Auscultation is one of the oldest and most valuable techniques in clinical medicine, particularly within the field of respiratory care. For respiratory therapists, physicians, and other healthcare professionals, the act of listening to the body’s internal sounds provides direct insight into the function of the lungs, heart, and airways.
Despite advances in imaging and diagnostic technologies, auscultation remains an essential skill because of its immediacy, simplicity, and effectiveness in bedside assessment.
This article explores what auscultation is, the principles behind it, how it is performed, and why it remains highly relevant to respiratory therapists and the broader field of respiratory care.
What is Auscultation?
Auscultation is the process of listening to the internal sounds of the body, typically using a stethoscope. The word is derived from the Latin auscultare, meaning “to listen.” In respiratory care, auscultation focuses mainly on breath sounds within the lungs and airways, although it is also used to assess the heart and blood flow in major vessels.
When a clinician places the diaphragm or bell of the stethoscope against the chest wall, they are able to detect the movement of air, the turbulence of airflow, and any abnormal sounds produced by diseased lungs or obstructed airways. These sounds are then interpreted to guide diagnosis, treatment, and monitoring of a patient’s respiratory condition.
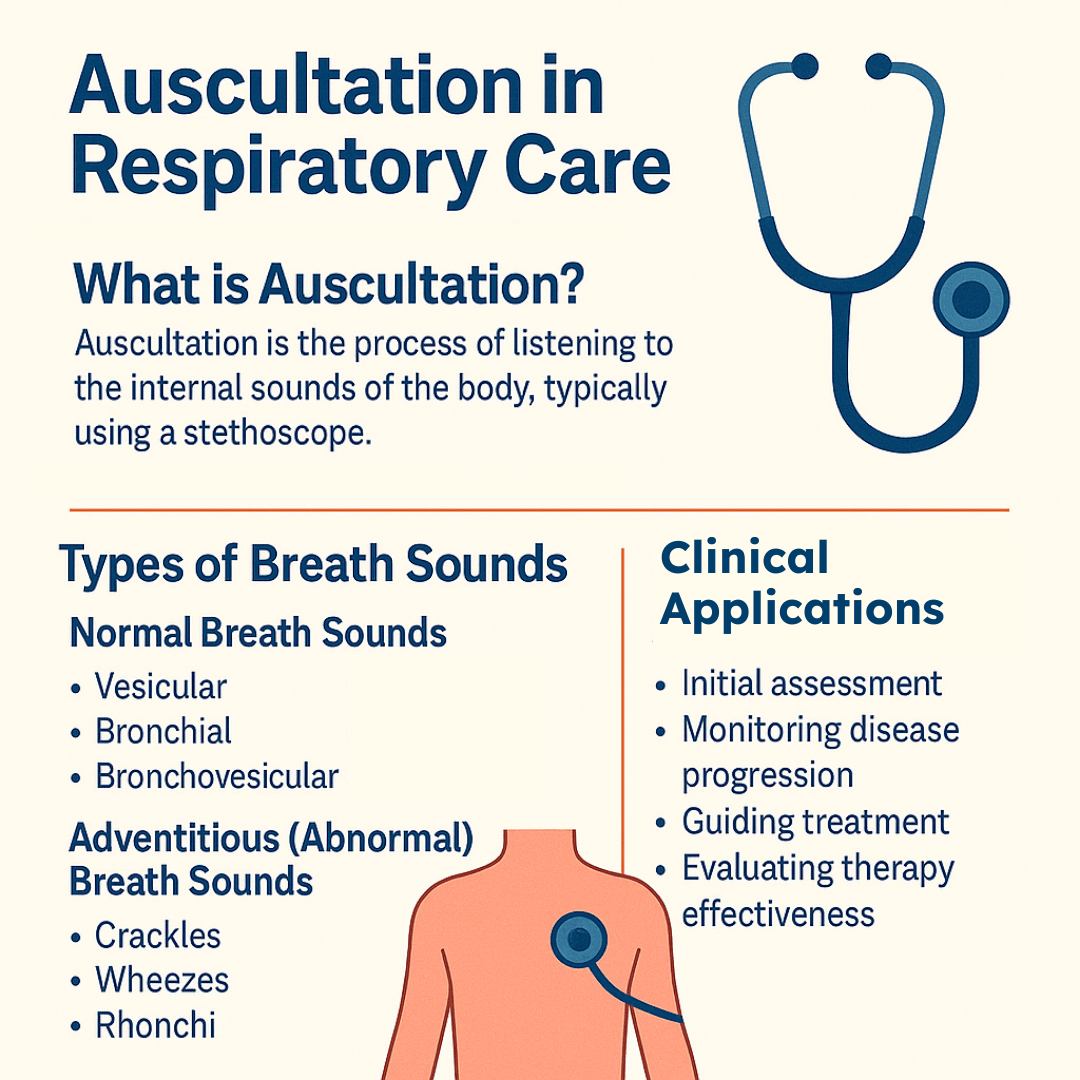
Types of Breath Sounds
The sounds detected during auscultation arise from airflow through the respiratory tract and its interaction with lung tissue, secretions, and occasionally fluid within the airways. These sounds can be broadly divided into normal breath sounds and adventitious (abnormal) breath sounds.
Recognizing the differences is a vital skill for respiratory therapists, as each type of sound provides valuable clues about a patient’s underlying condition.
Normal Breath Sounds
Normal breath sounds are those typically heard in healthy lungs and vary depending on where the stethoscope is placed.
- Vesicular breath sounds are soft, low-pitched, and heard over the majority of the lung fields, particularly in the peripheral areas. They represent the gentle rustling of air as it moves in and out of the alveoli.
- Bronchial breath sounds, by contrast, are louder and higher-pitched. These are normally heard only over the trachea, where airflow is more turbulent. If bronchial sounds are heard in peripheral lung fields, it may indicate consolidation, as seen in pneumonia.
- Bronchovesicular breath sounds fall between the two extremes, with a moderate pitch and intensity. These are usually heard in the central chest region, near the sternum or between the scapulae, where larger airways are located.
Adventitious (Abnormal) Breath Sounds
Adventitious sounds suggest an underlying abnormality and are key indicators of respiratory pathology.
- Crackles, also called rales, are discontinuous popping or bubbling noises that often occur when collapsed alveoli or fluid-filled airspaces suddenly open during inspiration. They are common in conditions such as pneumonia, pulmonary fibrosis, or congestive heart failure.
- Wheezes are high-pitched, musical sounds produced by narrowed or obstructed airways, frequently associated with asthma or COPD.
- Rhonchi are low-pitched, snoring-like sounds that result from secretions in larger airways and often clear with coughing.
- Stridor is a harsh, high-pitched sound heard primarily during inspiration and typically signals a serious upper airway obstruction, such as croup or foreign body aspiration.
- Pleural friction rub is a coarse, grating sound caused by inflamed pleural surfaces rubbing together, often linked to pleurisy or pulmonary embolism.
Note: By carefully identifying these sounds, respiratory therapists can distinguish between normal physiology and pathology, evaluate the severity of disease, and monitor how patients respond to treatment interventions.
How to Perform Auscultation
Auscultation requires both technical skill and attentive listening. Respiratory therapists typically follow these steps:
Preparation
- Ensure a quiet environment.
- Use a high-quality stethoscope.
- Position the patient sitting upright when possible, with the chest exposed for optimal contact.
Technique
- Place the stethoscope diaphragm firmly against the skin (not over clothing).
- Instruct the patient to take deep, slow breaths through an open mouth.
- Move systematically from one area of the chest to another, comparing sounds between the left and right sides.
Areas to Examine
- Anterior chest (upper, middle, and lower zones).
- Lateral chest (sides of the lungs).
- Posterior chest (upper, middle, and lower back).
Note: By covering all regions, the clinician ensures that localized abnormalities are not missed.
Clinical Applications in Respiratory Therapy
For respiratory therapists, auscultation is not just a routine procedure—it is a vital diagnostic and monitoring tool. Its applications include:
1. Initial Assessment
Auscultation is one of the first steps in evaluating a patient with respiratory distress. It helps identify whether the problem involves obstruction, infection, fluid accumulation, or restricted airflow.
2. Monitoring Disease Progression
Conditions such as asthma, COPD, pneumonia, and pulmonary edema change the quality of breath sounds over time. Serial auscultations allow therapists to detect worsening or improving lung function.
3. Guiding Treatment
The presence of wheezes may suggest the need for bronchodilators, while crackles may point to fluid overload requiring diuretics. Stridor may signal a critical airway emergency needing immediate intervention.
4. Evaluating Therapy Effectiveness
After treatments such as suctioning, bronchodilator therapy, or mechanical ventilation adjustments, auscultation confirms whether the intervention was successful.
5. Assessing Artificial Airways and Ventilated Patients
In intubated patients, auscultation helps verify endotracheal tube placement, detect complications such as unilateral ventilation, and evaluate ventilator settings’ impact on lung aeration.
Auscultation Practice Questions
1. What is auscultation?
The act of listening to internal body sounds, such as those from the heart and lungs, to assist in diagnosing medical conditions
2. Why is auscultation performed during a respiratory assessment?
To complete the assessment and help localize or define potential pathology in the lungs
3. What term refers to the process of listening to bodily sounds with a stethoscope?
Auscultation
4. What are the four basic components of a stethoscope?
Bell, diaphragm, tubing, and earpieces
5. What is the purpose of the bell on a stethoscope?
To detect low-pitched sounds, such as heart murmurs and certain vascular sounds
6. Which part of the stethoscope is best suited for listening to lung sounds?
The diaphragm, because it is designed for detecting high-frequency sounds
7. What is the ideal tubing length of a stethoscope for optimal sound transmission?
Approximately 25–35 cm (11–16 inches) to reduce external noise interference
8. Why is it important to begin lung auscultation at the bases?
Because abnormal sounds in the lower lobes may only be heard after a few deep breaths
9. What key characteristics should be assessed during auscultation of breath sounds?
Pitch, intensity, and the duration of both inspiratory and expiratory phases
10. What type of breath sound is soft, muffled, and heard over the healthy lung parenchyma?
Vesicular breath sounds
11. How do vesicular breath sounds compare to bronchovesicular breath sounds?
They are lower in pitch and intensity, and primarily heard during inhalation with a short expiratory phase
12. Where are bronchovesicular breath sounds typically heard?
Around the upper sternum and between the scapulae
13. How do bronchovesicular breath sounds differ from tracheal breath sounds?
They are slightly lower in pitch with equal inspiratory and expiratory phases
14. What are tracheal breath sounds?
Loud, tubular sounds normally heard over the trachea
15. In tracheal breath sounds, how does the expiratory phase compare to the inspiratory phase?
It is equal to or slightly longer than the inspiratory phase
16. What term is used to describe a reduction in the intensity of breath sounds?
Diminished breath sounds
17. What does it mean when breath sounds are completely inaudible?
Absent breath sounds
18. What term describes increased intensity of breath sounds?
Harsh breath sounds
19. What are bronchial breath sounds?
Harsh breath sounds where the expiratory phase is equal to the inspiratory phase
20. What are adventitious lung sounds?
Abnormal added sounds such as crackles or wheezes produced by air moving through diseased airways
21. How are discontinuous adventitious lung sounds described?
As intermittent, crackling, or bubbling sounds of short duration
22. What is another name for discontinuous adventitious lung sounds?
Crackles or rales
23. What term describes continuous adventitious lung sounds?
Wheezes
24. What is a wheeze?
A continuous, high-pitched, musical sound typically associated with airway narrowing
25. What sound resembles snoring and is associated with secretions in larger airways?
Rhonchi (though this term is less commonly used today)
26. What condition may cause diminished or absent breath sounds in the lower lobes?
Pleural effusion, atelectasis, or severe emphysema
27. What condition often produces bilateral wheezes during auscultation?
Asthma or other obstructive airway diseases
28. What lung pathology is commonly associated with fine crackles heard at the bases?
Pulmonary fibrosis or early congestive heart failure
29. What does the presence of coarse crackles usually indicate?
Excess secretions or fluid in the larger airways
30. Why is auscultation a critical skill for respiratory therapists?
It helps detect and differentiate normal from abnormal lung sounds to guide treatment decisions
31. Which lung sound is often used synonymously with coarse crackles due to excessive secretions in the airways?
Rhonchi
32. What is a loud, high-pitched, continuous lung sound that may be heard without a stethoscope?
Stridor
33. Where is stridor most commonly auscultated?
Over the larynx and trachea during inhalation
34. Is stridor classified as a continuous or discontinuous adventitious lung sound?
Continuous
35. What does the presence of stridor typically indicate?
An obstruction in the trachea or larynx
36. In which patient population is stridor most frequently observed?
Infants and small children
37. During which phase of breathing is stridor most commonly heard?
Inspiration
38. What term describes faint, low-intensity crackles heard during auscultation?
Fine crackles
39. What type of crackles are more pronounced, louder, and suggest the presence of mucus in larger airways?
Coarse crackles
40. What are normal breath sounds primarily generated by?
Turbulent airflow in the larger airways
41. What causes diminished breath sounds during auscultation?
Reduced sound generation or decreased transmission through the lungs or chest wall
42. Why does shallow breathing reduce the intensity of breath sounds?
Because it creates less turbulent airflow in the larger airways
43. What are five possible causes of reduced sound transmission in the lungs?
Airway mucus plugs, hyperinflation, pleural effusion or pneumothorax, generalized edema (anasarca), and obesity or muscular chest wall
44. What two lung sounds indicate high-velocity airflow through narrowed airways?
Wheezes and stridor
45. What serious lung sound suggests that the upper airway is critically compromised?
Stridor
46. What is the most common cause of chronic stridor in infants?
Laryngomalacia
47. What is the most frequent cause of acute stridor in children?
Croup
48. What type of stridor suggests narrowing above the glottis?
Inspiratory stridor
49. What does expiratory stridor typically indicate?
Narrowing or obstruction in the lower trachea
50. In adults, what is the most common cause of stridor?
Laryngeal or subglottic edema due to airway trauma following prolonged intubation
51. What four characteristics are used to describe lung sounds?
Pitch, quality, intensity, and the duration of inspiratory and expiratory phases
52. What are tracheal and bronchial breath sounds typically described as?
Loud, tubular sounds heard over the trachea with a longer expiratory phase and a slight pause between phases
53. When bronchial sounds are heard over distal lung fields, what are they considered and what might they indicate?
They are considered abnormal and may indicate lung consolidation or compression
54. Where are vesicular breath sounds typically heard?
Over the peripheral lung fields in healthy individuals
55. How do vesicular breath sounds differ in phase duration?
They have a longer inspiratory phase than expiratory phase, with no pause between the two
56. What are adventitious breath sounds?
Abnormal lung sounds heard during inspiration and/or expiration that may be continuous or discontinuous
57. What lung sound is often described as musical and associated with asthma or bronchospasm?
Wheezing
58. What does the presence of fine inspiratory crackles at the lung bases commonly suggest?
Pulmonary fibrosis or early congestive heart failure
59. What condition might be suspected if coarse crackles are heard that clear with coughing?
Excess secretions in the airways such as in bronchitis
60. What abnormal breath sound may be heard in a patient with epiglottitis or upper airway swelling?
Stridor
61. What is the description of crackles (formerly rales) heard during auscultation?
Abnormal, discontinuous, high-pitched popping sounds, most often during inspiration, associated with restrictive or obstructive disorders
62. What do wet crackles typically indicate during auscultation?
Movement of fluid or secretions in the airways during inspiration
63. What do dry crackles usually result from?
The sudden opening of closed airways
64. Crackles heard in the latter half of inspiration are typically associated with which conditions?
Atelectasis, pulmonary fibrosis, pulmonary edema, or pleural effusion
65. Crackles caused by secretions are typically described as what?
Low-pitched sounds resembling hair being rubbed together, heard during inspiration and/or expiration
66. What type of crackles may pulmonary edema produce?
Fine crackles as air bubbles through fluid in the distal small airways
67. Crackles heard at the lung bases are often associated with which pathologies?
Interstitial lung disease, atelectasis, pneumonia, bronchiectasis, and pulmonary edema
68. What abnormal breath sound is described as a dry, crackling sound heard during both inspiration and expiration?
Pleural friction rub
69. What causes a pleural friction rub?
Inflamed visceral and parietal pleura rubbing together
70. Where is a pleural friction rub best heard?
Over the area where the patient reports pleuritic chest pain
71. How is rhonchi best described?
Continuous low-pitched sounds with a snoring or gurgling quality, heard during inspiration and expiration
72. What typically causes rhonchi?
Air passing through an obstructed airway due to secretions, bronchial spasm, or tumors
73. What type of lung sound is a continuous, high-pitched wheeze indicating upper airway obstruction?
Stridor
74. What breath sound is described as a continuous musical or whistling sound with various pitches?
Wheeze
75. What causes wheezes during auscultation?
Turbulent airflow through narrowed airways due to bronchospasm, edema, collapse, secretions, or foreign bodies
76. When heard in peripheral lung fields, what do bronchial breath sounds suggest?
Abnormal findings such as lung consolidation
77. What condition commonly produces bronchial breath sounds in the periphery?
Pneumonia
78. What might decreased or diminished breath sounds indicate?
Severe airway congestion, emphysema, or hypoventilation
79. What do absent breath sounds suggest?
Pneumothorax or complete lung collapse
80. How are spoken voice sounds normally transmitted through healthy lung tissue?
Muffled and indistinct, especially with whispered words
81. What does increased loudness and clarity of voice sounds typically indicate?
Lung consolidation, atelectasis, or fibrosis
82. Why are whispered and spoken voice sounds useful in lung assessment?
They help detect consolidation, infarction, or atelectasis more sensitively than breath sounds alone
83. What is bronchophony?
Abnormally increased vocal resonance with clearer and louder spoken words (e.g., “99”)
84. What is egophony?
A form of bronchophony where the spoken long “E” changes to a long, nasal-sounding “A”
85. What is whispered pectoriloquy?
The ability to clearly hear whispered words like “1, 2, 3” over areas of lung consolidation
86. What are the three categories of auscultated lung sounds?
Sounds of breathing, added (adventitious) sounds, and other unknown sounds
87. What creates the basic sound of breathing?
Gas moving in and out of the lungs
88. What are the two primary types of breath sounds?
Normal (vesicular) and bronchial (bronchovesicular)
89. How are normal vesicular breath sounds described?
Soft, low-pitched, rustling sounds heard over the lung parenchyma
90. During which phase of breathing are normal breath sounds the loudest?
Inspiration
91. How long do normal breath sounds typically last during expiration?
They fade after the first one-third to one-half of expiration
92. What factors can alter normal breath sound characteristics?
Breathing rate, depth, and patient body size
93. What findings can help identify an abnormal breath sound during auscultation?
Reduced or absent breath sounds, or the presence of increased bronchial breath sounds
94. What are common causes of reduced or absent breath sounds?
Decreased sound transmission due to reduced ventilation or an abnormal barrier between the lungs and the stethoscope
95. What respiratory conditions can result in diminished or absent breath sounds?
Shallow breathing, atelectasis, hypoventilation, absence of lung tissue, internal masses, or hyperinflation
96. What pathological conditions can lead to completely absent breath sounds?
Total obstruction of a major bronchus, large pneumothorax, or complete lung collapse
97. What surgical or disease-related events may cause absent breath sounds?
Pneumonectomy or the presence of a large pleural effusion
98. How would you best describe added lung sounds?
Discontinuous, non-musical crackling sounds heard during inspiration, expiration, or both
99. What physiological changes lead to the generation of added breath sounds?
Sudden opening or closing of alveoli or airways due to altered lung elasticity
100. What causes the crackling sound associated with added lung sounds?
Rapid equalization of pressure between collapsed alveoli and adjacent airways
Final Thoughts
Auscultation is far more than a traditional ritual—it is a powerful, practical, and indispensable tool in respiratory care. By listening to the lungs, respiratory therapists can detect early signs of disease, monitor treatment effectiveness, and make critical decisions in real time.
While technology continues to advance, auscultation endures as a foundational skill that bridges the art and science of respiratory therapy. For both students learning the craft and seasoned clinicians practicing at the bedside, auscultation remains a cornerstone of patient assessment and a testament to the value of attentive listening in healthcare.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Sarkar M, Madabhavi I, Niranjan N, Dogra M. Auscultation of the respiratory system. Ann Thorac Med. 2015.

