Lung nodules are small, round or oval spots that appear within the lung tissue, often discovered unexpectedly during imaging tests performed for other reasons. While most nodules are harmless and result from past infections, inflammation, or scar tissue, their presence can understandably raise concern because they may also signal more serious conditions, including lung cancer.
The challenge lies in determining which nodules are benign and which require closer attention. Understanding when to worry about lung nodules—and when they are likely not a cause for alarm—can help patients approach the situation with clarity, reduce unnecessary anxiety, and ensure timely medical evaluation when needed.
Download our free guide that has over 100+ of the best tips for healthy lungs.
When to Worry About Lung Nodules?
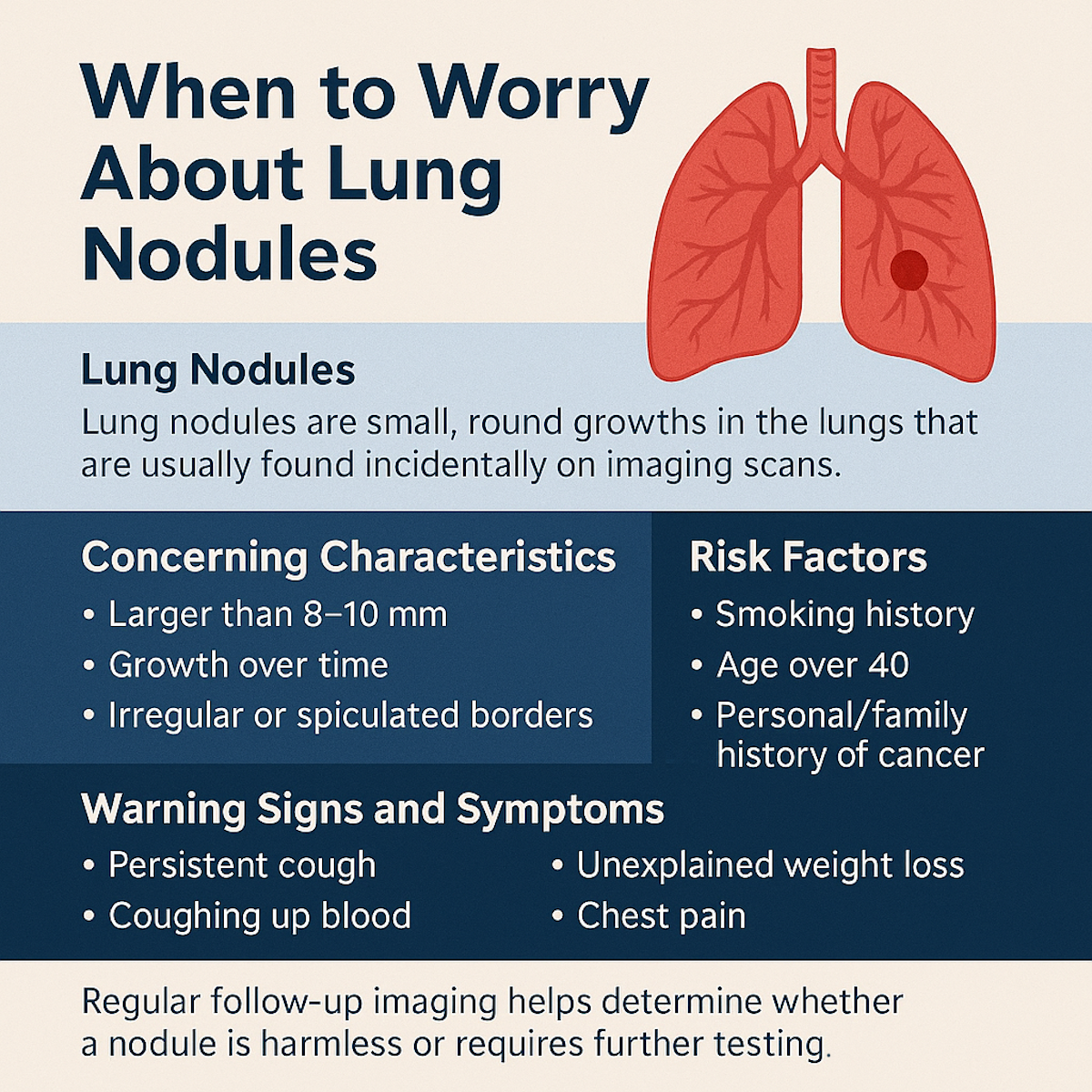
Lung nodules are small, round growths in the lungs that are usually found incidentally on imaging scans. In many cases, they are benign and caused by old infections, scar tissue, or noncancerous conditions. However, they can sometimes be an early sign of lung cancer.
You should worry about lung nodules if they are larger than 8–10 mm, show growth over time, or have irregular or spiculated borders. Risk factors such as smoking history, age over 40, or a personal/family history of cancer also raise concern.
If you develop symptoms such as persistent cough, coughing up blood, unexplained weight loss, or chest pain, prompt evaluation is necessary. Regular follow-up imaging helps determine whether a nodule is harmless or requires further testing.
What Are Lung Nodules?
Lung nodules are rounded or irregular spots measuring less than 3 centimeters found on chest X-rays or CT scans. They often appear as single, isolated spots but can sometimes occur in clusters. Many nodules are benign and discovered incidentally during imaging for other reasons.
Their size and growth rate are key factors in evaluating risk. Nodules smaller than 6 mm typically require less aggressive monitoring, while larger nodules often need more detailed investigation through repeated imaging or biopsy.
Types of Lung Nodules
There are two main types of lung nodules: solid and subsolid. Solid nodules are dense and easier to see on scans. Subsolid nodules can include part-solid or ground-glass opacities, which are less dense and harder to characterize.
Subsolid nodules have a higher chance of being associated with early lung cancer but can also be related to inflammation or infection. The distinction between types helps guide doctors on the urgency and method of follow-up.
Common Causes
Lung nodules may result from infections such as tuberculosis or fungal diseases that leave scar tissue. They can also form from non-infectious inflammation caused by conditions like rheumatoid arthritis or sarcoidosis.
Benign tumors and healed injuries can create nodules that remain stable over time. On the other hand, malignant nodules are often linked to lung cancer, especially in smokers or those with a history of cancer. Identifying the cause determines the next steps in management.
When to Worry About Lung Nodules
Lung nodules often require careful evaluation based on their features and patient history. Certain signs, nodule characteristics, and risk factors guide the decision about when further investigation or treatment is necessary.
Warning Signs and Symptoms
Most lung nodules do not cause symptoms and are found incidentally during imaging. However, new respiratory symptoms such as persistent cough, coughing up blood, unexplained weight loss, or chest pain can be concerning.
If any of these symptoms occur alongside a lung nodule, it raises suspicion for malignancy or infection. Immediate medical evaluation is advised, especially if symptoms have appeared recently or are worsening.
Size and Growth Patterns
Nodule size is a key factor in assessing risk. Nodules larger than 8-10 millimeters usually prompt closer observation or biopsy. Smaller nodules under 6 millimeters often require only periodic monitoring.
Growth rate is critical; a doubling in size within 1-6 months suggests malignancy. Stability over 2 years generally indicates a benign nodule. Rapid growth or changes in size demand prompt medical attention.
Risk Factors Increasing Concern
Certain patient factors increase the likelihood that a lung nodule is cancerous. These include a history of smoking, older age (over 50 years), prior cancer, and occupational exposures like asbestos.
A family history of lung cancer and underlying lung diseases also elevates risk. Patients with these factors should have more frequent and thorough evaluations of their nodules.
Nodule Appearance on Imaging
Characteristics seen on CT scans help differentiate benign from malignant nodules. Solid nodules with irregular or spiculated edges are more suspicious than smooth, well-defined ones.
Calcification patterns matter: diffuse, central, or laminated calcifications tend to indicate benign nodules, while eccentric or absent calcification is concerning. Ground-glass opacities may require further assessment due to the potential for early cancer.
Diagnosis and Evaluation
The process of diagnosing lung nodules involves various imaging techniques and guidelines to assess risk. Careful follow-up and advanced diagnostics help determine if nodules are benign or require further intervention.
Initial Detection Methods
Lung nodules are most commonly found through chest X-rays or low-dose CT scans, especially during lung cancer screening or imaging for unrelated issues. CT scans provide more detailed images, allowing precise measurement of nodule size, shape, and location.
Radiologists evaluate characteristics such as nodule margins, density, and calcification patterns to estimate malignancy risk. Larger nodules or those with irregular edges raise more concern and often prompt further testing.
Follow-Up and Monitoring Guidelines
Follow-up imaging is crucial for monitoring nodule growth or changes. Guidelines suggest timing based on nodule size and risk factors:
- Nodules smaller than 6 mm usually require no routine follow-up.
- Nodules 6-8 mm typically undergo CT scans at 6 to 12 months, then annually if stable.
- Nodules larger than 8 mm need more frequent scans or biopsy consideration.
Note: Smoking history, age, and prior cancer influence follow-up schedules. Stability over two years typically indicates a benign nodule.
Advanced Diagnostic Tools
When imaging is inconclusive, advanced tests are used. PET scans assess the metabolic activity of nodules, helping distinguish cancerous lesions by their glucose uptake.
Biopsies—either via bronchoscopy or CT-guided needle—provide tissue for histological analysis. Molecular testing on biopsy samples may identify specific mutations guiding treatment if cancer is present.
Other techniques, like radial endobronchial ultrasound, improve biopsy accuracy in small or hard-to-reach nodules. These tools reduce unnecessary surgery and improve diagnosis precision.
Lung Nodule Risk Factors
Certain factors increase the likelihood that a lung nodule may signal a serious condition. These include personal habits, genetic background, and environmental exposures that affect lung health.
Smoking History
Smoking is the most significant risk factor for lung nodules that could be cancerous. The risk rises with the intensity and duration of smoking, especially in those who have smoked for many years or are heavy smokers.
Both current and former smokers face increased risk compared to never-smokers. A history of smoking combined with age over 50 significantly raises the chance that a nodule is malignant. Quitting lowers risk but does not eliminate it.
Medical evaluations for lung nodules often prioritize smoking history to guide decisions about further testing, such as CT scans or biopsies.
Family Medical History
A family history of lung cancer or other respiratory diseases contributes to lung nodule risk. Individuals with immediate relatives diagnosed with lung cancer tend to have a higher probability of developing malignant nodules themselves.
Genetic predispositions can influence how lung tissue responds to damage or carcinogens. This background is important when assessing nodules, even in non-smokers.
Physicians consider family history alongside other factors to decide on monitoring frequency and diagnostic procedures.
Exposure to Environmental Toxins
Repeated or prolonged exposure to substances like asbestos, radon, or industrial chemicals elevates risk. These toxins can cause lung tissue abnormalities that appear as nodules on imaging.
People working in mining, construction, or industries using hazardous materials have higher exposure levels. Residential exposure to radon gas is also notable, especially in certain geographic areas.
Environmental risk is evaluated along with personal and family history to determine the urgency of nodule investigation.
Benign vs. Malignant Lung Nodules
Lung nodules can be either benign or malignant, and distinguishing between the two is crucial for managing patient care. Certain features strongly suggest a nodule is harmless, while other indicators raise suspicion of cancer.
Features Suggesting Benign Status
Benign nodules typically have smooth, well-defined edges and are often smaller than 8 millimeters. Calcification patterns, such as concentric or “popcorn” calcifications, frequently indicate a non-cancerous cause, like a healed infection.
Stable nodule size over two years on serial imaging strongly favors benignity. Nodules with a uniform density and no spiculated or irregular borders are also more likely to be non-malignant. Patient history, including lack of smoking or exposure to carcinogens, further supports a benign diagnosis.
Indicators of Possible Malignancy
Nodules larger than 8 millimeters, especially those with irregular, spiculated, or lobulated edges, warrant closer evaluation. Rapid growth over weeks to months is a concerning sign of cancer.
Non-calcified nodules, particularly those with heterogeneous density, increase suspicion. A personal or family history of lung cancer, smoking, or exposure to asbestos strongly correlates with malignant risk. PET scans showing increased metabolic activity also suggest malignancy and require biopsy for confirmation.
Treatment Options for Lung Nodules
Treatment varies based on nodule size, appearance, growth rate, and patient risk factors. Options include monitoring nodules, minimally invasive procedures for diagnosis or treatment, and surgery for suspicious or malignant nodules.
Active Surveillance Approach
Active surveillance is the preferred first step for most small, stable lung nodules. This involves scheduled CT scans at set intervals, typically every 3 to 12 months, to track any changes in size or density.
This approach minimizes unnecessary procedures and focuses on early detection of growth or changes that may indicate malignancy. Patients with low-risk nodules and no symptoms are usually candidates. Guidelines from medical societies inform the frequency and duration of imaging based on nodule characteristics.
Minimally Invasive Procedures
Minimally invasive procedures are used when a definitive diagnosis is needed or when nodules exhibit suspicious features, but surgery is not immediately warranted. Common methods include needle biopsy via CT guidance or bronchoscopy.
These procedures allow tissue sampling with low complication risk, aiding in distinguishing benign from malignant nodules. Depending on the nodule’s location, either needle biopsy or endobronchial techniques are selected to maximize diagnostic yield and patient safety.
Surgical Intervention
Surgical intervention is reserved for nodules that are growing, have high-risk features, or are confirmed malignancies. Surgery ranges from wedge resection or segmentectomy to more extensive lobectomy, depending on nodule size and location.
Pre-surgical evaluation includes imaging and pulmonary function tests to assess operability. Surgery offers the best chance for a cure in malignant cases and can be curative when nodules are localized cancers.
FAQs About Lung Nodules
What Size of Lung Nodule Is Worrisome?
Lung nodules smaller than 6 millimeters are usually considered low risk and often require minimal follow-up. Nodules between 6–8 millimeters are more concerning and typically warrant periodic CT scans to monitor for growth. Nodules larger than 8–10 millimeters are considered more worrisome, as they have a higher chance of being malignant, especially if they change in size or appearance over time.
Note: While size is an important factor, other aspects, such as shape, borders, and patient history, also influence risk assessment.
What Are the Symptoms of a Cancerous Lung Nodule?
Most lung nodules cause no symptoms and are detected incidentally on imaging. However, a cancerous lung nodule may be associated with warning signs. These include a persistent cough, coughing up blood, unexplained weight loss, chest pain, or shortness of breath.
Fatigue and recurrent respiratory infections can also occur in some cases. If these symptoms are present, especially in someone with risk factors like smoking history or family history of lung cancer, prompt medical evaluation is recommended to rule out malignancy.
How Fast Can Lung Nodules Turn Into Cancer?
The speed at which a lung nodule becomes cancerous depends on multiple factors, including the type of cancer and patient risk profile. Malignant nodules often show measurable growth within months, sometimes doubling in size in 1–6 months.
By contrast, benign nodules typically remain stable for years. A nodule that does not change over two years is generally considered noncancerous. This is why regular follow-up imaging is important. Rapidly growing nodules raise suspicion for malignancy and may require biopsy or other diagnostic tests.
Can You Live a Normal Life With Lung Nodules?
Yes, many people live normal, healthy lives with lung nodules. The majority of nodules are benign and never cause problems. Even when nodules require monitoring, regular imaging ensures early detection of any concerning changes. For small, stable nodules, no treatment may be needed, and they often remain harmless for life.
While the initial discovery may cause anxiety, understanding the low risk in most cases and following your doctor’s recommendations allows patients to continue daily activities without significant limitations or disruptions.
Can Cancerous Lung Nodules Decrease in Size?
Cancerous lung nodules usually grow over time rather than shrink. However, in rare cases, they may temporarily decrease in size, which can complicate diagnosis. Shrinking nodules are more often linked to benign causes such as infections, inflammation, or treatment with antibiotics.
Cancer treatment, including chemotherapy, radiation, or targeted therapy, can also reduce the size of malignant nodules. Still, any decrease in size requires careful follow-up, as cancerous nodules can fluctuate but later resume growth. Regular imaging helps track these changes accurately.
Are Most Lung Nodules Cancerous?
No, most lung nodules are not cancerous. In fact, the majority are benign and result from old infections, scar tissue, or inflammatory conditions. Studies show that fewer than 5% of all detected nodules turn out to be malignant. The likelihood of cancer increases with larger size, irregular shape, spiculated edges, or when risk factors such as smoking and older age are present.
Note: Because most nodules are harmless, doctors often recommend follow-up imaging instead of immediate invasive procedures, unless suspicious features are seen.
Do Lung Nodules Always Turn Into Cancer?
No, lung nodules do not always turn into cancer. In fact, most never do. Benign nodules caused by infections, inflammation, or noncancerous growths typically remain stable over time without transforming into malignancy. Even when nodules require follow-up, stability over a two-year period usually confirms a benign nature.
Cancerous transformation is relatively uncommon and is more likely when nodules are larger, irregular, or growing. This is why ongoing monitoring through imaging is essential—to distinguish between harmless nodules and those requiring intervention.
Final Thoughts
Discovering a lung nodule can be unsettling, but it’s important to remember that most are benign and never lead to serious health problems. The key is not to panic but to stay informed and follow through with your doctor’s recommendations for monitoring or further testing.
Factors such as the nodule’s size, appearance, growth pattern, and your individual risk profile help determine whether concern is warranted.
By understanding when to worry about lung nodules and when they are likely harmless, you can take an active role in your health while avoiding unnecessary stress. Early evaluation and regular follow-up provide peace of mind and the best chance for addressing any potential problems promptly.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Loverdos K, Fotiadis A, Kontogianni C, Iliopoulou M, Gaga M. Lung nodules: A comprehensive review on current approach and management. Ann Thorac Med. 2019.