Hemoglobin is one of the most vital proteins in the human body. Found within red blood cells, it plays a central role in the transport of oxygen from the lungs to the tissues and the return of carbon dioxide from the tissues back to the lungs.
For respiratory therapists, understanding hemoglobin is essential, as it directly affects oxygen delivery, gas exchange, and patient outcomes in both acute and chronic respiratory conditions.
What Is Hemoglobin?
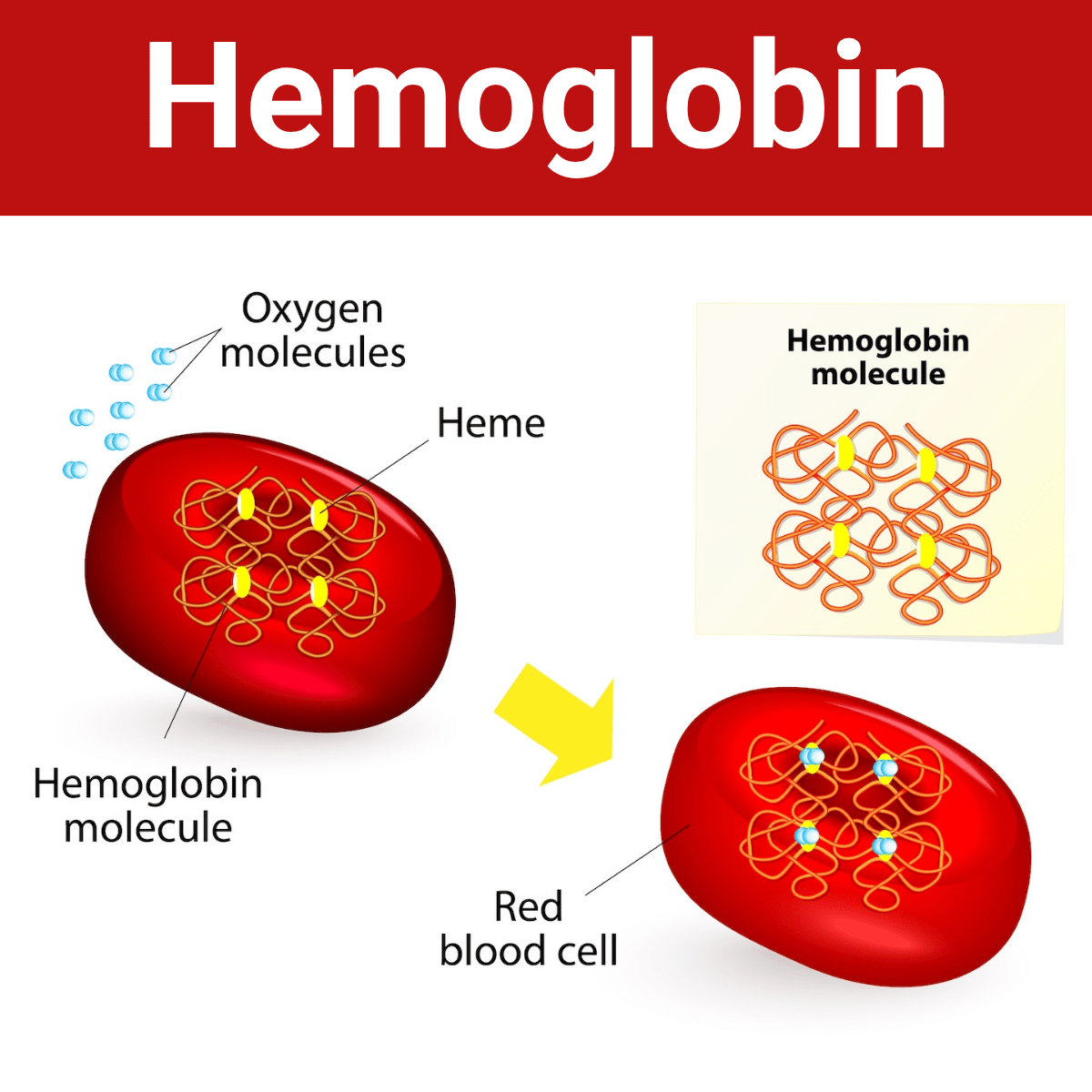
Hemoglobin is a complex, iron-containing protein that gives red blood cells their distinctive color. Each hemoglobin molecule is made up of four subunits—two alpha and two beta chains—each containing a heme group with an iron atom at its center. This iron atom binds oxygen molecules in the lungs, forming oxyhemoglobin, and releases them to tissues that need oxygen for cellular metabolism.
Beyond carrying oxygen, hemoglobin also helps transport carbon dioxide (CO₂) and maintain acid-base balance by acting as a buffer. The total hemoglobin concentration in the blood is a critical factor in determining the oxygen-carrying capacity of the circulatory system.
The Role of Hemoglobin in Gas Transport
Hemoglobin is responsible for carrying approximately 98% of the oxygen in the blood. When blood passes through the pulmonary capillaries, oxygen diffuses across the alveolar membrane and binds to hemoglobin in red blood cells. The amount of oxygen bound depends on the partial pressure of oxygen (PaO₂) and the affinity of hemoglobin for oxygen—a relationship illustrated by the oxygen-hemoglobin dissociation curve.
Under conditions such as high temperature, increased carbon dioxide, or acidosis, hemoglobin’s affinity for oxygen decreases (a phenomenon known as the Bohr effect), promoting oxygen release to the tissues. Conversely, in the lungs where oxygen levels are high and CO₂ is lower, hemoglobin readily binds oxygen.
Hemoglobin and Carbon Dioxide Transport
While hemoglobin is best known for transporting oxygen, it also carries about 20–30% of the carbon dioxide produced by cellular metabolism. This occurs when CO₂ binds to the globin portion of hemoglobin to form carbaminohemoglobin.
Additionally, hemoglobin plays a key role in buffering blood pH by binding free hydrogen ions, which helps maintain acid-base homeostasis—an essential aspect of respiratory physiology.
What Respiratory Therapists Must Know About Hemoglobin
For respiratory therapists, understanding hemoglobin is crucial for evaluating and managing patients with respiratory diseases and disorders. Many diagnostic and therapeutic decisions depend on accurate assessment of hemoglobin levels and oxygen saturation (SpO₂ or SaO₂).
Key examples include:
- Arterial Blood Gas (ABG) Interpretation: Hemoglobin concentration influences oxygen content (CaO₂), which helps therapists determine if oxygen delivery is adequate.
- Pulse Oximetry: Measures the percentage of hemoglobin saturated with oxygen, serving as a noninvasive tool for monitoring oxygenation status.
- Anemia and Hypoxia Management: Low hemoglobin reduces the oxygen-carrying capacity, even when oxygen saturation is normal, emphasizing the need to assess both hemoglobin and PaO₂.
- Mechanical Ventilation: Understanding hemoglobin-oxygen dynamics helps optimize FiO₂, PEEP, and other ventilator settings to enhance oxygen delivery.
Clinical Significance of Abnormal Hemoglobin Levels
- Low Hemoglobin (Anemia): Leads to tissue hypoxia, fatigue, and dyspnea. Causes include blood loss, nutritional deficiencies, or chronic diseases.
- High Hemoglobin (Polycythemia): May occur in chronic lung disease, high altitudes, or due to excessive erythropoietin production. This increases blood viscosity and can strain the heart.
- Abnormal Hemoglobin Variants: Such as carboxyhemoglobin (COHb) and methemoglobin (MetHb), impair oxygen transport and are important to recognize in carbon monoxide poisoning or certain drug toxicities.
Relevance in Respiratory Care
In the field of respiratory care, hemoglobin serves as a critical link between pulmonary function and cellular metabolism. Respiratory therapists routinely interpret hemoglobin-related data when assessing oxygenation, managing ventilator settings, or determining the need for supplemental oxygen.
For example, two patients might have identical oxygen saturations, but the one with lower hemoglobin delivers less oxygen to tissues—a nuance that can significantly impact clinical decisions.
Hemoglobin Practice Questions
1. What is hemoglobin?
A complex, iron-containing protein in red blood cells that transports oxygen from the lungs to the tissues and carbon dioxide from tissues to the lungs.
2. How many subunits make up one hemoglobin molecule?
Four subunits—two alpha and two beta chains—each containing a heme group.
3. What element at the center of each heme group binds to oxygen?
Iron (Fe²⁺).
4. What is oxyhemoglobin?
Hemoglobin bound to oxygen after oxygenation in the lungs.
5. What is the main function of hemoglobin in the body?
To carry oxygen to tissues and assist in the transport of carbon dioxide.
6. What percentage of oxygen in the blood is transported by hemoglobin?
Approximately 98%.
7. What is the oxygen-hemoglobin dissociation curve used to illustrate?
The relationship between oxygen partial pressure (PaO₂) and hemoglobin saturation (SaO₂).
8. What physiological conditions decrease hemoglobin’s affinity for oxygen?
Increased temperature, high CO₂, low pH (acidosis), and increased 2,3-DPG.
9. What is the Bohr effect?
A decrease in hemoglobin’s oxygen affinity caused by increased CO₂ and decreased pH, enhancing oxygen release to tissues.
10. Where in the body does hemoglobin have the highest oxygen affinity?
In the lungs, where PaO₂ is high and CO₂ is low.
11. What form of hemoglobin carries carbon dioxide?
Carbaminohemoglobin
12. What percentage of carbon dioxide in the blood is transported by hemoglobin?
Approximately 20–30%
13. How does hemoglobin help maintain acid-base balance?
By binding hydrogen ions, acting as a buffer.
14. What does the term “SaO₂” represent?
Arterial oxygen saturation — the percentage of hemoglobin binding sites occupied by oxygen.
15. Why is hemoglobin concentration important in ABG interpretation?
It affects total oxygen content (CaO₂), which determines how much oxygen is delivered to tissues.
16. What is the normal range for hemoglobin in adult males?
Approximately 13.5–17.5 g/dL
17. What is the normal range for hemoglobin in adult females?
Approximately 12.0–15.5 g/dL
18. How does anemia affect oxygen delivery?
It reduces oxygen-carrying capacity, even when oxygen saturation is normal.
19. What is polycythemia?
A condition with abnormally high hemoglobin concentration, often due to chronic hypoxemia or living at high altitude.
20. Why can polycythemia increase cardiac workload?
Because higher hemoglobin levels increase blood viscosity, making circulation more difficult.
21. What is carboxyhemoglobin (COHb)?
Hemoglobin bound to carbon monoxide instead of oxygen, impairing oxygen transport.
22. What is methemoglobin (MetHb)?
A form of hemoglobin where iron is oxidized to Fe³⁺, preventing oxygen binding.
23. What device is used to measure oxygen saturation noninvasively?
A pulse oximeter.
24. Why can a pulse oximeter give falsely high readings in carbon monoxide poisoning?
Because it cannot distinguish oxyhemoglobin from carboxyhemoglobin.
25. What blood test measures hemoglobin concentration directly?
A complete blood count (CBC).
26. In respiratory therapy, why must hemoglobin be considered when evaluating hypoxia?
Because low hemoglobin reduces oxygen delivery regardless of PaO₂ or SpO₂.
27. What condition might cause elevated hemoglobin in a COPD patient?
Chronic hypoxemia stimulating erythropoietin release and red blood cell production.
28. How does hemoglobin contribute to the buffering of blood pH?
It binds hydrogen ions released during CO₂ transport, minimizing pH changes.
29. What parameter reflects the total oxygen content of arterial blood?
CaO₂ (Arterial oxygen content).
30. How is CaO₂ calculated?
CaO₂ = (Hb × 1.34 × SaO₂) + (PaO₂ × 0.003).
31. What does a low CaO₂ value indicate?
Reduced oxygen delivery to tissues.
32. Which patient population commonly exhibits low hemoglobin due to chronic disease?
Patients with chronic kidney disease or malnutrition.
33. How does altitude affect hemoglobin production?
Chronic low oxygen levels stimulate erythropoietin, increasing hemoglobin concentration.
34. Why do respiratory therapists monitor hemoglobin levels in ventilated patients?
Because hemoglobin determines the blood’s oxygen-carrying capacity and affects oxygen delivery despite FiO₂.
35. What is the clinical significance of the oxyhemoglobin dissociation curve shifting to the right?
It means oxygen is released more easily to the tissues.
36. What causes a leftward shift in the oxyhemoglobin dissociation curve?
Alkalosis, hypothermia, and decreased 2,3-DPG, increasing oxygen affinity.
37. How can carbon monoxide poisoning shift the dissociation curve?
It shifts it to the left, reducing oxygen release to tissues.
38. What symptom commonly accompanies severe anemia due to low hemoglobin?
Dyspnea on exertion or fatigue from tissue hypoxia.
39. In ABG interpretation, what does a normal PaO₂ with low CaO₂ suggest?
Anemia — oxygen is present but total carrying capacity is reduced.
40. What happens to oxygen delivery when hemoglobin levels fall below 7 g/dL?
Tissue hypoxia develops even if oxygen saturation appears normal.
41. What is the common abbreviation for hemoglobin?
Hb or Hgb.
42. What type of molecule is hemoglobin?
An iron-containing protein found inside red blood cells (RBCs) responsible for oxygen transport.
43. What gives red blood cells their characteristic red color?
Hemoglobin
44. What is the main function of hemoglobin?
To bind oxygen in the lungs and carry it to tissues throughout the body.
45. What test is commonly used to measure the amount of hemoglobin in the blood?
A hemoglobin test or a complete blood count (CBC).
46. What does a hemoglobin test evaluate in clinical practice?
The oxygen-carrying capacity of the blood and the overall health of red blood cells.
47. Which other test is often performed alongside a hemoglobin test?
Hematocrit — which measures the percentage of blood volume made up of RBCs.
48. What is a normal function of the hematocrit test in relation to hemoglobin?
It helps assess red blood cell mass and supports the diagnosis of anemia or polycythemia.
49. When hemoglobin levels trend upward, what condition is likely present?
Polycythemia
50. When hemoglobin levels trend downward, what condition is indicated?
Anemia
51. What are common causes of elevated hemoglobin (polycythemia)?
Chronic hypoxia (e.g., COPD), congenital heart disease, dehydration, or high altitude.
52. What symptoms may occur in a patient with polycythemia?
Dizziness, headache, chest pain, hypertension, or visual disturbances due to thickened blood.
53. What are common causes of decreased hemoglobin (anemia)?
Blood loss, poor nutrition, chronic kidney disease, bone marrow disorders, or hemolysis.
54. What symptoms may suggest anemia in a patient?
Fatigue, pallor, tachycardia, shortness of breath, and decreased exercise tolerance.
55. When the oxygen-carrying capacity of the blood is reduced, the condition is known as what?
Anemia
56. When red blood cells clump together due to antigen-antibody interaction, what is this called?
Agglutination
57. During centrifugation of whole blood, what component settles at the bottom of the tube?
Red blood cells (RBCs)
58. How is hemoglobin concentration commonly measured in the lab?
Colorimetrically — by comparing the intensity of the red color in the blood sample.
59. What part of a hematology test allows visualization and quantification of white blood cells?
A differential white blood cell (WBC) count.
60. What branch of medicine studies the composition and diseases of blood?
Hematology
61. What are the two main components of blood?
A liquid phase (plasma) and a cellular phase (formed elements).
62. What are the three primary formed elements found in blood?
Red blood cells, white blood cells, and platelets.
63. What is the function of red blood cells?
To transport oxygen and carbon dioxide via hemoglobin.
64. What is the function of white blood cells?
To defend the body against infection and foreign substances.
65. What is the primary function of platelets?
To aid in blood clotting and wound repair.
66. What is the approximate lifespan of a red blood cell?
About 120 days.
67. Where are red blood cells and hemoglobin produced?
In the bone marrow.
68. What happens to old or damaged red blood cells?
They are removed by the spleen and liver through phagocytosis.
69. Why is iron important for hemoglobin function?
It allows oxygen molecules to bind reversibly to the heme groups.
70. How can severe anemia affect respiratory function?
It can cause dyspnea and increased respiratory rate due to decreased oxygen delivery to tissues.
71. What is hematocrit?
The ratio of the volume of packed red blood cells (RBCs) to the total volume of blood.
72. How is hematocrit value determined in the lab?
By centrifuging a blood sample and comparing the packed RBC column to the total column using a reader or scale card.
73. What is the normal hematocrit range for adult males?
40–54%
74. What is the normal hematocrit range for adult females?
37–47%
75. What is the primary objective of the RBC count test?
To determine the number of red blood cells per milliliter of whole blood.
76. What instrument or system is used to perform an RBC count?
The Ery-TIC dilution system, which helps dilute the blood for accurate cell counting.
77. What are the normal hemoglobin values for an adult male?
Approximately 13.5–16.5 g/dL
78. What are the normal hemoglobin values for an adult female?
Approximately 12.0–15.0 g/dL
79. Why are hemoglobin values included in a complete blood count (CBC)?
They help evaluate the blood’s oxygen-carrying capacity and detect anemia or polycythemia.
80. What does a low hemoglobin value typically indicate?
Anemia, which can result from blood loss, chronic disease, or reduced oxygen transport.
81. What does a high hemoglobin value typically indicate?
Polycythemia, often caused by chronic hypoxemia, dehydration, or high altitude.
82. Why can patients with normal PaO₂ still experience hypoxia if hemoglobin is low?
Because oxygen delivery depends on both oxygen content and hemoglobin concentration, not PaO₂ alone.
83. What is the main function of hemoglobin in oxygen transport?
Each hemoglobin molecule binds oxygen in the lungs and releases it to tissues.
84. How much oxygen can each gram of hemoglobin carry?
Approximately 1.34 mL of oxygen.
85. What percentage of oxygen in the blood is bound to hemoglobin?
About 98%
86. What percentage of oxygen is dissolved in plasma?
Approximately 2%, measured as PaO₂.
87. What is the most accurate way to assess oxygen delivery in the blood?
By calculating oxygen content (CaO₂).
88. What is the formula for arterial oxygen content (CaO₂)?
CaO₂ = (Hb × 1.34 × SaO₂) + (PaO₂ × 0.003).
89. Why is hemoglobin essential in the CaO₂ equation?
Because it determines the blood’s total oxygen-carrying capacity.
90. Can a normal ABG result still indicate tissue hypoxia?
Yes, if hemoglobin levels are low, oxygen delivery to tissues may still be inadequate.
91. What additional test is used to measure abnormal forms of hemoglobin?
Co-oximetry (hemoximetry)
92. What are two abnormal hemoglobin forms that can interfere with oxygen transport?
Carboxyhemoglobin and methemoglobin.
93. How does carboxyhemoglobin affect oxygen transport?
It binds carbon monoxide instead of oxygen, reducing oxygen delivery to tissues.
94. How does methemoglobin interfere with oxygen transport?
It contains iron in the ferric (Fe³⁺) state, which cannot bind oxygen effectively.
95. What are common causes of low hemoglobin (anemia)?
Blood loss, chronic disease, nutritional deficiency, bone marrow suppression, or renal failure.
96. What are common causes of high hemoglobin (polycythemia)?
Chronic hypoxemia, dehydration, high altitude, or bone marrow disorders.
97. Why can high hemoglobin levels be dangerous?
They increase blood viscosity, raising the risk of thrombosis and impairing circulation.
98. How should hypoxia caused by low hemoglobin be treated?
With blood transfusion or correction of the underlying cause, not just oxygen therapy.
99. At what hemoglobin level is transfusion typically considered?
When Hb falls below 7–8 g/dL, depending on the patient’s condition.
100. Why is hemoglobin monitoring important in respiratory therapy?
Because it helps assess oxygen delivery, guide oxygen therapy, and identify causes of persistent hypoxia.
Final Thoughts
Hemoglobin is a key protein that enables oxygen transport and carbon dioxide removal throughout the body. Its structure and behavior determine how efficiently gases are exchanged between the lungs and tissues.
For respiratory therapists, understanding hemoglobin is important for interpreting test results, managing oxygen therapy, and providing effective patient care. A clear grasp of hemoglobin physiology helps connect respiratory function with the body’s overall metabolic needs.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Farid Y, Bowman NS, Lecat P. Biochemistry, Hemoglobin Synthesis. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.

