The idea of donating a lung to save the life of a loved one is a powerful and selfless gesture. For families facing the devastating effects of end-stage lung disease, the question often arises: Can you donate a lung to a family member?
While full lung donation isn’t possible from a living person, medical advancements have made partial lung transplants a rare but potential option in certain cases. However, this procedure comes with strict requirements and is only available at select transplant centers.
In this article, we’ll explore how living donor lung transplants work, who qualifies, and what it takes to become a donor for a family member in need.
Download our free guide that has over 100+ of the best tips for healthy lungs.
Can You Donate a Lung to a Family Member?
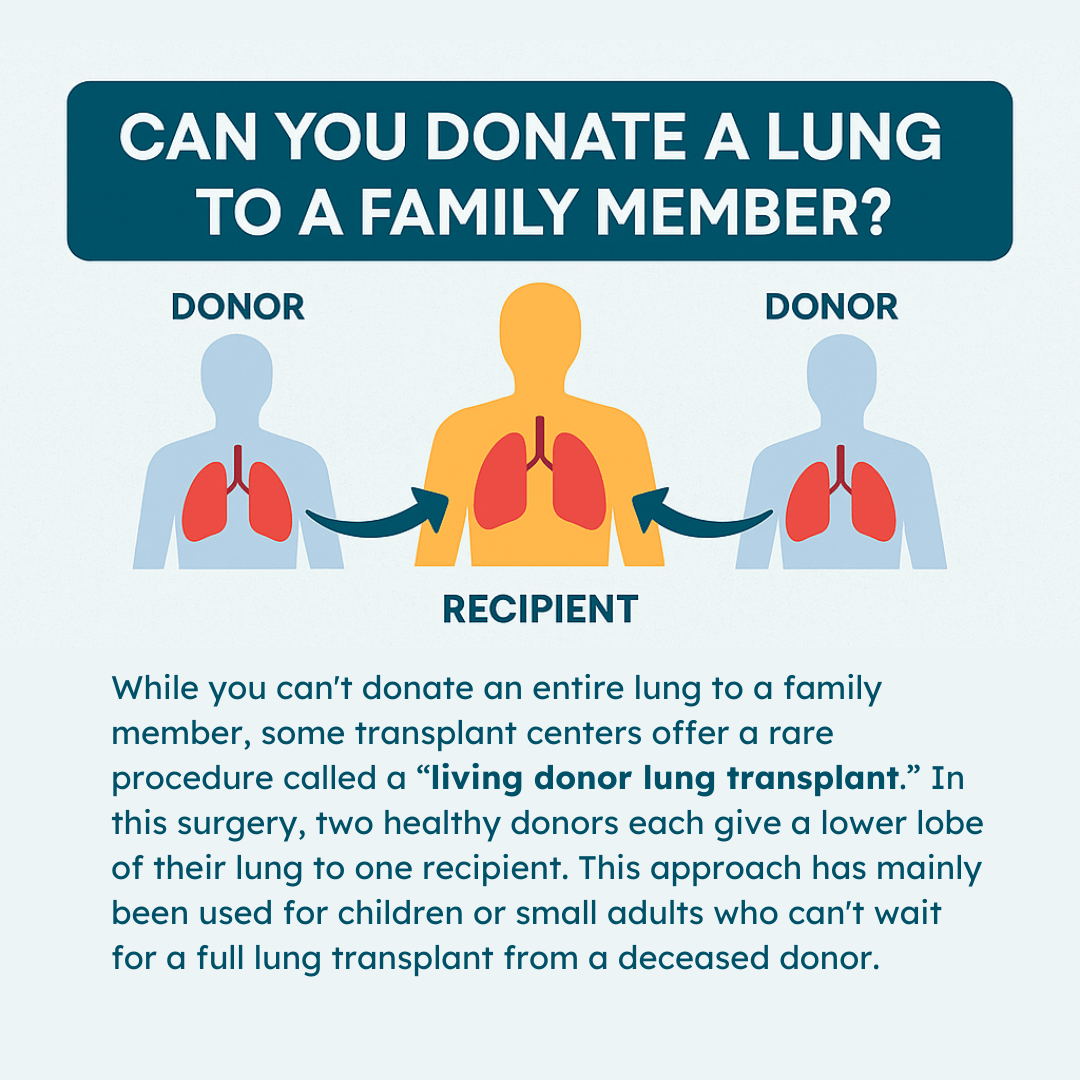
While you can’t donate an entire lung to a family member, some transplant centers offer a rare procedure called a “living donor lung transplant.” In this surgery, two healthy donors each give a lower lobe of their lung to one recipient. This approach has mainly been used for children or small adults who can’t wait for a full lung transplant from a deceased donor.
However, it’s not widely available, and strict criteria must be met, including having two compatible donors. Not all hospitals perform this procedure; therefore, it’s essential to consult with a transplant center to determine eligibility. If you’re considering a donation, thorough testing for tissue compatibility and overall health is required for all potential donors.
How Living Donor Lung Transplants Work
A living donor lung transplant is a complex and highly specialized procedure. Unlike deceased donor transplants, where an entire lung may be used, this surgery involves transplanting two lower lung lobes—one from each of two living donors—into a single recipient. The right lung has three lobes (upper, middle, and lower), while the left has two (upper and lower).
In this procedure, each donor typically contributes one lower lobe, which is sufficient to provide adequate lung function in the recipient.
Once the lobes are removed from the donors, they are immediately transplanted into the recipient during the same surgical session. Over time, the donated lobes adapt and compensate for the missing lung volume, allowing the recipient to breathe more effectively. However, it’s important to note that this procedure doesn’t restore full lung capacity—it improves quality of life and extends survival, but doesn’t offer the same function as two healthy, native lungs.
Because this surgery involves three people—two donors and one recipient—it requires extensive coordination, careful planning, and a surgical team with specialized expertise. The risks are significant for everyone involved, so this option is only considered when the potential benefits clearly outweigh the risks, and no suitable deceased donor organs are available in time.
Who Is Eligible for a Living Donor Lung Transplant?
Living donor lung transplants are not a routine option and are only considered under very specific conditions. The recipient must have end-stage lung disease and be unable to wait for a deceased donor transplant due to the severity of their condition.
This is most often the case in pediatric patients or adults with rapidly progressing diseases such as cystic fibrosis or pulmonary fibrosis.
Potential donors must also meet strict criteria. Typically, donors are close family members or individuals with a strong emotional bond to the recipient, but a biological relationship is not required. What matters most is medical compatibility. Each donor must:
- Be in excellent physical health
- Be between the ages of 18 and 60
- Have a compatible blood type and tissue match
- Be a non-smoker with healthy lung function
- Pass comprehensive physical and psychological evaluations
In addition to medical suitability, donors must be fully informed and willing to participate voluntarily. Because the procedure is not without risk—including pain, infection, or reduced lung capacity after donation—doctors must ensure the decision is made freely and without pressure.
Note: Even if all medical criteria are met, the final decision lies with the transplant team at a specialized center. They will evaluate the overall health and safety of everyone involved before proceeding.
Risks and Recovery for Living Lung Donors
Although living donor lung transplantation can be life-saving for the recipient, it’s important to understand that the surgery carries risks for the donors as well. Removing a lung lobe is a major operation that involves general anesthesia, surgical incisions, and a hospital stay. The most common risks for donors include:
- Postoperative pain and discomfort
- Bleeding or infection
- Reduced lung function
- Blood clots
- Pneumonia or other respiratory complications
While most healthy individuals can live with a reduced lung volume, some donors may experience a decline in stamina or shortness of breath, especially during physical exertion. Long-term studies suggest that the majority of donors return to their normal daily activities, but careful monitoring and follow-up care are essential to ensure a full recovery.
Recovery time varies, but most donors stay in the hospital for about a week and need several weeks to a few months before resuming normal activities. Emotional health is also an important factor, and psychological support may be recommended, especially since donors are taking on risk for someone else’s benefit.
Note: Despite these challenges, many donors report a deep sense of fulfillment, especially when the transplant leads to a successful outcome for their loved one. Still, it’s a decision that requires careful consideration, strong support systems, and open communication with the medical team.
Benefits and Challenges for the Recipient
For the transplant recipient, a living donor lung transplant can be a second chance at life, especially when time is running out and a deceased donor lung is not available. Recipients of living donor lobes often experience improved breathing, increased energy, and better quality of life. These benefits can be life-changing, especially for children or small adults who previously struggled with severe lung disease.
However, it’s important to acknowledge that this type of transplant is not a cure. Recipients must take lifelong immunosuppressant medications to prevent rejection of the transplanted lobes.
These drugs weaken the immune system, increasing the risk of infections and other complications. Regular follow-up care, including lung function tests, imaging, and blood work, is essential to monitor for signs of rejection or other complications.
Another challenge is the size of the lobes. Since adult donors provide only a portion of their lungs, the fit must be just right, especially for pediatric patients. In some cases, the transplanted lobes may not fully meet the recipient’s oxygen demands, although the body can adapt over time.
The Role of Transplant Centers and Availability
Not every hospital or transplant center is equipped to perform living donor lung transplants. This highly specialized procedure requires a skilled and experienced surgical team, as well as a facility equipped with advanced resources. Only a handful of centers worldwide routinely perform this type of surgery, and most are located in major academic or research hospitals.
Because of the complexity and the need for two healthy donors, living donor lung transplants are typically considered a last-resort option. The procedure is most commonly used when:
- A suitable deceased donor organ is unlikely to become available in time
- The recipient’s condition is rapidly deteriorating
- Two willing and medically suitable donors are identified
Patients and their families considering this option must undergo an extensive evaluation process at a qualified transplant center. This includes not only medical testing but also discussions with transplant coordinators, social workers, psychologists, and ethics committees. The decision to proceed is never taken lightly.
In the United States, living donor lung transplants are still relatively rare. Most lung transplants are performed using lungs from deceased donors. That said, ongoing research and surgical advancements continue to improve outcomes, and select centers remain open to performing these procedures in urgent and appropriate cases.
Note: If you’re exploring this path, it’s crucial to reach out early to a recognized transplant center, ask detailed questions, and understand the full scope of what’s involved.
Ethical Considerations and Emotional Impact
Donating a lung lobe to a family member is not only a medical decision but also an emotional and ethical one. It involves a deep personal commitment, and the process can be emotionally intense for both the donor and recipient. While many donors are driven by love and a desire to help, transplant teams are careful to ensure the decision is voluntary and free from pressure or guilt.
Psychological evaluations are part of the donor screening process to assess mental readiness, emotional stability, and motivations. Transplant teams want to ensure that donors fully understand the risks and are prepared for the recovery process. They also evaluate the family dynamic to make sure the donor’s decision isn’t influenced by unrealistic expectations or unspoken obligations.
For recipients, the emotional weight can also be significant. While receiving a life-saving gift is uplifting, some experience feelings of guilt or anxiety, especially if the donor experiences complications. Ongoing counseling and support are often recommended for both parties before and after surgery.
Support groups, transplant social workers, and therapy can help families navigate these challenges, offering a space to discuss fears, expectations, and hopes. Clear communication, realistic planning, and emotional support are all key to making the process as smooth and positive as possible.
Final Thoughts
Living donor lung transplants are a remarkable example of how medical science and human generosity can come together to save lives. While not a common procedure, they represent a viable option in certain life-threatening situations, particularly when time is short and two willing, healthy donors are available.
If you’re considering donating a lung lobe to a family member, start by consulting with a reputable transplant center. Be prepared for an extensive evaluation process, and surround yourself with a strong support system.
Whether you’re a potential donor or recipient, understanding the medical, emotional, and logistical aspects of the journey can help you make informed, empowered decisions.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Date H. Living-related lung transplantation. J Thorac Dis. 2017.