Cricothyrotomy is an emergency airway procedure performed when traditional methods such as endotracheal intubation are not possible or have failed. By making an incision through the cricothyroid membrane, it creates a direct pathway for air to reach the lungs, offering rapid and often lifesaving access to ventilation.
Though considered a last-resort intervention, its role in critical care is undeniable. For respiratory therapists, understanding the cricothyrotomy procedure is essential for supporting physicians, managing the airway afterward, and ensuring patient safety during high-risk emergencies.
What is a Cricothyrotomy?
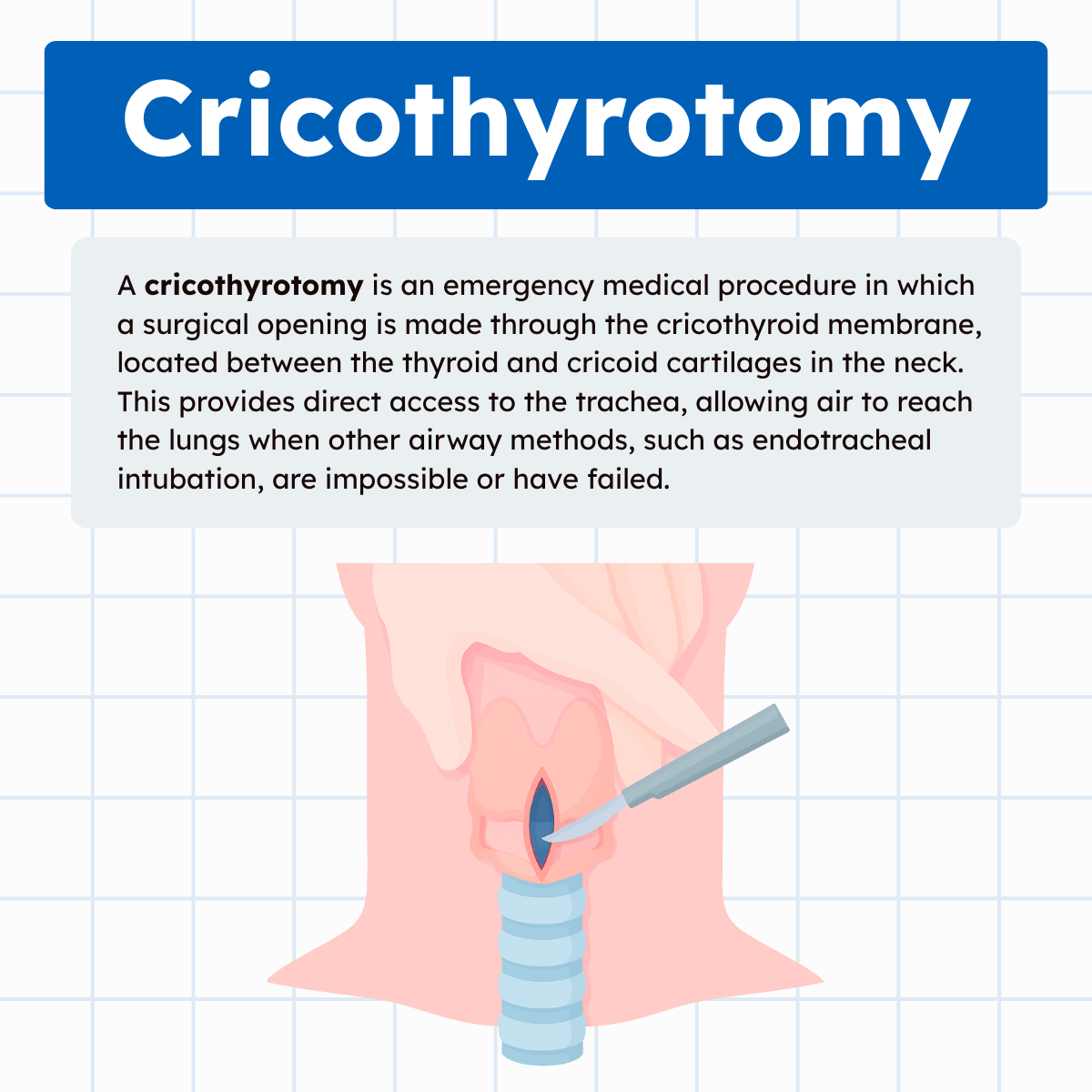
A cricothyrotomy is an emergency medical procedure in which a surgical opening is made through the cricothyroid membrane, located between the thyroid and cricoid cartilages in the neck. This provides direct access to the trachea, allowing air to reach the lungs when other airway methods, such as endotracheal intubation, are impossible or have failed.
It is typically performed in life-threatening “cannot intubate, cannot ventilate” situations, such as severe facial trauma, airway obstruction from swelling or burns, or massive bleeding.
While generally considered a temporary measure due to potential complications, a cricothyrotomy can be lifesaving by restoring ventilation until a more secure airway, such as a tracheostomy, is established. It is a critical concept in emergency and respiratory care.
When is a Cricothyrotomy Performed?
A cricothyrotomy is typically indicated in “cannot intubate, cannot ventilate” scenarios. Some examples include:
- Severe facial trauma obstructing access to the mouth or nose
- Airway obstruction caused by swelling, burns, or anaphylaxis
- Upper airway tumors or structural abnormalities
- Failed attempts at endotracheal intubation
- Massive maxillofacial bleeding that makes airway visualization impossible
Note: In these critical situations, the procedure provides immediate, lifesaving oxygenation until a more permanent airway can be established.
Cricothyrotomy vs. Tracheostomy
Although both procedures involve creating a surgical opening in the airway, they differ significantly:
- Cricothyrotomy is performed quickly through the cricothyroid membrane in emergencies and is considered a temporary airway.
- Tracheostomy is a more controlled, planned procedure performed in an operating room or ICU setting through the trachea, typically for long-term airway management.
Note: This distinction highlights the urgent, short-term nature of cricothyrotomy compared to the sustained role of tracheostomy.
Why is Cricothyrotomy Relevant to Respiratory Therapists?
While respiratory therapists are not typically the primary providers performing a cricothyrotomy, their role surrounding the procedure is critical. Here’s why:
1. Airway Expertise
Respiratory therapists are highly trained in airway anatomy, mechanical ventilation, and oxygen delivery systems. This knowledge makes them key contributors to the airway management team during emergencies.
2. Equipment Preparation and Support
RTs often prepare and set up airway devices, suction, and mechanical ventilators. In the case of a cricothyrotomy, they may assist by preparing equipment and ensuring immediate ventilation and oxygenation once the airway is established.
3. Post-Procedural Care
Once the cricothyrotomy is in place, respiratory therapists play a major role in:
- Connecting the airway to appropriate oxygen delivery systems
- Monitoring gas exchange through blood gases and ventilator parameters
- Providing suctioning and secretion management
- Educating the care team on ventilator settings appropriate for the newly established airway
4. Patient Advocacy and Safety
Respiratory therapists often serve as the first to recognize signs of airway failure or compromised ventilation. Their vigilance can help escalate care quickly, ensuring a cricothyrotomy is performed without delay when needed.
Importance in the Field of Respiratory Care
Understanding cricothyrotomy is vital for respiratory therapists for several reasons:
- Emergency Preparedness: Knowing when and why a cricothyrotomy may be necessary enhances collaboration in high-stress scenarios.
- Interdisciplinary Collaboration: RTs work closely with physicians, nurses, and emergency personnel during airway crises, and understanding the procedure strengthens team communication.
- Clinical Competence: Even though RTs may not make the incision, they must be proficient in managing and stabilizing patients who undergo cricothyrotomy.
- Educational Role: RTs often teach patients, families, and healthcare students about airway management. Familiarity with cricothyrotomy supports their role as educators.
Cricothyrotomy Practice Questions
1. What is a cricothyrotomy?
It is an emergency procedure where an incision is made through the cricothyroid membrane to provide direct access to the trachea and restore ventilation.
2. In what type of situation is a cricothyrotomy typically performed?
In “cannot intubate, cannot ventilate” emergencies such as airway obstruction, severe facial trauma, or failed intubation attempts.
3. What anatomical landmark is used for a cricothyrotomy?
The cricothyroid membrane, located between the thyroid and cricoid cartilages.
4. Why is a cricothyrotomy considered a temporary airway solution?
Because it has higher risks of complications and is usually replaced with a more secure airway, like a tracheostomy.
5. Which airway emergency may require a cricothyrotomy due to swelling?
Anaphylaxis or thermal airway burns.
6. How does cricothyrotomy differ from tracheostomy?
Cricothyrotomy is a rapid, emergency airway through the cricothyroid membrane, while tracheostomy is a planned, long-term airway through the trachea.
7. Which condition would make endotracheal intubation difficult, leading to cricothyrotomy?
Massive maxillofacial bleeding or trauma obscuring the airway.
8. What patient symptom may signal the need for a cricothyrotomy?
Severe respiratory distress with complete upper airway obstruction.
9. What is the primary purpose of a cricothyrotomy?
To quickly restore oxygen delivery to the lungs in a life-threatening airway emergency.
10. Which professional typically performs a cricothyrotomy?
A physician, usually in emergency medicine, surgery, or critical care.
11. What role do respiratory therapists play during a cricothyrotomy?
They assist with equipment preparation, ventilation setup, and post-procedure airway management.
12. What is one complication that can occur after a cricothyrotomy?
Damage to nearby structures such as the vocal cords or thyroid gland.
13. How does a cricothyrotomy restore ventilation compared to bag-mask ventilation?
It bypasses upper airway obstruction, allowing direct passage of air into the trachea.
14. What equipment is commonly used to maintain a cricothyrotomy airway?
A small tracheostomy tube or a specialized cricothyrotomy kit tube.
15. What monitoring tool is essential after a cricothyrotomy is established?
Arterial blood gases (ABGs) or capnography to assess ventilation and oxygenation.
16. Why is synchronization with the R wave not relevant to cricothyrotomy?
Because it is a surgical airway procedure, not an electrical intervention like cardioversion.
17. What step should be taken immediately after securing the airway through a cricothyrotomy?
Connect the tube to oxygen or a ventilator and confirm placement with capnography.
18. Why might a cricothyrotomy be preferred over a tracheostomy in emergencies?
It is faster, requires less dissection, and provides immediate airway access.
19. What post-procedure care is critical for patients with a cricothyrotomy?
Airway suctioning, ventilator management, and monitoring for complications like bleeding or infection.
20. How does understanding cricothyrotomy benefit respiratory therapists in critical care?
It improves emergency preparedness, interdisciplinary teamwork, and patient safety during airway crises.
21. What is the definition of a cricothyrotomy?
The establishment of a surgical airway through the cricothyroid membrane.
22. What are the two main types of cricothyrotomy?
Open surgical and percutaneous.
23. What is an open surgical cricothyrotomy?
An airway created by making a surgical incision in the cricothyroid membrane and inserting a cuffed tracheostomy tube or endotracheal tube.
24. What is a percutaneous cricothyrotomy?
An airway created using the Seldinger technique or a large-bore needle (12–16 gauge), often leading to higher work of breathing.
25. Why are cricothyrotomies performed?
As a last resort when other methods fail, usually in “cannot intubate, cannot oxygenate” (CICO) emergencies.
26. How long should a cricothyrotomy remain in place?
Less than 24 hours, before conversion to a more permanent airway such as a tracheostomy.
27. What factors should be considered before performing a cricothyrotomy?
Effectiveness, anatomical limitations, underlying pathology, and patient age (children <10 years may require needle cric).
28. What is the most common indication for a cricothyrotomy?
A failed airway when intubation and ventilation attempts are unsuccessful.
29. What is an absolute contraindication for surgical cricothyrotomy?
Age under 10 years.
30. What is the preferred cricothyrotomy method for children under 10 years old?
Percutaneous needle cricothyrotomy.
31. What is the preferred airway technique for children under 5 years old?
Needle cricothyrotomy only.
32. What are relative contraindications for cricothyrotomy?
Preexisting laryngeal or tracheal disease, hematoma, coagulopathy, or lack of trained personnel.
33. What is the scalpel-finger-bougie technique?
A surgical cricothyrotomy method where a scalpel incision is made, a finger identifies the airway, and a bougie guides tube placement.
34. What are the basic steps of a surgical cricothyrotomy?
Palpate landmarks, make a skin incision, incise the membrane, apply traction, and insert the airway tube.
35. What is the procedure for a percutaneous cricothyrotomy?
Identify landmarks, stabilize the larynx, insert a transtracheal needle, advance the catheter, confirm placement, and connect to ventilation.
36. How are patients ventilated through a percutaneous cricothyrotomy?
Using percutaneous transtracheal jet ventilation or bag-valve ventilation.
37. How does percutaneous jet ventilation function?
A jet ventilator connects to a 50 psi source, delivering tidal volume with a 1:3 I:E ratio; exhalation occurs through the upper airway.
38. How can bag-valve ventilation be performed through a percutaneous cricothyrotomy?
By attaching a 30 mL syringe with an ETT connector to the catheter, allowing connection to a bag-valve device.
39. When is jet ventilation contraindicated?
In children under 5 years old, where bag-valve ventilation is preferred.
40. What does the acronym SMART stand for in predicting difficult cricothyrotomy?
Surgery, Mass, Access, Radiation, Tumor — conditions that complicate cricothyrotomy.
41. What are common short-term complications of cricothyrotomy?
Hemorrhage, tracheal injury, subcutaneous emphysema, pneumomediastinum, infection, or barotrauma.
42. What are potential long-term complications of cricothyrotomy?
Subglottic stenosis and voice changes.
43. What is the main complication associated with cricothyrotomy?
Misplacement of the airway tube.
44. Where can misplacement of the airway tube occur in cricothyrotomy?
Superior or inferior to the cricothyroid membrane, or through the posterior tracheal wall.
45. What traumatic conditions may indicate cricothyrotomy instead of intubation?
Severe maxillofacial injuries, cervical spine trauma, or airway obstruction from burns or swelling.
46. What type of airway device is typically placed after an open surgical cricothyrotomy?
A cuffed tracheostomy tube or endotracheal tube.
47. Why is cricothyrotomy considered a temporary airway solution?
Because of increased risks of complications and difficulty with long-term use.
48. In which clinical situation might cricothyrotomy be the only viable option?
When intubation is impossible and the patient cannot be ventilated, as in a complete upper airway obstruction.
49. Which age group should not undergo surgical cricothyrotomy?
Infants and children under 10 years old.
50. What type of ventilation support is often initiated immediately after cricothyrotomy placement?
Bag-valve ventilation or mechanical ventilation via the inserted tube.
51. What is the main difference between an open surgical and percutaneous cricothyrotomy?
Open surgical uses a scalpel incision with tube placement, while percutaneous uses a needle or Seldinger technique for rapid airway access.
52. In what type of situation is a cricothyrotomy considered the “last resort” airway?
In “cannot intubate, cannot oxygenate” (CICO) emergencies.
53. Why should a cricothyrotomy generally not be left in place longer than 24 hours?
Because of the increased risk of complications such as infection, stenosis, or tube misplacement.
54. What does the acronym SMART help predict in cricothyrotomy planning?
Potential anatomical or pathological barriers: Surgery, Mass, Access issues, Radiation, Tumor.
55. What is the absolute contraindication for open surgical cricothyrotomy?
Children under 10 years old.
56. What method of cricothyrotomy is preferred in children under 10 years old?
Percutaneous needle cricothyrotomy.
57. What is the only cricothyrotomy option for children under 5 years old?
Needle cricothyrotomy with bag-valve ventilation.
58. What type of catheter is typically used in a percutaneous cricothyrotomy?
A large-bore (12–16 gauge) IV catheter.
59. What is the purpose of transtracheal jet ventilation after a cricothyrotomy?
To provide tidal volume delivery through high-pressure oxygen flow.
60. Why is an I:E ratio of 1:3 used in jet ventilation?
To allow sufficient time for exhalation and prevent air trapping.
61. What complication can occur if air cannot escape during jet ventilation?
Barotrauma or pneumothorax.
62. Why is jet ventilation contraindicated in children under 5 years old?
Their small airways make exhalation inadequate, increasing the risk of barotrauma.
63. What is the safest method to ventilate a child under 5 years after needle cricothyrotomy?
Bag-valve ventilation with a small connector or modified adapter.
64. What is the primary clinical goal of a cricothyrotomy?
To restore oxygenation and ventilation in a life-threatening airway emergency.
65. What are the most common short-term complications of cricothyrotomy?
Hemorrhage, infection, subcutaneous emphysema, and tracheal injury.
66. What are the most significant long-term complications of cricothyrotomy?
Voice changes and subglottic stenosis.
67. Why is cricothyrotomy generally avoided in infants and small children?
Because their anatomy makes it difficult and dangerous, with higher complication rates.
68. During an open surgical cricothyrotomy, what is the first critical step?
Palpating and identifying the cricothyroid membrane.
69. What is the purpose of applying traction after making the membrane incision?
To maintain an opening and guide proper tube insertion.
70. How is placement confirmed after a cricothyrotomy tube is inserted?
By observing chest rise, auscultating breath sounds, and confirming with capnography.
71. What is the major risk of tube misplacement during cricothyrotomy?
Passing the tube superior, inferior, or posterior to the trachea.
72. What is a relative contraindication for cricothyrotomy in patients with neck trauma?
Preexisting laryngeal or tracheal injury.
73. Why is operator expertise important in cricothyrotomy?
Because incorrect technique increases risk of misplacement and complications.
74. What equipment is essential for percutaneous cricothyrotomy?
A large-bore needle, syringe, guidewire, and catheter.
75. What is the primary advantage of percutaneous over surgical cricothyrotomy?
It can be performed rapidly with minimal equipment at the bedside.
76. What is a potential downside of percutaneous cricothyrotomy compared to surgical?
It provides a smaller airway, which increases work of breathing.
77. What physical sign may indicate subcutaneous emphysema after cricothyrotomy?
Crepitus on palpation of the neck.
78. How can pneumomediastinum occur after cricothyrotomy?
From air leakage into mediastinal tissues due to high-pressure ventilation.
79. Why is early conversion to a tracheostomy recommended after cricothyrotomy?
To establish a more secure, long-term airway with fewer complications.
80. What is the key difference between cricothyrotomy and tracheostomy in clinical practice?
Cricothyrotomy is a temporary emergency procedure, while tracheostomy is a planned, long-term airway.
81. In what type of emergency is a cricothyrotomy typically performed before a tracheostomy?
When immediate airway access is needed and there is no time for surgical tracheostomy.
82. What feature makes the cricothyroid membrane a good site for emergency airway access?
It is superficial, relatively avascular, and easy to palpate.
83. What physical exam maneuver helps locate the cricothyroid membrane?
Palpating downward from the thyroid cartilage (“Adam’s apple”) until the depression above the cricoid ring is felt.
84. What is the most common patient position for performing a cricothyrotomy?
Supine with the neck extended, if not contraindicated by trauma.
85. Why is cervical spine immobilization important in trauma patients needing cricothyrotomy?
To prevent worsening of potential spinal cord injury during airway access.
86. What is the primary benefit of using a bougie in a surgical cricothyrotomy?
It guides safe placement of the airway tube into the trachea.
87. What is the role of suction during a cricothyrotomy?
To clear blood, secretions, or debris for better visualization and airway placement.
88. What tube size is commonly recommended for adult cricothyrotomy placement?
A cuffed tube between 5.0–6.0 mm internal diameter.
89. What clinical sign indicates that a cricothyrotomy airway is functioning properly?
Adequate chest rise with ventilation and improved oxygen saturation.
90. What role do respiratory therapists play immediately after a cricothyrotomy?
They connect the airway to oxygen delivery or a ventilator and monitor gas exchange.
91. Why is misplacement of the tube a serious complication of cricothyrotomy?
Because it can lead to failed ventilation, hypoxia, or injury to surrounding structures.
92. What is the most reliable method to confirm correct tube placement in cricothyrotomy?
Continuous waveform capnography.
93. What medication is often required before cricothyrotomy in conscious patients?
Sedatives or paralytics for patient comfort and safety.
94. Why is cricothyrotomy sometimes referred to as a “surgical airway of last resort”?
Because it is only performed when all other airway methods have failed.
95. What type of ventilation pattern is recommended immediately after placing a cricothyrotomy tube?
Gentle, controlled ventilation to avoid barotrauma.
96. What complication can occur if the incision is made too high during cricothyrotomy?
Damage to the vocal cords or thyroid cartilage.
97. What complication can occur if the incision is made too low during cricothyrotomy?
Accidental tracheostomy with risk of posterior tracheal wall injury.
98. What is the survival benefit of cricothyrotomy in airway obstruction?
It bypasses the blocked upper airway and allows immediate oxygen delivery.
99. What is one of the earliest signs of cricothyrotomy tube obstruction?
Increasing airway pressures or poor chest rise with ventilation.
100. What long-term follow-up may be needed for patients after cricothyrotomy?
Evaluation for subglottic stenosis, scar tissue formation, or voice changes.
Final Thoughts
Cricothyrotomy is not a routine procedure, but in the rare cases when it is required, it becomes the most crucial intervention for patient survival. For respiratory therapists, understanding the anatomy, indications, and post-procedural care associated with cricothyrotomy ensures they can respond effectively as part of the airway management team.
By mastering both the technical knowledge and supportive care surrounding this emergency intervention, respiratory therapists reinforce their role as indispensable professionals in respiratory and critical care medicine.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- McMahon K, Tariq A, Morley EJ. Cricothyroidotomy. [Updated 2025 Apr 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.