Lung cancer remains one of the leading causes of cancer-related deaths worldwide, with surgical resection traditionally considered the gold standard treatment for early-stage disease. However, the effectiveness of surgical removal as a standalone treatment for lung cancer faces significant limitations that oncologists and patients must understand.
While surgery can be curative in certain circumstances, its success is constrained by multiple factors, including disease stage at diagnosis, patient health status, cancer biology, and the inherent challenges of completely eliminating all malignant cells.
This article examines the various reasons why surgical removal of lung cancer, while important, is not universally effective and explores the complex factors that influence treatment outcomes.
Download our free guide that has over 100+ of the best tips for healthy lungs.
Why is the Surgical Removal of Lung Cancer Ineffective?
Surgical removal of lung cancer can be ineffective when the disease is diagnosed at an advanced stage or has already spread (metastasized) beyond the lungs. In such cases, removing the primary tumor does not address cancer cells that may have traveled to other parts of the body.
Additionally, some tumors are located in areas that are difficult to access or involve vital structures, making surgery too risky. Patients with poor lung function or other serious health conditions may also be unable to tolerate the procedure. Therefore, surgery is most effective only when the cancer is localized and caught early.
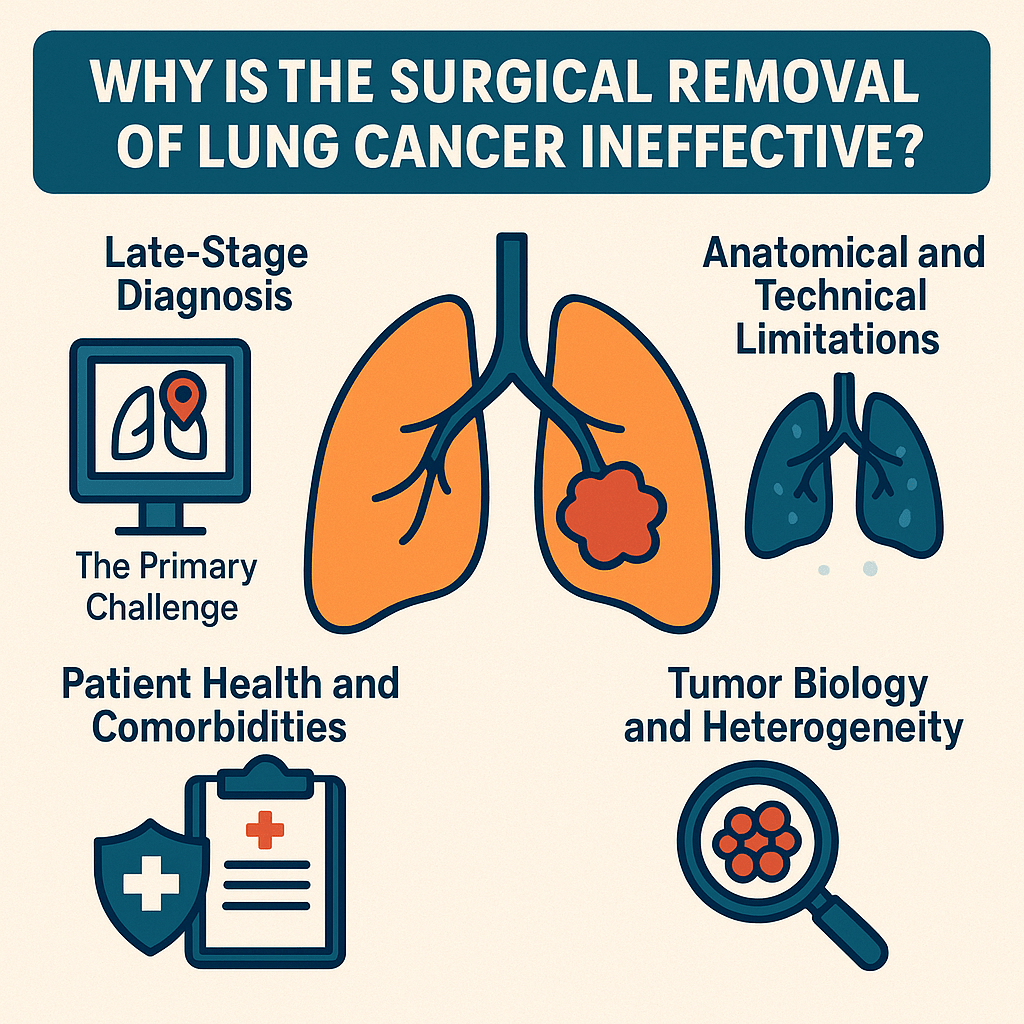
Late-Stage Diagnosis: The Primary Challenge
The most significant limitation of surgical treatment for lung cancer stems from the fact that the majority of cases are diagnosed at advanced stages when surgery is no longer a viable option. Lung cancer is often called a “silent killer” because early-stage disease typically produces few or no symptoms. By the time patients experience noticeable symptoms such as persistent cough, chest pain, shortness of breath, or weight loss, the cancer has frequently progressed beyond the point where surgical resection alone can provide a cure.
Statistics reveal that only approximately 20-25% of lung cancer patients are diagnosed with early-stage disease suitable for surgical intervention. The remaining 75-80% present with locally advanced or metastatic disease, where the cancer has spread beyond the primary tumor site to nearby lymph nodes, adjacent organs, or distant parts of the body. In these cases, surgical removal of the primary tumor would not address the widespread nature of the disease.
The lack of effective screening programs for lung cancer has historically contributed to this problem. Unlike other cancers, such as breast or colorectal cancer, which have well-established screening protocols, lung cancer screening with low-dose computed tomography (LDCT) has only recently gained widespread acceptance and implementation. Even with current screening recommendations for high-risk individuals, many patients still present with advanced disease.
Anatomical and Technical Limitations
The lungs’ complex anatomy presents unique challenges for surgical intervention. The proximity of vital structures such as major blood vessels, the heart, esophagus, and critical nerves makes complete tumor removal technically difficult and potentially dangerous. Tumors located near the hilum (the central part of the lung where blood vessels and airways enter) or those that have invaded the chest wall, diaphragm, or mediastinal structures may be deemed inoperable due to the risk of damaging essential organs.
Furthermore, the extensive lymphatic drainage system of the lungs allows cancer cells to spread to regional lymph nodes early in the disease process. Even when the primary tumor appears resectable, microscopic involvement of lymph nodes may not be detectable during preoperative staging, leading to inadequate surgical margins and increased risk of recurrence.
The concept of “microscopic residual disease” represents another significant limitation. Even when surgeons believe they have achieved complete resection with clear margins, microscopic cancer cells may remain in the surrounding tissue or have already disseminated to distant sites. These invisible remnants can later give rise to local recurrence or metastatic disease, explaining why surgery alone is often insufficient for long-term cure.
Patient Health and Comorbidities
Many lung cancer patients are not suitable candidates for surgical resection due to compromised overall health and comorbidities. The strong association between lung cancer and smoking history means that many patients have concurrent conditions such as chronic obstructive pulmonary disease (COPD), cardiovascular disease, or reduced lung function that significantly increase surgical risk.
Pulmonary function tests are crucial in determining surgical candidacy. Patients must have adequate respiratory reserve to tolerate the removal of lung tissue while maintaining sufficient breathing capacity for daily activities. Those with severely compromised lung function may not survive the immediate postoperative period or may experience such significant disability that surgery becomes contraindicated.
Age is another important factor, as lung cancer predominantly affects older adults who may have multiple comorbidities and reduced physiological reserve. The stress of major thoracic surgery, combined with general anesthesia and prolonged recovery, can be prohibitive for elderly or frail patients.
Tumor Biology and Heterogeneity
The biological behavior of lung cancer varies significantly between different histological types and even within the same tumor. Non-small cell lung cancer (NSCLC), which comprises about 85% of all lung cancers, includes several subtypes with distinct characteristics. Small cell lung cancer (SCLC), representing approximately 15% of cases, is typically more aggressive and has usually spread beyond the primary site at diagnosis, making surgical resection rarely appropriate.
Tumor heterogeneity refers to the fact that different areas of the same tumor may exhibit varying genetic mutations, growth patterns, and responses to treatment. This biological diversity makes it challenging to predict which patients will benefit most from surgical intervention and increases the likelihood that some cancer cells will possess characteristics that enable them to survive and proliferate despite the surgical removal of the primary tumor.
The concept of cancer stem cells further complicates surgical treatment. These cells, which may represent only a small fraction of the total tumor burden, possess the ability to regenerate entire tumors and may be particularly resistant to conventional treatments. Even if the bulk of the tumor is successfully removed, surviving cancer stem cells can lead to recurrence.
Inadequate Staging and Hidden Metastases
Accurate staging is crucial for determining the appropriateness of surgical intervention. However, current imaging techniques and staging procedures have limitations that can lead to understaging of the disease. Small metastatic deposits in distant organs may not be detectable by conventional imaging studies such as CT scans or PET scans, leading to a false assessment of early-stage disease.
The phenomenon of “occult metastases” refers to cancer spread that is present but not detectable at the time of diagnosis. These hidden metastases become apparent only after attempted curative surgery when patients develop recurrent disease in distant sites. This situation highlights the systemic nature of lung cancer and explains why local treatment alone is often insufficient.
Mediastinal lymph node involvement can be challenging to accurately assess, even with advanced imaging techniques. The sensitivity and specificity of imaging studies for detecting lymph node metastases are not perfect, and surgical staging procedures, such as mediastinoscopy or endobronchial ultrasound with biopsy, may also miss microscopic disease.
The Role of Molecular Characteristics
Modern understanding of lung cancer has revealed the importance of molecular and genetic characteristics in determining treatment response and prognosis. Tumors with specific genetic mutations, such as EGFR mutations, ALK rearrangements, or ROS1 fusions, may respond better to targeted therapies than to surgical resection alone.
The identification of these molecular markers has led to a more personalized approach to lung cancer treatment, where the optimal therapy is selected based on the tumor’s genetic profile rather than solely on staging and resectability.
In some cases, patients with resectable tumors may achieve better outcomes with targeted therapy or immunotherapy than with surgery, particularly if their tumors harbor specific mutations.
Postoperative Complications and Recovery
Surgical resection of lung cancer is associated with significant morbidity and mortality risks that can impact its effectiveness as a treatment modality. Major complications can include pneumonia, respiratory failure, cardiac complications, prolonged air leaks, and wound healing problems.
The mortality rate for lung cancer surgery, while generally low at experienced centers, still represents a significant consideration, particularly for high-risk patients.
The recovery period following lung cancer surgery can be prolonged and may significantly impact quality of life. Patients may experience reduced exercise tolerance, chronic pain, and psychological effects that can affect their ability to tolerate additional treatments if needed.
For some patients, particularly those with marginal pulmonary function, the functional impact of surgery may be so severe that their overall survival and quality of life are adversely affected.
Limitations of Surgical Margins
Achieving adequate surgical margins is crucial for successful cancer treatment, but this can be challenging in lung cancer surgery. The concept of “clear margins” refers to the absence of cancer cells at the edges of the resected tissue. However, determining what constitutes an adequate margin in lung cancer is complex and depends on factors such as tumor size, location, and histological type.
Even when margins appear clear on pathological examination, microscopic disease may extend beyond the resected area. The three-dimensional nature of lung anatomy and the potential for skip lesions (areas of cancer separated from the main tumor by normal tissue) can make complete removal difficult to achieve and verify.
The Systemic Nature of Advanced Disease
Perhaps the most fundamental limitation of surgical treatment for lung cancer is the recognition that cancer, even when it appears localized, is often a systemic disease. By the time a lung tumor is detectable, cancer cells may have already begun to circulate in the bloodstream and establish microscopic deposits in distant organs.
This systemic nature of cancer explains why patients with apparently early-stage disease can develop recurrent cancer after seemingly successful surgery.
Note: The primary tumor may represent only the visible portion of a more widespread disease process, making local treatment insufficient for cure.
FAQs About the Surgical Removal of Lung Cancer
Can Cancer Be Surgically Removed From the Lungs?
Yes, lung cancer can be surgically removed if it is detected at an early stage and has not spread beyond the lungs. Surgery aims to remove the tumor along with a portion of surrounding lung tissue, and sometimes nearby lymph nodes.
The most common surgical options include lobectomy, segmentectomy, and pneumonectomy. However, not all patients are candidates for surgery, especially if the cancer is advanced or the patient has poor lung function or other significant health issues.
What Are the Disadvantages of Lung Cancer Surgery?
Lung cancer surgery, while potentially life-saving, comes with several disadvantages. It’s a major procedure that can result in pain, a long recovery period, and reduced lung capacity. Some patients may experience complications, including infections, bleeding, or respiratory problems.
Additionally, surgery does not guarantee a cure, especially if cancer cells remain or have spread elsewhere. For patients with other health conditions, surgery may be too risky. These factors must be taken into account when considering surgical treatment.
What Are the Risks of Lung Cancer Surgery?
Risks of lung cancer surgery include bleeding, infection, pneumonia, and blood clots. There is also a risk of anesthesia-related complications. In some cases, patients may experience prolonged shortness of breath due to reduced lung capacity, particularly when a significant portion of lung tissue is removed.
Other potential complications include prolonged air leaks, arrhythmias, or the need for a ventilator after surgery. Surgeons typically assess a patient’s overall health and lung function before recommending surgery.
What Are the Types of Surgery for Lung Cancer?
The main types of lung cancer surgery are lobectomy, pneumonectomy, segmentectomy, and wedge resection. A lobectomy removes one of the lung’s lobes and is the most common surgery for non-small cell lung cancer.
A pneumonectomy involves removing an entire lung and is used for larger or centrally located tumors. Segmentectomy and wedge resection are less invasive and remove smaller portions of the lung, typically used for early-stage cancers or when lung function is limited.
Final Thoughts
While surgical resection remains an important component of lung cancer treatment and can be curative for appropriately selected patients with early-stage disease, its limitations are substantial and multifaceted.
The late presentation of symptoms, technical challenges related to anatomy and tumor location, patient comorbidities, tumor biology, staging limitations, and the often systemic nature of the disease all contribute to the reduced effectiveness of surgery as a standalone treatment.
Understanding these limitations has led to the development of multimodal treatment approaches that combine surgery with chemotherapy, radiation therapy, targeted therapy, and immunotherapy. The goal is to address both local and systemic disease while minimizing treatment-related morbidity and mortality.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Siddiqui F, Vaqar S, Siddiqui AH. Lung Cancer. [Updated 2023 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.
- Montagne F, Guisier F, Venissac N, Baste JM. The Role of Surgery in Lung Cancer Treatment: Present Indications and Future Perspectives-State of the Art. Cancers (Basel). 2021.


