A cough that lingers for weeks or even months can be frustrating, exhausting, and sometimes alarming. While many coughs fade on their own after a short illness, a persistent cough often signals an underlying issue that needs attention.
From common conditions like asthma, allergies, and acid reflux to more serious concerns such as chronic bronchitis or lung disease, a long-lasting cough should never be ignored.
Understanding the possible causes can help you recognize when it’s time to seek medical advice and take steps toward relief.
Download our free guide that has over 100+ of the best tips for healthy lungs.
What Can Cause a Cough to Last for Months?
A cough that lingers for months is often considered chronic and can stem from several causes. Common culprits include asthma, which irritates and narrows the airways, and gastroesophageal reflux disease (GERD), where stomach acid irritates the throat and lungs. Postnasal drip from allergies or sinus problems can also cause persistent coughing.
Chronic bronchitis, part of chronic obstructive pulmonary disease (COPD), leads to ongoing inflammation of the airways. Smoking or long-term exposure to irritants like dust, chemicals, or pollution may worsen symptoms.
Less common but serious causes include lung infections, heart failure, or even lung cancer. Because a prolonged cough may signal an underlying condition, medical evaluation is recommended to identify the cause and ensure proper treatment.
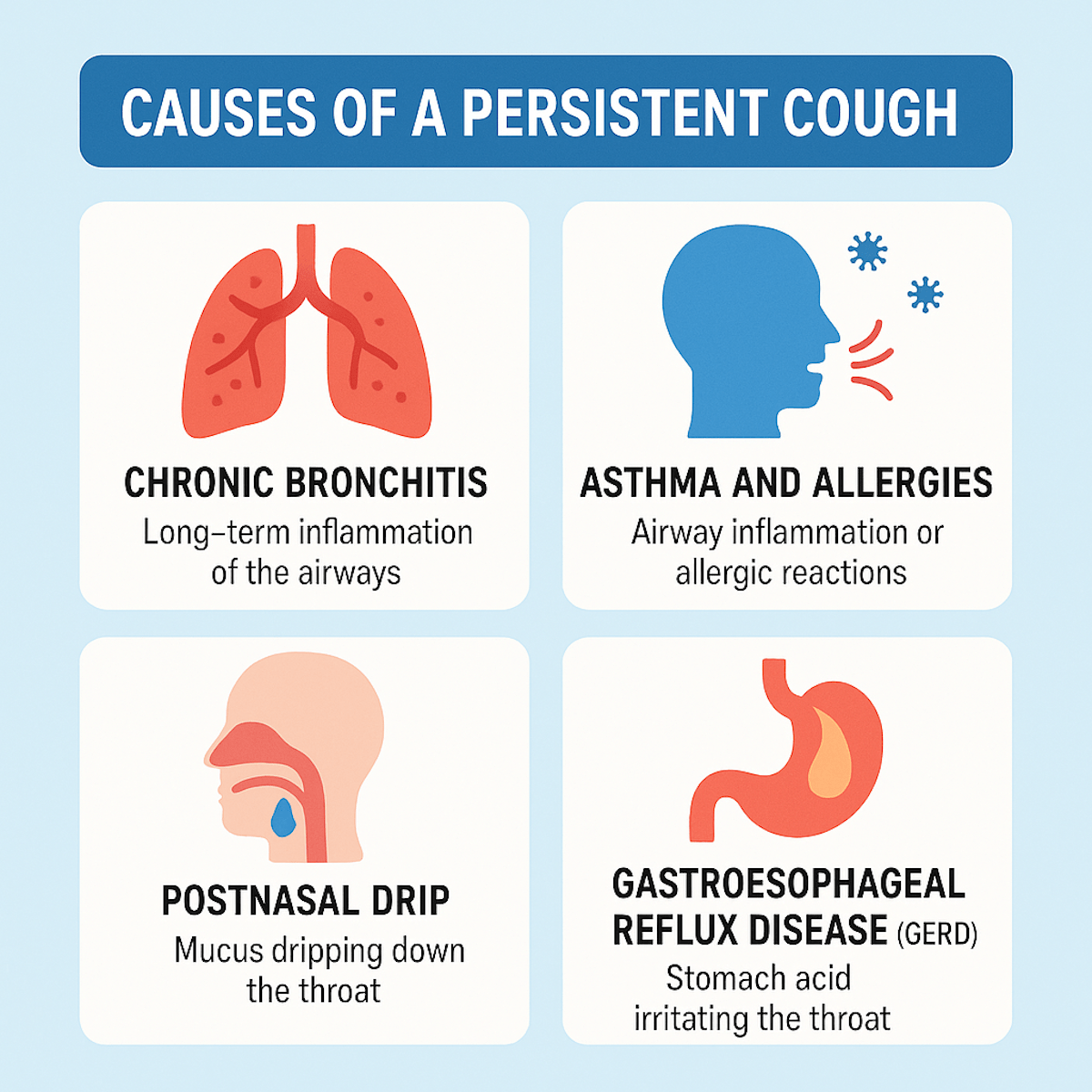
Causes of a Persistent Cough
A cough lasting several months often arises from underlying respiratory or digestive issues. Common causes include chronic inflammation, allergic reactions, and acid irritation, each producing distinct patterns and symptoms. Understanding these can guide proper diagnosis and treatment.
Chronic Bronchitis
Chronic bronchitis is a long-term inflammation of the bronchial tubes, often caused by smoking or prolonged exposure to irritants like pollution. It leads to increased mucus production and a productive cough lasting at least three months over two consecutive years. The cough is usually worse in the morning and can be accompanied by wheezing and shortness of breath.
Infections or repeated irritations damage the airway lining, triggering persistent cough as the body tries to clear mucus. Treatment focuses on quitting smoking, avoiding irritants, and managing symptoms with bronchodilators and steroids.
Asthma and Allergies
Asthma causes airway inflammation and tightening, resulting in coughing, wheezing, and difficulty breathing. The cough often worsens at night or with exercise. Allergic reactions to pollen, dust mites, or pet dander trigger similar symptoms by causing airway swelling and excess mucus.
These conditions activate the immune system, making the airways overly sensitive. Inhaled corticosteroids and antihistamines help reduce inflammation and control symptoms. Accurate diagnosis may require lung function tests and allergy screening.
Postnasal Drip
Postnasal drip occurs when excess mucus from the nasal passages drips down the throat. It irritates the throat and triggers a reflex cough to clear the mucus. This condition may result from chronic sinus infections, allergies, or irritants like smoke.
Symptoms include a sensation of mucus in the throat, frequent throat clearing, and a cough that worsens when lying down. Treatment targets the underlying nasal inflammation with decongestants, nasal sprays, or allergy medications.
Gastroesophageal Reflux Disease (GERD)
GERD causes stomach acid to flow back into the esophagus and sometimes reach the throat, irritating the lining. This acid irritation can trigger a persistent cough, especially after eating or when lying flat. Some people may not experience typical heartburn but still have acid-related cough.
The cough often appears dry and may be accompanied by hoarseness or throat clearing. Treatment involves lifestyle changes, such as avoiding late meals and acidic foods, and medications like proton pump inhibitors to reduce acid production.
When to Seek Medical Attention
A cough lasting for months may indicate an underlying health issue requiring professional evaluation. Identifying specific warning signs, understanding individual risk factors, and knowing the criteria doctors use to diagnose chronic cough can help determine when medical care is necessary.
Warning Signs and Symptoms
Persistent coughing accompanied by blood in the sputum or chest pain requires immediate medical attention. Other red flags include significant weight loss, night sweats, or fever lasting more than a few days.
Difficulty breathing or wheezing should also prompt urgent evaluation, as these may signal serious lung or heart conditions. A cough lasting more than eight weeks without improvement warrants a thorough medical assessment.
Risk Factors for Serious Conditions
People who smoke or have a history of asthma, chronic obstructive pulmonary disease (COPD), or lung infections are at higher risk. Exposure to environmental pollutants, occupational irritants, or a weakened immune system increases the chance of serious causes.
Older adults and those with a history of cancer or recent travel to areas with high tuberculosis rates should be particularly vigilant. Early identification of these factors helps prioritize timely diagnosis and treatment.
Diagnostic Criteria for Chronic Cough
A chronic cough is defined as one lasting longer than eight weeks in adults or four weeks in children. Doctors assess patient history, symptom patterns, and any associated signs such as wheezing or sputum production.
Common causes considered include postnasal drip, asthma, gastroesophageal reflux disease (GERD), and chronic bronchitis. Diagnostic tests may include chest X-rays, spirometry, or sputum analysis to pinpoint the cause and guide treatment.
Common Misdiagnoses and Overlooked Conditions
Persistent coughs are often mistaken for common colds or allergies, but they can signal more serious or less obvious issues. Some causes might be related to medications, malignancies, or chronic lung diseases that require specific attention.
Medication Side Effects
Certain medications, especially ACE inhibitors used for high blood pressure, frequently cause a dry cough that can last for months. This side effect may be overlooked if doctors do not review the patient’s medication history carefully.
The cough caused by these drugs usually appears within weeks of starting treatment and stops when the medication is discontinued. Patients may not connect their cough to a medicine prescribed for unrelated issues, delaying diagnosis.
Other medications, like beta blockers or some chemotherapy drugs, can also trigger prolonged coughing. Identifying this cause requires detailed patient interviews and sometimes trial discontinuation under medical supervision.
Lung Cancer
A cough that persists for months can be an early symptom of lung cancer, especially in smokers or those with a history of exposure to carcinogens. The cough is often harsh, sometimes accompanied by blood or changes in sputum color.
Lung cancer-related coughs do not respond to typical cold or asthma treatments. Early diagnosis relies on imaging tests like X-rays or CT scans, paired with a biopsy for confirmation.
Note: Other symptoms, such as weight loss, chest pain, or shortness of breath, may also be present but are not always obvious at first.
Chronic Obstructive Pulmonary Disease (COPD)
COPD, including emphysema and chronic bronchitis, causes a long-lasting cough due to airway inflammation and mucus buildup. It primarily affects smokers or people exposed to long-term lung irritants.
The cough in COPD is usually productive, with thick mucus that persists for over three months in a year for at least two consecutive years. Patients often experience wheezing and gradual breathlessness.
Note: Diagnosis involves lung function tests (spirometry) to assess airway obstruction. Recognizing COPD early can improve management and slow disease progression.
Diagnostic Tests for a Cough That Won’t Go Away
A persistent cough requires thorough evaluation through specific tests. These tests help identify the underlying cause by examining the lungs, airway function, and potential allergens.
Imaging and X-rays
Chest X-rays are often the first imaging test used to assess a chronic cough. They can reveal infections, lung tumors, chronic lung diseases, or fluid buildup. If X-rays do not provide clear answers, a CT scan may be ordered. This offers detailed images of the lungs and airways, helping detect smaller abnormalities or structural problems.
Note: Imaging tests are non-invasive and crucial for ruling out serious conditions such as pneumonia, bronchiectasis, or lung cancer.
Spirometry and Lung Function Tests
Spirometry measures how much air a person can breathe in and out, and how quickly. It helps diagnose obstructive lung diseases like asthma and chronic obstructive pulmonary disease (COPD). During spirometry, patients take a deep breath and exhale forcefully. Lung function tests can also assess airflow limitation or identify restrictive lung disorders.
Note: These tests provide objective data about lung capacity and airway resistance, guiding doctors toward specific diagnoses related to persistent cough.
Allergy Testing
Allergy testing determines if allergic reactions contribute to the cough. Skin prick tests or blood tests identify sensitivities to common allergens like pollen, dust mites, or pet dander.
If allergy testing reveals a trigger, targeted treatments such as antihistamines or avoiding allergens may reduce coughing episodes. This testing is important when allergic rhinitis or asthma is suspected to fuel chronic cough symptoms.
Treatment Options for Long-Term Cough
Managing a cough that persists for months involves multiple approaches targeting different factors. These include modifying daily habits, using specific medications, and treating any root cause identified through medical evaluation.
Lifestyle Adjustments
Lifestyle changes can reduce cough triggers and help lessen symptoms. Avoiding exposure to smoke, dust, and chemical irritants is essential. Using a humidifier can ease throat dryness often linked to chronic coughing.
Staying hydrated thins mucus, aiding its clearance from the airways. Patients should limit caffeine and alcohol, as these can dehydrate the body. Elevating the head during sleep may reduce postnasal drip, a common cause of prolonged cough.
Note: Stopping smoking is crucial. Quitting halts ongoing lung irritation and promotes healing. Regular hand washing also helps prevent respiratory infections that might worsen or prolong cough.
Prescription Medications
Doctors may prescribe medications based on the cough’s cause and severity. Common options include inhaled corticosteroids for inflammation and bronchodilators to open airways in cases of asthma or chronic obstructive pulmonary disease (COPD).
If acid reflux causes the cough, proton pump inhibitors or H2 blockers can reduce stomach acid. For coughs linked to allergies, antihistamines and nasal corticosteroids may be recommended.
In cases of persistent cough from infections, antibiotics or antifungals might be necessary. Cough suppressants are generally avoided with productive coughs but may be considered if the cough disrupts sleep.
Addressing Underlying Conditions
Identifying and treating the primary cause is key to resolving a long-term cough. Common underlying issues include asthma, gastroesophageal reflux disease (GERD), chronic bronchitis, and postnasal drip. Patients require thorough evaluation, possibly including chest X-rays, spirometry, or sinus imaging. Treating asthma involves avoiding triggers and regular use of inhalers.
For GERD, lifestyle changes and medications reduce acid reflux. Allergic rhinitis often requires antihistamines and nasal sprays. Chronic bronchitis treatment focuses on smoking cessation and pulmonary rehabilitation.
Note: Failure to address these conditions allows the cough to persist or worsen, making targeted treatment essential.
Prevention and Reducing Recurrence
Addressing persistent cough involves controlling triggers and boosting the body’s defenses. Small but targeted lifestyle adjustments can significantly reduce repeated episodes and lessen their duration.
Environmental Modifications
Reducing exposure to irritants like dust, smoke, and chemicals is essential. Using air purifiers in living spaces can lower airborne allergens and pollutants. Regular cleaning to remove dust and mold helps minimize respiratory irritation.
Humidity levels should be maintained between 30-50% to prevent dry air, which can worsen coughs. Avoiding strong fragrances and harsh cleaning products also reduces throat irritation. Proper ventilation in work and home environments further limits contact with airborne irritants.
Smoking Cessation
Quitting smoking is the most effective way to prevent chronic cough related to tobacco use. Smoke damages airway linings, causing persistent irritation and cough. Avoiding secondhand smoke also helps prevent respiratory inflammation.
Support programs, nicotine replacement therapies, and counseling improve success rates in quitting. After cessation, coughs caused by smoking typically lessen over weeks to months as lung function gradually improves.
FAQs About a Cough That Won’t Go Away for Months
Can a Cough Last for Months?
Yes, a cough can last for months and is often classified as chronic if it persists for more than eight weeks in adults. Common causes include asthma, chronic bronchitis, postnasal drip, or gastroesophageal reflux disease (GERD). Long-term exposure to smoke, dust, or other irritants may also contribute.
While some chronic coughs are manageable with lifestyle changes or medication, others may indicate more serious conditions that need medical evaluation. Persistent coughing should not be ignored and always warrants attention.
Why Do I Have a Cough With Phlegm That Won’t Go Away?
A cough with phlegm that won’t resolve is usually a sign of excess mucus production caused by infection, allergies, or chronic lung conditions like COPD or bronchiectasis. Respiratory infections, even after the acute illness clears, can leave lingering airway irritation that produces phlegm.
Smoking and environmental irritants may worsen symptoms. Less commonly, long-term phlegm production may signal more serious conditions like pneumonia or lung cancer. If your cough persists for weeks, consult a healthcare provider for proper diagnosis and treatment.
What Are the Red Flags for a Chronic Cough?
Red flags for a chronic cough include coughing up blood, unexplained weight loss, persistent chest pain, shortness of breath, or night sweats. These symptoms may point to serious underlying conditions such as lung cancer, tuberculosis, or advanced COPD.
Other concerning signs include worsening wheezing, severe fatigue, or swelling in the legs and ankles, which may indicate heart-related issues. If a cough interferes with sleep, daily function, or is accompanied by these warning signs, immediate medical attention is strongly recommended.
When to Be Concerned About a Cough That Won’t Go Away?
You should be concerned about a cough that lasts longer than eight weeks in adults or four weeks in children. A persistent cough may indicate chronic respiratory disease, asthma, GERD, or infections like pneumonia.
Coughs that worsen at night, produce blood, or are paired with chest pain, difficulty breathing, or unintended weight loss are especially concerning. Even if symptoms seem mild, a lingering cough could be your body’s signal of a deeper problem, making medical evaluation essential for peace of mind and proper care.
Final Thoughts
A cough that refuses to go away for months is more than just an inconvenience—it can be a sign of an underlying condition that requires attention. While some causes may be relatively minor and treatable at home, others may indicate chronic respiratory issues or more serious health concerns.
Paying attention to accompanying symptoms and seeking medical evaluation when needed are key to finding answers and relief. By identifying the root cause, you can move beyond frustration and take the right steps toward restoring your health and comfort.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Alhajjaj MS, Sankari A, Bajaj P. Chronic Cough. [Updated 2024 Oct 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.


