forms: emphysema and chronic bronchitis. Many patients have overlapping features of both, but recognizing the differences is essential for diagnosis, management, and exam preparation.
Emphysema
Emphysema is characterized by the destruction of alveolar walls, leading to loss of elasticity and overstretching of the air sacs. This causes air trapping, hyperinflation, and impaired gas exchange.
- Appearance: “Pink puffer” — thin build, barrel chest, pursed-lip breathing, use of accessory muscles, digital clubbing
- Dyspnea: Severe, progressive shortness of breath
- Cough: Minimal or absent; little mucus
- Breath sounds: Diminished with wheezing
- ABGs: Compensated respiratory acidosis with moderate hypoxemia
- Chest X-ray: Hyperinflation, flattened diaphragm, small heart
- Percussion: Hyperresonant note
- PFTs: Decreased flow rates
- Lung volumes: Increased RV and TLC
- DLCO: Decreased (loss of alveolar surface area)
- Lung compliance: Increased
Chronic Bronchitis
Chronic bronchitis involves persistent inflammation of the bronchial tubes, causing excessive mucus production and airway narrowing. It is defined clinically as a productive cough lasting at least three months per year for two consecutive years.
- Appearance: “Blue bloater” — stocky build, chronic hypoxemia, cyanosis, possible peripheral edema
- Dyspnea: Mild (compared to emphysema)
- Cough: Productive, frequent, with thick purulent mucus
- Breath sounds: Rhonchi and wheezing
- ABGs: Respiratory acidosis with moderate hypoxemia
- Chest X-ray: Increased cardiothoracic ratio, large heart, flattened diaphragm
- Percussion: Normal
- PFTs: Decreased flow rates
- Lung volumes: Increased RV
- DLCO: Normal
- Lung compliance: Normal
Clinical Considerations
- Emphysema patients often appear thin and cachectic due to increased work of breathing.
- Chronic bronchitis patients are more prone to right-sided heart failure (cor pulmonale) from long-standing hypoxemia and pulmonary hypertension.
- Airway clearance therapy is particularly important for chronic bronchitis to help remove secretions.
Board Exam Tips
- Think “Pink puffer = emphysema” and “Blue bloater = chronic bronchitis” for quick recall.
- DLCO values are a major differentiating point: decreased in emphysema, normal in chronic bronchitis.
- On the board exam, chronic productive cough = chronic bronchitis; severe dyspnea with minimal cough = emphysema.
Summary and Board Exam Strategy
Chronic obstructive pulmonary disease (COPD) is a long-term, progressive respiratory condition most often caused by cigarette smoking and environmental irritants. The two main types—emphysema and chronic bronchitis—share airflow limitation but differ in their clinical features, diagnostic findings, and progression.
- Emphysema is defined by alveolar damage, air trapping, and severe dyspnea, often seen in thin, barrel-chested patients with diminished breath sounds and decreased DLCO.
- Chronic bronchitis is marked by persistent inflammation of the bronchi, productive cough, and excess mucus, commonly in cyanotic “blue bloater” patients with right-sided heart strain.
Management focuses on conservative strategies, including low-flow oxygen, long-acting bronchodilators, inhaled corticosteroids, smoking cessation, pulmonary rehabilitation, and vaccinations, to improve daily function and reduce exacerbations.
During an acute exacerbation, treatment shifts to higher FiO₂, short-acting bronchodilators, systemic corticosteroids, ABG monitoring, and non-invasive ventilation such as BiPAP, with intubation as a last resort.
Board Exam Tips
- Remember the SpO₂ goal for COPD patients is 88–92%.
- Stable COPD = compensated respiratory acidosis; acute exacerbation = uncompensated respiratory acidosis.
- DLCO is decreased in emphysema but normal in chronic bronchitis.
- On a chest X-ray, emphysema shows hyperinflation with a small heart, while chronic bronchitis shows an enlarged heart.
- Chronic bronchitis patients often have copious mucus production and benefit from airway clearance therapy.
Final Thoughts
COPD remains a major global health challenge, but understanding the pathophysiology, clinical presentation, and treatment strategies for emphysema and chronic bronchitis is essential for both patient care and exam success.
By focusing on key differences, recognizing exacerbation signs, and mastering management principles, students and healthcare providers can be better prepared to improve outcomes for patients with this complex disease.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Agarwal AK, Raja A, Brown BD. Chronic Obstructive Pulmonary Disease. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.
- Pahal P, Avula A, Afzal M. Emphysema. [Updated 2025 Mar 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.
- Widysanto A, Goldin J, Mathew G. Chronic Bronchitis. [Updated 2025 Feb 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.