A collapsed lung, medically known as a pneumothorax, is a serious condition that occurs when air leaks into the space between the lung and chest wall, causing the lung to deflate. This can happen suddenly and without warning, leading to chest pain, difficulty breathing, and in severe cases, life-threatening complications.
Whether caused by injury, underlying lung disease, or occurring spontaneously, a collapsed lung requires prompt medical attention.
But how long can someone actually survive with this condition? In this article, we’ll explore the factors that influence survival, the importance of timely treatment, and what to expect during recovery.
Download our free guide that has over 100+ of the best tips for healthy lungs.
How Long Can You Live With a Collapsed Lung?
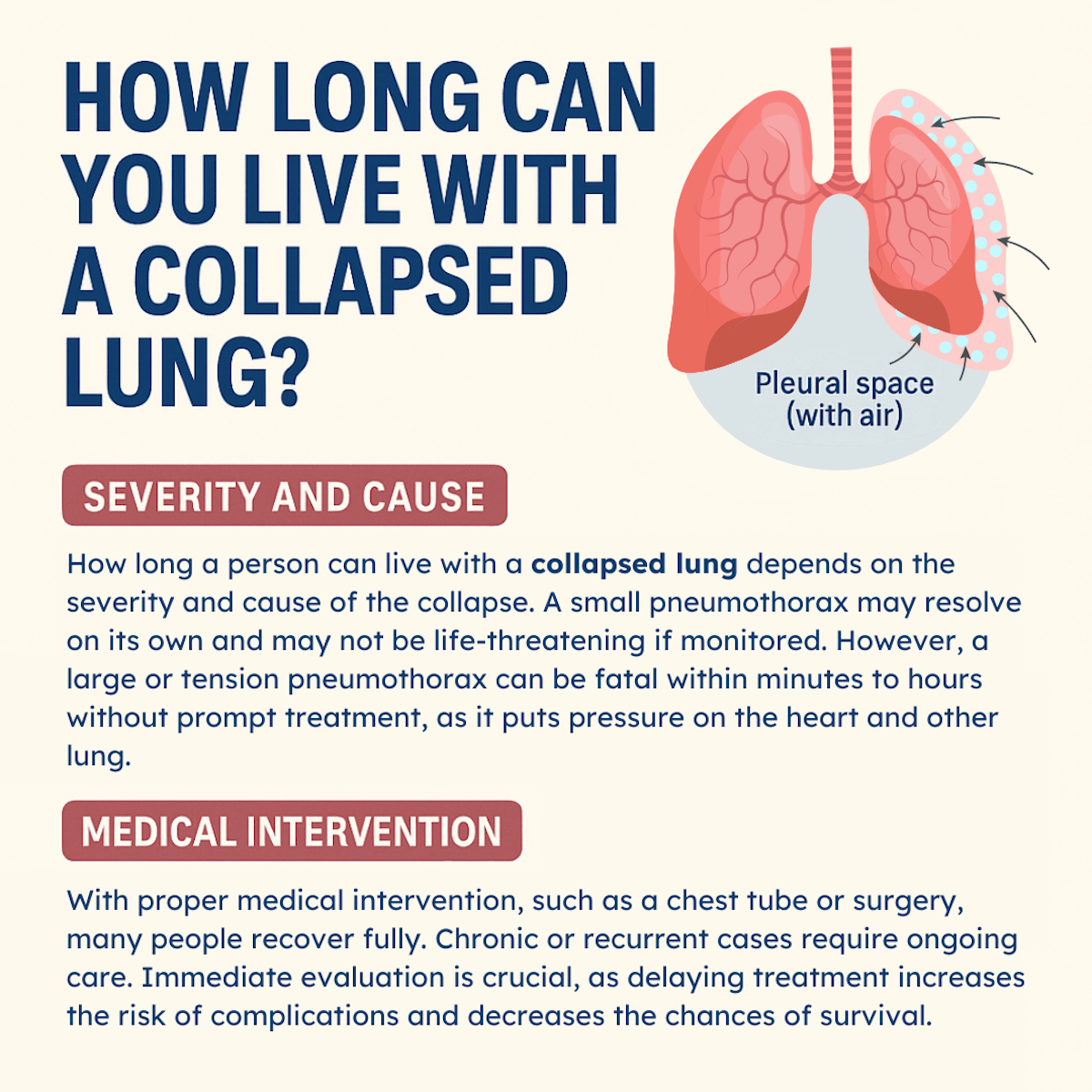
How long a person can live with a collapsed lung depends on the severity and cause of the collapse. A small pneumothorax may resolve on its own and may not be life-threatening if monitored. However, a large or tension pneumothorax can be fatal within minutes to hours without prompt treatment, as it puts pressure on the heart and other lung.
With proper medical intervention, such as a chest tube or surgery, many people recover fully. Chronic or recurrent cases require ongoing care. Immediate evaluation is crucial, as delaying treatment increases the risk of complications and decreases the chances of survival.
What is a Pneumothorax?
A pneumothorax occurs when the pleural space, the thin gap between the lung and the chest wall, fills with air or gas. Normally, this space contains only a small amount of fluid that helps the lungs move smoothly during breathing. When air enters this space, it creates pressure that prevents the lung from expanding properly, leading to collapse.
There are several types of pneumothorax, each with different implications for survival and treatment urgency:
- Spontaneous pneumothorax occurs without any obvious cause or injury, often affecting tall, thin young men or people with underlying lung conditions.
- Traumatic pneumothorax results from chest injuries, such as those sustained in car accidents, falls, or penetrating wounds.
- Tension pneumothorax represents the most dangerous form, where increasing pressure in the chest cavity compresses the heart and major blood vessels, creating a medical emergency.
Immediate Survival Factors
The question of how long someone can survive with a collapsed lung depends on multiple critical factors. The size of the collapse plays a fundamental role in determining both symptoms and survival time.
A small pneumothorax affecting less than 20% of the lung may cause minimal symptoms and can sometimes resolve on its own over days or weeks. However, a large collapse affecting 50% or more of the lung creates severe breathing difficulties and requires immediate medical intervention.
The type of pneumothorax has a significant impact on survival expectations. Simple pneumothorax, while serious, typically allows for survival measured in hours to days with appropriate medical care. Tension pneumothorax, however, can be fatal within minutes to hours if left untreated, as it progressively compresses vital structures in the chest cavity.
An individual’s health status before the collapse significantly influences their survival prospects. Young, healthy individuals with strong cardiovascular systems can often compensate better for reduced lung function compared to elderly patients or those with pre-existing heart or lung conditions. People with chronic obstructive pulmonary disease (COPD), asthma, or heart disease face greater risks and shorter survival times without treatment.
Physiological Impact on the Body
When a lung collapses, the body initiates several compensatory mechanisms to maintain adequate oxygen delivery to vital organs. The unaffected lung must work harder to provide sufficient oxygenation, while the heart increases its rate to pump blood more efficiently through the remaining functional lung tissue. These compensatory responses can sustain life temporarily but become increasingly ineffective as the collapse worsens or time progresses.
The cardiovascular system bears significant strain during pneumothorax. In tension pneumothorax, the mediastinum—the central chest area containing the heart and major blood vessels—shifts away from the affected side. This displacement can compress the vena cava, reducing blood return to the heart and potentially causing cardiovascular collapse. Without immediate intervention, this progression can lead to cardiac arrest within 30 minutes to several hours.
Oxygen saturation levels provide crucial indicators of survival prospects. While healthy individuals can initially maintain adequate oxygen levels with a moderate pneumothorax, severe cases quickly lead to hypoxemia, dangerously low blood oxygen levels. When oxygen saturation drops below 90%, cellular function begins to deteriorate, and the likelihood of organ damage increases.
Treatment Approaches and Their Impact on Survival
Medical treatment significantly improves the survival prospects for patients with pneumothorax. Small, spontaneous pneumothoraces may be managed conservatively with careful monitoring and supplemental oxygen. This approach, called “watchful waiting,” relies on the body’s natural ability to reabsorb the trapped air over time, typically requiring several days to weeks for complete resolution.
Moderate to large pneumothoraces usually require active intervention to remove trapped air and re-expand the lung. Needle aspiration involves inserting a large needle or small catheter into the chest cavity to withdraw air, providing rapid relief in many cases. This procedure can be life-saving when performed promptly, often restoring normal breathing within minutes.
Chest tube insertion represents the most common treatment for significant pneumothorax. A plastic tube is placed through the chest wall into the pleural space, allowing continuous drainage of air and monitoring of lung re-expansion. This procedure typically requires hospitalization for several days while the lung heals and the tube can be safely removed.
Emergency situations, particularly tension pneumothorax, may require immediate decompression through needle thoracostomy. This life-saving procedure involves inserting a large-bore needle into the chest to release pressure, buying time for more definitive treatment. When performed correctly within minutes of recognition, this intervention can mean the difference between life and death.
Long-term Survival and Recovery
With appropriate treatment, most people with pneumothorax can achieve complete recovery and return to a normal life expectancy. However, recurrence rates vary significantly depending on the underlying cause. Primary spontaneous pneumothorax has a recurrence rate of approximately 25-30% after the first episode, increasing to 50-80% after subsequent episodes.
Surgical intervention may be recommended for recurrent pneumothorax to prevent future episodes. Video-assisted thoracoscopic surgery (VATS) allows surgeons to repair blebs or bullae—weak spots on the lung surface that commonly cause spontaneous collapse. This minimally invasive procedure significantly reduces recurrence rates to less than 5% while preserving long-term lung function.
Recovery time varies based on the size of the collapse and treatment method. Small pneumothoraces managed conservatively may resolve within 1-2 weeks, while those requiring chest tube drainage typically heal within 3-7 days of tube placement. Surgical patients typically experience longer recovery periods of 2-4 weeks but benefit from a dramatically reduced risk of recurrence.
Risk Factors and Prevention
Understanding risk factors helps identify individuals at higher risk for pneumothorax and potentially fatal complications. Smoking significantly increases the risk of a spontaneous pneumothorax, particularly in tall, thin young men. Certain genetic conditions, such as Marfan syndrome or alpha-1 antitrypsin deficiency, predispose individuals to lung weakness and increased collapse risk.
Occupational and recreational activities can increase the risk of a pneumothorax. Scuba diving poses particular dangers, as rapid pressure changes during ascent can cause lung rupture in susceptible individuals. Flying in unpressurized aircraft or traveling to high altitudes may trigger pneumothorax in people with underlying lung conditions.
Medical procedures occasionally cause an iatrogenic pneumothorax, particularly those involving the chest or neck. Central line placement, lung biopsy, and mechanical ventilation all carry small but significant risks of causing lung collapse. Healthcare providers must remain vigilant for signs of pneumothorax during and after these procedures.
Warning Signs and When to Seek Help
Recognizing the symptoms of a pneumothorax can be life-saving, as early treatment dramatically improves outcomes. Sudden, sharp chest pain accompanied by shortness of breath represents the classic presentation of a heart attack. The pain typically occurs on one side of the chest and may worsen with deep breathing or coughing.
Progressive difficulty breathing, particularly when accompanied by a rapid heart rate, bluish discoloration of the skin, or anxiety, suggests a worsening pneumothorax that requires immediate medical attention. These symptoms indicate that the body’s compensatory mechanisms are failing to maintain adequate oxygenation.
A tension pneumothorax presents with additional alarming signs, including severe difficulty breathing, rapid deterioration in mental status, and signs of shock, such as low blood pressure and weak pulse. This constellation of symptoms represents a true medical emergency requiring immediate intervention to prevent death.
Prognosis and Quality of Life
The long-term prognosis for patients with pneumothorax is generally excellent with appropriate treatment. Most individuals return to normal activities within weeks of recovery, with no lasting impact on lung function or exercise capacity. However, those with recurrent episodes may experience some anxiety about future occurrences, potentially affecting quality of life.
Certain activities may require modification after a pneumothorax, particularly for those at high risk of recurrence. Scuba diving is generally contraindicated after spontaneous pneumothorax unless surgical treatment has been performed. Air travel is typically safe once the lung has fully re-expanded and healed, though some physicians recommend waiting 2-6 weeks after resolution.
FAQs About Surviving With a Collapsed Lung
How Long Can You Stay Alive With a Collapsed Lung?
The length of survival depends on the severity and type of the collapsed lung. A small pneumothorax may allow someone to live for days or even weeks if untreated, though symptoms may persist. However, a large or tension pneumothorax can become life-threatening within minutes to hours without immediate medical intervention.
Survival time is significantly improved with prompt treatment, such as oxygen therapy, needle aspiration, or chest tube placement. Early diagnosis is crucial to avoid serious complications or death.
How Does a Collapsed Lung Feel?
A collapsed lung often causes sudden, sharp chest pain that worsens with breathing or coughing. It’s usually felt on one side of the chest. Many people also experience shortness of breath, a rapid heart rate, or a feeling of tightness or pressure.
In more severe cases, symptoms may include lightheadedness, fatigue, anxiety, or a bluish discoloration of the skin due to low oxygen levels. These sensations can develop rapidly and should be treated as a medical emergency if they worsen.
What Helps a Collapsed Lung Heal Faster?
Timely medical intervention is crucial for faster healing. For small pneumothoraces, rest and supplemental oxygen may be enough. For larger cases, procedures like needle aspiration or chest tube insertion help re-expand the lung.
Avoiding physical exertion, following the doctor’s instructions, staying hydrated, and refraining from smoking can also support recovery. In some cases, surgery may be necessary to prevent recurrence.
Note: Regular follow-ups and imaging help ensure that the lung heals properly over time.
What Not to Do After a Collapsed Lung?
After a collapsed lung, avoid strenuous physical activities, heavy lifting, or flying in unpressurized aircraft until cleared by your doctor. These activities can increase chest pressure and increase the risk of recurrence. Do not smoke, as it delays healing and raises the chance of another collapse.
Also, avoid scuba diving unless you’ve had surgical treatment and full clearance. Follow all post-treatment instructions, attend follow-up visits, and notify your healthcare provider if symptoms return.
Can A Collapsed Lung Cause Permanent Damage?
In most cases, a collapsed lung heals completely with proper treatment, leaving no lasting damage. However, if the condition is severe, recurrent, or left untreated, it can lead to complications such as scarring, reduced lung function, or chronic breathing issues.
People with underlying lung diseases like COPD are at greater risk for long-term effects. Surgical interventions can reduce the risk of recurrence and preserve lung function, but each case varies depending on the individual’s overall health.
Can A Collapsed Lung Kill You?
Yes, a collapsed lung can be fatal if not treated, especially in the case of a tension pneumothorax. This form rapidly increases pressure in the chest, which can compress the heart and other lung, leading to shock and death within minutes to hours.
Even less severe cases can be dangerous if left unmanaged. However, with prompt medical attention, the majority of people survive and recover fully. Recognizing symptoms early and seeking emergency care is essential for a good outcome.
Can A Collapsed Lung Really Heal Itself?
A small, uncomplicated pneumothorax can sometimes heal on its own without invasive treatment. The body can gradually reabsorb the trapped air over a few days to weeks, especially with the aid of supplemental oxygen.
However, larger collapses typically require medical procedures such as needle aspiration or chest tube insertion to remove the air and re-expand the lung. Even if it seems minor, a doctor should always evaluate any suspected collapsed lung to determine the best course of action.
Can A Pneumothorax Be Prevented?
While not all pneumothoraces can be prevented, certain actions can reduce the risk. Avoid smoking, as it significantly increases the likelihood of lung collapse. If you have a history of pneumothorax, your doctor may recommend surgery to prevent recurrence. People with underlying lung disease should manage their condition carefully.
Avoid high-risk activities, such as scuba diving or flying at high altitudes, without obtaining medical clearance. Prompt treatment of chest injuries and careful monitoring after certain medical procedures also help prevent this condition.
Final Thoughts
The survival time with a collapsed lung varies dramatically based on the size and type of collapse, individual health factors, and access to medical care. While small pneumothoraces may allow survival for days to weeks, large or tension pneumothorax can be fatal within hours without treatment. The key to achieving optimal outcomes lies in the rapid recognition of symptoms, prompt medical intervention, and comprehensive follow-up care.
Understanding pneumothorax empowers individuals to recognize warning signs and seek timely medical attention. With modern medical treatment, the vast majority of patients with pneumothorax achieve complete recovery and return to a normal, healthy life.
However, the potential for rapid deterioration in untreated cases underscores the critical importance of immediate medical evaluation for anyone experiencing sudden chest pain and breathing difficulties.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- McKnight CL, Burns B. Pneumothorax. [Updated 2023 Feb 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.