Gastroesophageal reflux disease (GERD) is commonly viewed as a digestive disorder associated with heartburn or acid reflux, but its impact extends far beyond the gastrointestinal system. In many patients, particularly infants, children, and individuals with chronic lung disease, GERD can significantly affect respiratory health. Refluxed stomach contents may irritate the airways, trigger asthma-like symptoms, contribute to chronic cough, or increase the risk of aspiration.
For respiratory therapists, understanding GERD is essential, as it can influence airway management, therapy selection, patient positioning, and overall respiratory care decisions across a wide range of clinical settings.
What Is Gastroesophageal Reflux Disease?
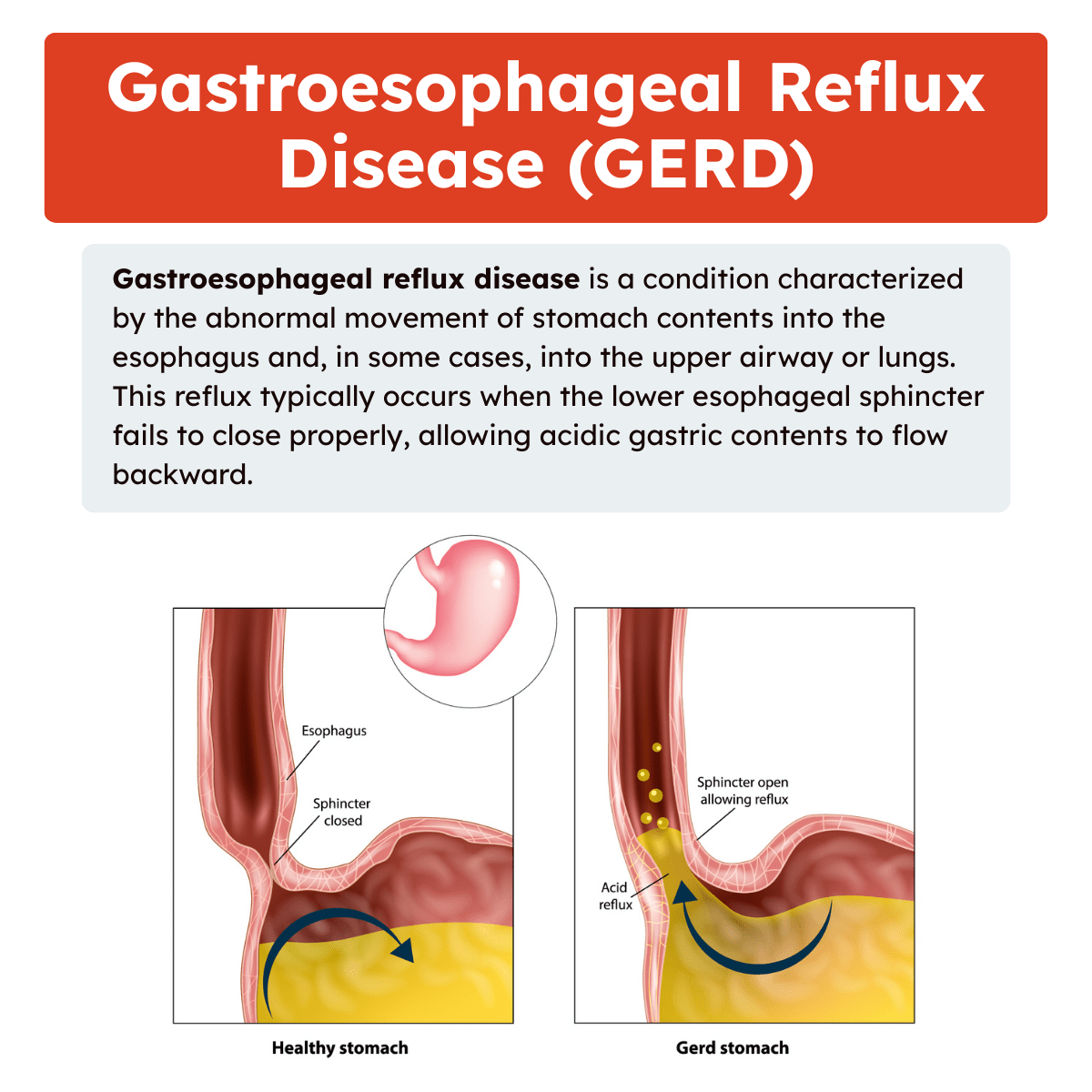
Gastroesophageal reflux disease is a condition characterized by the abnormal movement of stomach contents into the esophagus and, in some cases, into the upper airway or lungs. This reflux typically occurs when the lower esophageal sphincter fails to close properly, allowing acidic gastric contents to flow backward.
While occasional reflux can be normal, especially in infants and after meals, GERD refers to persistent or pathological reflux that leads to symptoms or complications. The acidic nature of gastric contents can irritate the esophagus, larynx, and airways, producing both gastrointestinal and respiratory manifestations.
In severe cases, refluxed material may be aspirated into the lungs, leading to inflammation, bronchospasm, or infection. This aspiration component is one of the most important reasons GERD is relevant to respiratory care.
GERD Across the Lifespan
GERD in Infants and Children
GERD is common in infancy and early childhood. Many cases are nonpathologic and resolve as the child matures. However, when reflux is severe or persistent, it can cause significant respiratory problems. These may include wheezing, recurrent pneumonia, choking spells, stridor, apnea, and laryngospasm.
GERD should be considered in infants who experience sudden life-threatening events or unexplained apnea. In older children, chronic cough, hoarseness, or recurrent head and neck symptoms may be linked to reflux rather than primary pulmonary disease.
GERD in Adults
In adults, GERD often presents with classic symptoms such as heartburn and regurgitation. However, many patients experience so-called “silent reflux,” where respiratory symptoms predominate. Chronic cough, asthma-like symptoms, chest pain, and hoarseness may all be manifestations of reflux, even in the absence of typical gastrointestinal complaints.
Respiratory Manifestations of GERD
GERD can affect the respiratory system through both direct and indirect mechanisms. Understanding these pathways helps respiratory therapists identify reflux-related symptoms and avoid unnecessary or ineffective interventions.
Aspiration and Microaspiration
One of the most direct respiratory consequences of GERD is aspiration. Acidic gastric contents can enter the airway, especially during sleep, supine positioning, or impaired airway protection. This can result in:
- Aspiration pneumonia
- Chemical pneumonitis
- Chronic airway inflammation
- Recurrent lower respiratory infections
Note: Microaspiration may occur repeatedly without obvious choking, leading to chronic lung injury over time.
Bronchoconstriction and Reflex Mechanisms
GERD can also provoke respiratory symptoms without overt aspiration. Acid exposure in the esophagus may stimulate vagal reflexes, leading to bronchoconstriction. This mechanism is believed to contribute to asthma-like symptoms in some patients.
Notably, reflux is nearly three times more prevalent in patients with asthma than in those without asthma. Although the relationship remains controversial, many clinicians recognize GERD as a potential trigger or exacerbating factor in difficult-to-control asthma.
Chronic Cough
Chronic cough, defined as lasting eight weeks or longer, is a common and frustrating clinical problem. When chest imaging is normal and serious disease is excluded, more than 90 percent of chronic cough cases are attributed to upper airway cough syndrome, asthma, and GERD.
In reflux-related cough, acid or nonacid reflux irritates laryngeal and esophageal receptors, triggering a cough reflex. Respiratory therapists frequently encounter these patients during pulmonary function testing, bronchodilator trials, or airway clearance therapy.
Upper Airway Complications
GERD may also affect the upper airway, leading to:
- Laryngospasm
- Hoarseness
- Stridor
- Chronic throat clearing
- Vocal cord irritation
Note: These symptoms can complicate airway management and mimic primary upper airway disorders.
GERD and Chronic Lung Disease
Asthma
The link between asthma and GERD is complex and bidirectional. Asthma may increase intrathoracic pressure changes that promote reflux, while reflux may worsen asthma symptoms through aspiration or vagal reflexes. For respiratory therapists, persistent asthma symptoms despite appropriate bronchodilator and anti-inflammatory therapy should raise suspicion for underlying GERD.
Cystic Fibrosis
Patients with cystic fibrosis are at higher risk for GERD due to chronic coughing, increased abdominal pressure, and altered gastrointestinal motility. Reflux in these patients can worsen airway inflammation and increase aspiration risk.
Because of this risk, patients with cystic fibrosis are generally no longer placed in head-down positions during postural drainage and percussion therapy. This change highlights how GERD directly influences respiratory therapy practice.
Interstitial Lung Disease and IPF
GERD is commonly found in patients with interstitial lung disease, particularly idiopathic pulmonary fibrosis (IPF). Symptoms of reflux should be actively sought in these patients, even if gastrointestinal complaints are minimal.
Although studied primarily in IPF, treatment of GERD has been associated with lower IPF-related mortality. This suggests that microaspiration may contribute to disease progression, reinforcing the importance of reflux management in chronic lung conditions.
GERD and Chest Pain in Respiratory Assessment
Respiratory therapists frequently encounter patients with chest pain. While pleuritic chest pain often points to pulmonary causes, non-pleuritic chest pain may be related to GERD, esophageal spasm, chest wall pain, or gallbladder disease.
Understanding GERD as a differential diagnosis helps respiratory therapists communicate effectively with the healthcare team and avoid misattributing symptoms solely to pulmonary pathology.
Diagnosis of GERD
GERD is diagnosed using a combination of clinical assessment and diagnostic testing. Common diagnostic tools include:
- Esophageal pH monitoring to measure acid exposure
- Upper gastrointestinal contrast studies
- Gastric scintiscan to evaluate reflux and aspiration risk
Note: While respiratory therapists do not perform these tests, familiarity with diagnostic methods enhances interdisciplinary communication and patient education.
Management of GERD
Medical Management
Most cases of GERD are managed medically. Treatment may include acid-suppressive therapy, dietary modifications, and positioning strategies. When GERD is identified in patients with respiratory disease, treatment often improves respiratory symptoms and reduces exacerbations.
Surgical Management
A small number of patients do not respond to medical therapy and may require surgical intervention, such as fundoplication. These cases are more common in severe pediatric reflux or neurologically impaired patients with recurrent aspiration.
Implications for Respiratory Therapy Practice
GERD directly affects how respiratory therapy is delivered. Failure to consider reflux can increase the risk of aspiration and compromise patient safety.
Airway Clearance Therapy
Postural drainage and percussion can exacerbate reflux, particularly in patients with known GERD or impaired airway protection. Head-down positioning increases the risk of aspiration and should be avoided when possible. Alternative airway clearance techniques may be more appropriate.
Treatment timing is also critical. Airway clearance and aerosol therapies should be scheduled before meals or at least two hours after eating or tube feedings to reduce the risk of vomiting and aspiration.
Aerosol and Mucoactive Therapy
Coughing induced by aerosol treatments may promote reflux in susceptible patients. RTs should monitor for signs of regurgitation and adjust therapy as needed.
Mechanical Ventilation and Airway Protection
Patients with GERD and reduced airway reflexes are at increased risk for aspiration while mechanically ventilated. Proper head-of-bed elevation, cuff pressure management, and vigilance for aspiration signs are essential components of care.
Patient Assessment and Education
Respiratory therapists play a key role in identifying reflux-related respiratory symptoms. Asking about heartburn, regurgitation, coughing after meals, or nighttime symptoms can provide valuable clinical clues.
Note: RTs also reinforce patient education on positioning, meal timing, and adherence to reflux treatment plans, especially in patients with chronic lung disease.
Gastroesophageal Reflux Disease Practice Questions
1. What is gastroesophageal reflux disease (GERD)?
A condition in which stomach contents reflux into the esophagus and sometimes the mouth due to impaired lower esophageal sphincter function.
2. How can GERD directly affect the respiratory system?
Refluxed gastric contents can be aspirated into the airway, causing inflammation, bronchospasm, and airway irritation.
3. Which respiratory symptoms are commonly associated with GERD?
Wheezing, chronic cough, laryngospasm, stridor, apnea, and aspiration pneumonia.
4. Why can GERD mimic asthma symptoms?
Acid reflux can trigger vagal reflexes that increase bronchial tone, leading to asthma-like bronchoconstriction.
5. Why is GERD often considered in patients with chronic cough?
GERD is one of the three most common causes of chronic cough lasting longer than 8 weeks.
6. What is a chronic cough?
A cough that persists for 8 weeks or longer.
7. Why should GERD be considered in infants with unexplained apnea or choking episodes?
Refluxed gastric contents may enter the airway, causing laryngospasm or airway obstruction.
8. Which diagnostic test directly measures acid exposure in the esophagus?
Esophageal pH monitoring.
9. What imaging study can help evaluate anatomical causes of reflux?
Upper gastrointestinal contrast studies.
10. What nuclear medicine study can assess gastric emptying and reflux?
Gastric scintigraphy (scintiscan).
11. How is GERD initially managed once diagnosed?
With medical therapy such as acid suppression, lifestyle modification, and feeding adjustments.
12. When is surgical intervention for GERD considered?
When symptoms are severe and unresponsive to optimal medical management.
13. Why is GERD especially relevant in patients with chronic lung diseases?
Repeated microaspiration can worsen lung injury and disease progression.
14. What is the relationship between GERD and interstitial lung disease?
GERD is common in ILD, and treating reflux may reduce disease progression, especially in idiopathic pulmonary fibrosis.
15. Why should head-down postural drainage be avoided in patients with GERD?
It increases the risk of reflux and aspiration.
16. How should airway clearance treatments be timed in patients with GERD?
Before meals or at least 2 hours after eating to reduce aspiration risk.
17. Why is GERD a concern during postural drainage and percussion therapy?
Reflux combined with impaired airway protection increases aspiration risk.
18. What role does vagal stimulation play in GERD-related respiratory symptoms?
Esophageal acid exposure can stimulate vagal nerves, increasing bronchoconstriction.
19. Which non-pulmonary condition commonly causes non-pleuritic chest pain similar to cardiac pain?
Gastroesophageal reflux disease.
20. Why must patient positioning be carefully considered during respiratory therapy in GERD?
Certain positions can worsen reflux and increase the risk of vomiting or aspiration.
21. How does GERD increase the risk of aspiration pneumonia?
Refluxed gastric contents can enter the airway, leading to chemical injury and infection of the lungs.
22. Why are patients with cystic fibrosis at increased risk for GERD?
Chronic coughing, increased intra-abdominal pressure, and altered gastrointestinal motility promote reflux.
23. What upper airway symptom suggests reflux-related laryngeal irritation?
Hoarseness due to chronic acid exposure of the vocal cords.
24. How can GERD contribute to recurrent laryngospasm?
Acid irritation of the larynx can trigger reflex closure of the vocal cords.
25. Why may GERD worsen nocturnal respiratory symptoms?
Supine positioning facilitates reflux and microaspiration during sleep.
26. What respiratory finding may suggest silent GERD in adults?
Unexplained chronic cough with a normal chest radiograph.
27. Why is GERD an important consideration in patients with unexplained wheezing?
Reflux-related bronchospasm can occur even in the absence of classic heartburn symptoms.
28. How can GERD affect sleep-disordered breathing?
Reflux episodes can provoke arousals, airway irritation, and apnea events.
29. Why should GERD be considered in patients with recurrent pneumonia?
Repeated aspiration of gastric contents can lead to frequent lower respiratory infections.
30. What role does lower esophageal sphincter dysfunction play in GERD?
It allows stomach contents to reflux into the esophagus and airway.
31. How can feeding tube placement influence GERD risk?
Gastric distention and positioning may increase reflux and aspiration risk.
32. Why is GERD associated with stridor in infants?
Acid exposure can cause supraglottic edema and airway narrowing.
33. What respiratory complication may result from chronic microaspiration?
Progressive airway inflammation and fibrosis.
34. How can GERD complicate airway clearance therapy?
Increased risk of vomiting and aspiration during treatments.
35. Why should GERD be assessed in patients with persistent throat clearing?
Chronic reflux can irritate the pharynx and larynx.
36. What positional strategy helps reduce reflux during respiratory treatments?
Maintaining the head of bed elevated.
37. How does GERD contribute to reactive airway disease?
Acid reflux triggers reflex bronchoconstriction and airway hyperresponsiveness.
38. Why may bronchodilators be ineffective in GERD-related wheezing?
The underlying cause is acid-induced reflex bronchospasm rather than airway smooth muscle disease.
39. What symptom may differentiate GERD-related cough from infectious cough?
Cough that worsens after meals or when lying down.
40. How can GERD influence ventilated patients?
Increased aspiration risk due to impaired airway reflexes.
41. Why is timing of respiratory treatments important in GERD?
Treatments given too soon after meals increase aspiration risk.
42. What upper gastrointestinal symptom may be absent in GERD patients with respiratory manifestations?
Heartburn
43. How does obesity contribute to GERD-related respiratory issues?
Increased abdominal pressure promotes reflux and airway aspiration.
44. Why is GERD considered in unexplained apnea episodes?
Reflux can stimulate airway reflexes causing breathing pauses.
45. How can chronic GERD affect lung transplant candidates?
Ongoing microaspiration can damage lung tissue and impair outcomes.
46. What breathing-related symptom may worsen during reflux episodes?
Chest tightness
47. How does GERD contribute to inflammation of the upper airway?
Repeated acid exposure damages mucosal surfaces.
48. Why is GERD a risk factor during supine positioning?
Gravity no longer helps keep gastric contents in the stomach.
49. What diagnostic clue suggests reflux-related respiratory symptoms?
Symptoms improve with acid-suppressive therapy.
50. Why must GERD be managed in patients with chronic lung disease?
Untreated reflux can worsen lung injury and impair respiratory function.
51. How can GERD contribute to chronic bronchitis symptoms?
Repeated aspiration of acidic contents can cause ongoing airway irritation and mucus production.
52. Why may GERD be suspected in patients with chronic cough but normal spirometry?
Reflux-related cough can occur without intrinsic airway obstruction.
53. How does gastric acid affect the bronchial mucosa when aspirated?
It causes chemical inflammation and increased airway sensitivity.
54. What respiratory symptom may worsen after large meals in GERD patients?
Shortness of breath due to reflux-induced airway irritation.
55. Why is GERD commonly overlooked in patients with respiratory complaints?
Symptoms may occur without classic gastrointestinal signs such as heartburn.
56. How can GERD aggravate existing asthma symptoms?
Acid reflux can trigger reflex bronchoconstriction via vagal stimulation.
57. What airway reflex is activated by esophageal acid exposure?
A vagally mediated reflex that increases bronchial tone.
58. Why can GERD cause morning hoarseness?
Nocturnal reflux irritates the vocal cords during sleep.
59. How does delayed gastric emptying increase GERD risk?
Prolonged stomach distention promotes reflux into the esophagus.
60. What respiratory finding may suggest aspiration from GERD?
Recurrent infiltrates in dependent lung segments.
61. Why should GERD be considered in patients with unexplained hypoxemia?
Chronic aspiration can impair gas exchange.
62. How does GERD contribute to chronic throat irritation?
Acid exposure damages pharyngeal mucosa.
63. What respiratory complication may result from untreated GERD over time?
Aspiration-related lung injury.
64. Why can GERD worsen symptoms during physical exertion?
Increased intra-abdominal pressure promotes reflux during activity.
65. How does GERD affect patients with neuromuscular disorders?
Impaired swallowing increases aspiration risk.
66. What symptom may indicate reflux-induced airway inflammation in children?
Recurrent wheezing without infection.
67. How does GERD influence airway protection mechanisms?
It can overwhelm protective reflexes, leading to aspiration.
68. Why is GERD relevant in patients with unexplained chest discomfort?
Reflux can mimic cardiac or pulmonary chest pain.
69. How can GERD complicate postural drainage therapy?
Positions may promote reflux and aspiration.
70. What respiratory sign may be associated with GERD-related laryngitis?
Inspiratory stridor
71. Why is GERD a concern in patients receiving enteral nutrition?
Tube feedings can increase gastric volume and reflux risk.
72. How does supine sleep position affect GERD-related respiratory symptoms?
It increases the likelihood of nocturnal aspiration.
73. What lung segments are most affected by aspiration due to GERD?
Dependent posterior segments of the lower lobes.
74. Why can GERD cause a sensation of chest tightness?
Esophageal irritation can mimic bronchoconstriction.
75. How does chronic GERD affect airway sensitivity?
It increases airway hyperresponsiveness.
76. Why may GERD be suspected in patients with recurrent sinus infections?
Reflux can reach the upper airway and sinuses.
77. How does GERD impact patients with obstructive sleep apnea?
Reflux episodes can worsen airway collapse and arousals.
78. What respiratory complication may follow repeated reflux aspiration?
Chronic inflammatory lung changes.
79. Why should GERD be managed aggressively in patients with chronic cough?
Treating reflux can resolve cough when other causes are excluded.
80. How can GERD alter the effectiveness of respiratory medications?
Persistent reflux may continue to trigger symptoms despite therapy.
81. How can GERD contribute to recurrent pneumonia?
Repeated microaspiration of gastric contents can introduce bacteria and cause inflammation in the lungs.
82. Why might GERD be suspected in patients with persistent nocturnal cough?
Reflux often worsens when lying flat, leading to nighttime airway irritation.
83. How does GERD affect the larynx in chronic cases?
Ongoing acid exposure can cause laryngeal inflammation and edema.
84. What respiratory symptom may occur without heartburn in GERD patients?
Chronic cough or wheezing
85. Why does GERD increase the risk of aspiration during sleep?
Protective airway reflexes are reduced during sleep.
86. How can GERD influence voice quality?
Acid irritation can lead to hoarseness and voice fatigue.
87. What pulmonary finding may suggest chronic aspiration from GERD?
Basilar crackles on auscultation.
88. Why are infants particularly vulnerable to GERD-related respiratory issues?
Immature esophageal sphincter function increases reflux risk.
89. How can GERD exacerbate symptoms in patients with chronic lung disease?
Reflux-induced inflammation adds to existing airway compromise.
90. Why should reflux be considered in patients with unexplained stridor?
Laryngeal edema from acid exposure can narrow the upper airway.
91. How does GERD contribute to bronchospasm?
Acid stimulation triggers reflex airway constriction.
92. What respiratory complication may arise from silent GERD?
Aspiration-related lung injury without obvious GI symptoms.
93. Why can GERD worsen breathing during bending or lifting?
Increased abdominal pressure promotes reflux into the esophagus.
94. How does GERD affect patients after prolonged intubation?
Airway irritation increases susceptibility to reflux-related injury.
95. What respiratory sign may improve after effective GERD treatment?
Chronic cough
96. Why is GERD relevant in patients with frequent choking episodes?
Refluxed material can enter the airway during swallowing.
97. How can GERD impact oxygenation in severe cases?
Repeated aspiration impairs alveolar gas exchange.
98. Why should GERD be considered in patients with unexplained wheezing?
Upper airway or reflex-mediated bronchoconstriction may be present.
99. How does GERD influence airway inflammation over time?
Chronic acid exposure sustains inflammatory processes.
100. What respiratory complication can result from untreated GERD in vulnerable patients?
Progressive aspiration-related lung disease.
Final Thoughts
Gastroesophageal reflux disease is far more than a gastrointestinal disorder. Its impact on the respiratory system is substantial, affecting patients across all age groups and contributing to a wide range of pulmonary symptoms and complications.
For respiratory therapists, GERD is a critical consideration in airway management, chronic disease assessment, and therapy planning.
By recognizing the respiratory manifestations of GERD, understanding its role in chronic lung disease, and adjusting treatment strategies accordingly, respiratory therapists help reduce aspiration risk, improve symptom control, and enhance overall patient outcomes. GERD is a prime example of how closely the respiratory and gastrointestinal systems are linked and why comprehensive, interdisciplinary care is essential in respiratory practice.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Clarrett DM, Hachem C. Gastroesophageal Reflux Disease (GERD). Mo Med. 2018.

