In the field of respiratory care, maintaining a patient’s airway is one of the most critical responsibilities. When natural breathing is compromised due to illness, trauma, or surgical procedures, healthcare providers may rely on an artificial airway to ensure adequate oxygen delivery and carbon dioxide removal.
For respiratory therapists, understanding artificial airways is fundamental, as these devices play a direct role in life support, ventilation management, and patient safety.
What is an Artificial Airway?
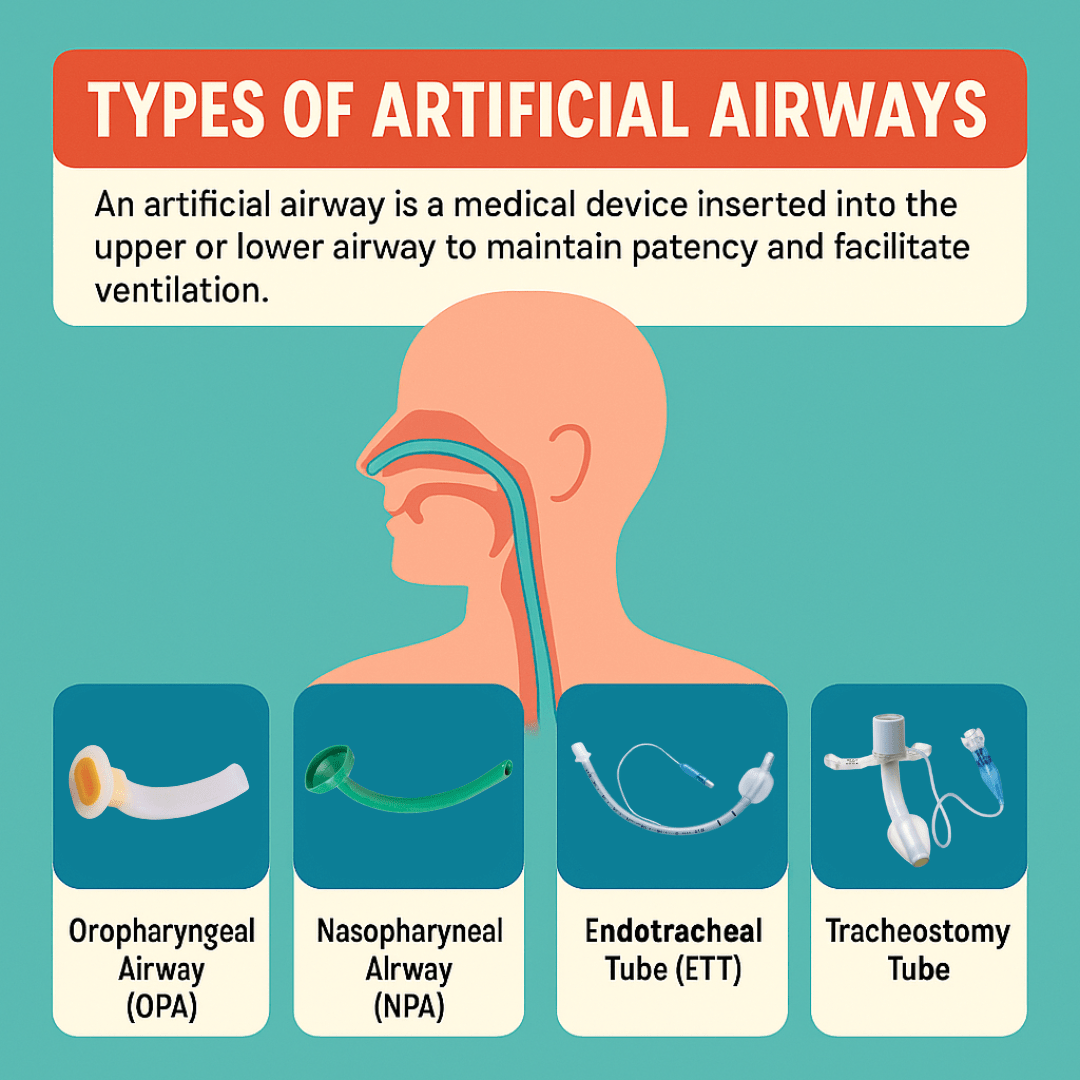
An artificial airway is a medical device inserted into the patient’s upper or lower airway to maintain patency, facilitate ventilation, and protect the lungs. It bypasses or supports the natural airway when it is obstructed or inadequate.
Artificial airways are temporary or long-term depending on the patient’s condition, and their placement requires close monitoring by respiratory therapists to prevent complications.
Types of Artificial Airways
Artificial airways come in several forms, each designed for specific clinical situations. The choice of device depends on factors such as the patient’s level of consciousness, the presence of protective reflexes, the anticipated duration of airway support, and whether mechanical ventilation is required.
Here are the most common types of artificial airways used in respiratory care:
1. Oropharyngeal Airway (OPA)
An oropharyngeal airway is a curved plastic device that is inserted through the mouth and rests in the pharynx, positioned just above the glottis. Its primary purpose is to prevent the tongue from falling back against the posterior pharyngeal wall, which can obstruct airflow—particularly in unconscious patients.
Because it stimulates the gag reflex, it is not recommended for conscious or semi-conscious individuals, as insertion may provoke vomiting, aspiration, or laryngospasm.
The OPA is most useful during resuscitation efforts, in operating rooms under general anesthesia, and in emergency situations where airway obstruction from soft tissue collapse is a concern. Respiratory therapists must ensure the correct size is chosen, as a device that is too short may fail to keep the tongue away from the airway, while one that is too long could push the epiglottis downward and worsen the obstruction.
2. Nasopharyngeal Airway (NPA)
A nasopharyngeal airway is a soft, flexible tube inserted through the nostril, passing into the pharynx to create a clear pathway for airflow. Unlike the OPA, it is more comfortable for patients who are semi-conscious or awake because it does not strongly stimulate the gag reflex. For this reason, it is sometimes called the “nasal trumpet.”
NPAs are especially valuable for patients requiring frequent suctioning, such as those with thick secretions or impaired ability to clear their airway.
They are also useful in patients with facial trauma or trismus (lockjaw) that makes oral access difficult. However, they should be used with caution in cases of suspected basilar skull fracture or severe nasal injury, as insertion could lead to intracranial placement or bleeding.
3. Endotracheal Tube (ETT)
An endotracheal tube is one of the most common and critical artificial airways in acute care. It is a flexible plastic tube inserted through the mouth (orotracheal) or nose (nasotracheal) and advanced into the trachea. Its placement ensures a secure airway that allows direct ventilation, suctioning, and delivery of oxygen or anesthetic gases.
Most modern ETTs include an inflatable cuff near the distal end, which seals against the tracheal wall to prevent aspiration and ensure adequate ventilation pressures.
Endotracheal intubation is typically performed in emergencies, critical illness, or during surgical procedures that require controlled ventilation. Although lifesaving, it carries risks such as trauma to the airway, infection, or accidental extubation. Prolonged use can also cause damage to the trachea, which is why tracheostomy may eventually be considered for long-term ventilation.
4. Tracheostomy Tube
A tracheostomy tube is placed surgically through an incision in the neck directly into the trachea. Unlike OPAs and NPAs, which are temporary and less invasive, or the ETT, which is suitable for short- to medium-term use, a tracheostomy provides a stable, long-term solution for patients who require extended airway support.
Tracheostomies reduce airway resistance and dead space, often making breathing more comfortable and efficient for patients. They also facilitate suctioning, oral hygiene, and, in some cases, allow patients to eat and speak with specialized valve attachments.
Compared to prolonged intubation, tracheostomy tubes carry a lower risk of laryngeal injury, but they still require diligent care to prevent infection, obstruction, or accidental decannulation.
Why Artificial Airways are Relevant in Respiratory Care
- Ventilator Management: Artificial airways allow connection to mechanical ventilators, enabling precise control of oxygen delivery, tidal volume, and airway pressures. Respiratory therapists adjust ventilator settings based on patient needs.
- Airway Protection: In patients with impaired consciousness or weak airway reflexes, artificial airways prevent aspiration of secretions or gastric contents into the lungs.
- Airway Clearance: Respiratory therapists use artificial airways to perform suctioning, helping remove secretions that patients cannot clear independently.
- Critical Care and Emergency Response: From cardiac arrest to severe respiratory failure, artificial airways are lifesaving interventions that respiratory therapists are trained to place, manage, and monitor.
The Role of Respiratory Therapists
Respiratory therapists play a central role in:
- Selecting the appropriate airway device.
- Assisting with insertion and securing of the device.
- Monitoring for complications such as infection, obstruction, or accidental removal.
- Educating patients and families when long-term airways like tracheostomies are required.
Note: Their expertise ensures that artificial airways are not only placed correctly but also managed safely throughout the course of care.
Artificial Airway Practice Questions
1. Inserting a tube into the trachea to bypass the upper airway and laryngeal structures creates what type of airway?
An artificial airway
2. What surgical procedure is performed when long-term airway support is expected?
Tracheotomy
3. What is the preferred method of emergency intubation, and why?
Oral intubation; it allows rapid airway control and the use of a larger-diameter tube to reduce airway resistance
4. What type of intubation involves blindly inserting a tube through the nose and into the trachea?
Nasal endotracheal intubation
5. What must be obtained before non-emergent endotracheal intubation?
Informed consent
6. What is rapid-sequence intubation (RSI), and when is it contraindicated?
Simultaneous administration of sedative and paralytic for emergency airway management; contraindicated in cardiac arrest or known difficult airways
7. What sedative-hypnotic drug is commonly used for inducing unconsciousness during intubation?
Midazolam (Versed) or Etomidate (Amidate)
8. What opioid is used for pain control during intubation?
Fentanyl
9. What neuromuscular blocker is used for rapid muscle paralysis during intubation?
Succinylcholine (Anectine)
10. What is the ideal head position for oral intubation?
Supine with the head extended and neck flexed (sniffing position)
11. What medications may be used to reduce trauma during nasal intubation?
Lidocaine (Xylocaine) and Epinephrine
12. How do you confirm proper placement of an artificial airway after insertion?
Colorimetric CO₂ detector, bilateral chest auscultation, and visible chest rise with ventilation
13. What should be documented after endotracheal tube placement?
Tube size, insertion depth, cuff pressure, position, lip or mucosal injuries, and any bleeding
14. Before extubating a patient, what steps must be completed?
Suction oropharynx and ETT, preoxygenate the patient, and confirm cuff deflation
15. What is the most common reason for performing tracheal suctioning?
Retention of secretions
16. What is the most frequent complication associated with suctioning?
Hypoxemia
17. A cuff pressure of 45 cm H₂O during sealing with a minimal occluding volume suggests what issue?
The endotracheal tube is too small for the patient
18. What are some complications of tracheal suctioning?
Bronchospasm, mucosal trauma, elevated intracranial pressure
19. How often should a patient be suctioned?
Only when clinical signs indicate the need
20. What is the appropriate suction pressure range for adults?
-100 to -120 mm Hg
21. What is the maximum suction catheter size for a 6-mm endotracheal tube?
10 French
22. What is the maximum suction catheter size for an 8-mm endotracheal tube?
14 French
23. A mechanically ventilated patient with a tracheostomy shows rising peak inspiratory pressures and decreased breath sounds. What is the likely cause?
Partial obstruction of the tracheostomy tube
24. To prevent hypoxemia during suctioning, what should be done first?
Preoxygenate the patient with 100% oxygen
25. How can you maintain PEEP and FiO₂ during suctioning in a mechanically ventilated patient?
Use a closed-system suction catheter
26. What is the maximum total application time recommended for endotracheal suctioning in adults?
10 to 15 seconds
27. Which features of modern endotracheal tubes assist in confirming correct tube placement?
Length markings on the tube and a radiopaque indicator near the tip
28. Which medications can be used to reduce bleeding risk during fiberoptic bronchoscopy?
Phenylephrine and Epinephrine
29. While suctioning, you observe an abrupt ECG change. What is the most appropriate response?
Stop suctioning immediately and administer oxygen
30. Which techniques help reduce the risk of mucosal trauma during suctioning?
Rotating the catheter while withdrawing and limiting suction pressure
31. What is the recommended suction pressure range for children during airway suctioning?
-100 to -120 mm Hg
32. What is an absolute contraindication for performing nasotracheal suctioning?
Epiglottitis and croup
33. After multiple nasotracheal suctions, a patient develops minor nasal bleeding. What action should you take?
Control the bleeding and use a nasopharyngeal airway for future suctioning
34. Coarse breath sounds clear after suctioning, but expiratory wheezing is now heard. What is the likely cause?
The patient developed bronchospasm due to hyperactive airways
35. What general clinical conditions typically require airway management?
Airway compromise, respiratory failure, or the need to protect the airway
36. Which signs indicate a patient is unable to adequately protect their airway?
Coma, absence of gag reflex, and inability to cough
37. Which types of artificial airways are inserted through the larynx?
Orotracheal and nasotracheal tubes
38. What are the advantages of oral intubation compared to nasal intubation?
Less risk of kinking, easier suctioning, and less traumatic insertion
39. What are the advantages of nasal intubation compared to oral intubation?
Less gag reflex stimulation, reduced risk of accidental extubation, and greater comfort for long-term use
40. Compared to endotracheal intubation, what are the benefits of a tracheostomy?
Improved patient comfort, reduced risk of mainstem intubation, and avoidance of upper airway complications
41. What is the universal external adapter size for endotracheal and tracheostomy tubes?
15 mm
42. What is the function of the Murphy eye on modern endotracheal tubes?
To maintain airflow if the main opening becomes obstructed
43. What is the purpose of the cuff on an artificial airway?
To seal the airway and prevent aspiration
44. What does the pilot balloon on an endotracheal or tracheostomy tube indicate?
It allows monitoring of the cuff’s inflation status and pressure
45. What is the function of the removable inner cannula in a tracheostomy tube?
To aid in cleaning and to maintain airway patency if obstruction occurs
46. What is the purpose of a tracheostomy obturator?
To guide the outer cannula during insertion and reduce mucosal trauma
47. If no facial or neck trauma is present, what is the preferred emergency airway technique?
Orotracheal intubation
48. What equipment must be checked before initiating an intubation procedure?
Laryngoscope light source, endotracheal tube cuff, and suction setup
49. During emergency intubation, the Miller blade works, but the Macintosh blade doesn’t light. What should you do?
Check and replace the bulb on the Macintosh blade
50. What is the function of a stylet used with an endotracheal tube?
To provide shape and rigidity for easier insertion
51. How should a patient’s head and neck be positioned to facilitate oral intubation?
With the neck flexed and the head extended (sniffing position), supported by a towel under the neck
52. What is the maximum recommended time for a single intubation attempt?
30 seconds
53. During oral intubation, how far should the endotracheal tube be advanced into the trachea?
Until the cuff passes through the vocal cords
54. What are the immediate steps after placing an oral endotracheal tube in an adult?
Stabilize the tube, inflate the cuff, and begin ventilation or oxygenation
55. Where should the distal tip of a properly positioned endotracheal tube lie in an adult male?
Approximately 3 to 6 cm above the carina.
56. Which bedside method can definitively confirm that an endotracheal tube is correctly placed in the trachea?
Fiberoptic laryngoscopy
57. What is the typical distance from the tip of a properly positioned oral endotracheal tube to the incisors in an adult male?
21 to 23 cm
58. When using a bulb-type esophageal detection device, how can you tell the tube is in the esophagus?
The bulb fails to reexpand after being released
59. After an intubation attempt, capnography shows near-zero CO₂. What does this likely indicate?
The tube is in the esophagus
60. What condition can cause a false-negative result when using capnometry to verify tube placement?
Cardiac arrest (due to minimal or no pulmonary perfusion)
61. After intubating a cardiac arrest patient, you notice a gradual rise in exhaled CO₂ levels. What does this suggest?
Return of spontaneous circulation (ROSC)
62. A trauma patient with a maxillofacial injury needs short-term ventilation. What airway approach is best?
Nasal intubation
63. What is the primary indication for performing a tracheostomy?
Need for long-term airway management
64. What factors should be considered when deciding to switch from an endotracheal tube to a tracheostomy tube?
Patient’s condition, tolerance, duration of need, risk comparison, and ability to undergo surgery
65. In a standard surgical tracheotomy, where is the incision made to access the trachea?
Through or between the second and third tracheal rings
66. During an elective tracheotomy on an orally intubated patient, what is your role as an RT?
Withdraw the oral tube 2 to 3 inches while the incision is made
67. Compared with traditional surgical tracheostomy, what are benefits of percutaneous dilatational tracheostomy?
Fewer complications, quicker procedure, and can be done at the bedside
68. What is the most common symptom of transient glottic edema or vocal cord inflammation after extubation?
Hoarseness
69. An adult patient develops a high-pitched inspiratory noise after extubation. What should you do?
Administer a STAT racemic epinephrine aerosol treatment
70. After prolonged tracheostomy, where can tracheal stenosis commonly develop?
At the cuff site, stoma site, or tube tip
71. A patient on a T-piece setup is at risk for tracheal damage due to tube movement. What can reduce this risk?
Switch to a tracheostomy collar to allow more stable support
72. What methods help reduce infection risk at a tracheostomy site?
Sterile dressing changes, aseptic technique, and routine stoma cleaning
73. What autonomic or protective reflexes can be triggered during emergency airway management?
Bradycardia, hypotension, cardiac arrhythmias, and laryngospasm
74. On chest X-ray, where should the distal tip of an endotracheal or tracheostomy tube be positioned?
3 to 6 cm above the carina
75. If a chest radiograph shows the endotracheal tube tip is only 2 cm above the carina, what should you do?
Withdraw the tube by 2 to 3 cm using tube markings as a guide
76. Which of the following are valid indications for emergency tracheal intubation?
Upper airway or laryngeal edema, loss of protective reflexes, hypoxic respiratory failure, and traumatic upper airway obstruction
77. To ensure adequate humidification for a patient with an artificial airway, inspired gas should be 100% saturated with water vapor at what temperature?
32° to 35° C
78. Why do tracheal airways increase the risk of pulmonary infections?
Due to increased risk of aspiration, contaminated equipment, and impaired cough clearance
79. What is the recommended range for tracheal tube cuff pressures?
20 to 25 mm Hg
80. What effect can repeated connection and disconnection of the cuff pressure manometer have?
It may lead to a gradual decrease in cuff pressure
81. Which of the following statements about cuff inflation techniques is FALSE?
The minimal leak technique eliminates the need for cuff pressure monitoring
82. What is the appropriate suction pressure range for infants during endotracheal suctioning?
-80 to -100 mm Hg
83. What measures can help minimize the risk of aspiration in intubated patients receiving enteral nutrition?
Use semi-recumbent positioning, post-pyloric feeding tube placement, subglottic suctioning, and slightly higher cuff pressure during and after feedings
84. What are common causes of tracheal tube obstruction in a patient with a tracheal airway?
Cuff herniation, mucus plugs, kinking of the tube, or impingement on the tracheal wall
85. A patient with a tracheal tube exhibits severe distress and no breath sounds. What is the likely cause?
Complete obstruction of the tracheal tube
86. If head repositioning and cuff deflation do not relieve a complete endotracheal tube obstruction, what is the next step?
Immediately extubate the patient and provide ventilation
87. What is the best course of action if a mechanically ventilated patient accidentally dislodges the endotracheal tube?
Remove the tube and begin manual ventilation or oxygenation
88. What does a positive cuff leak test suggest prior to extubation?
Low risk of upper airway obstruction
89. Which findings indicate a patient is ready for extubation based on secretion clearance ability?
Strong cough on suctioning, cooperative behavior, and a maximum inspiratory pressure of at least -73 cm H2O
90. What supplies should be gathered before assisting with extubation?
Suction setup, oxygen or aerosol equipment, manual resuscitator and mask, racemic epinephrine, and intubation tray
91. What aerosol therapy is most appropriate to reduce laryngeal swelling after extubation?
Cool mist delivered by a jet nebulizer and aerosol mask
92. What equipment is required for performing nasotracheal suctioning?
Suction catheter kit, oxygen delivery system, sterile saline or water
93. After extubation, which clinical parameters should be monitored closely?
Color, breath sounds, and vital signs
94. An adult patient develops stridor while receiving cool mist after extubation. What is the appropriate intervention?
Administer a racemic epinephrine treatment
95. What is a rare but potentially life-threatening complication following extubation?
Laryngospasm
96. What methods can be used to begin weaning a patient from a tracheostomy tube?
Use progressively smaller tubes, switch to a fenestrated tube, or apply a tracheostomy button
97. How do you assess upper airway function in a patient with a fenestrated tracheostomy tube?
Remove the inner cannula, deflate the cuff, and occlude the proximal opening
98. For which of the following purposes is a tracheal button used?
To maintain airway patency and assist with secretion clearance
99. How do you estimate the correct size of an oropharyngeal airway (OPA)?
Hold it from the corner of the mouth to the angle of the jaw
100. Which of the following are contraindications for oropharyngeal airway placement?
Intact gag reflex, vomiting, oral trauma, active seizures, awake and alert state
Final Thoughts
Artificial airways are vital tools in modern respiratory care, ensuring patients receive the oxygen they need when natural airway function is compromised. For respiratory therapists, mastering the knowledge and skills of airway management is a cornerstone of their practice.
Whether in emergency care, intensive care units, or long-term support, artificial airways remain at the heart of life-saving respiratory therapy.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Branson RD, Gomaa D, Rodriquez D Jr. Management of the artificial airway. Respir Care. 2014.