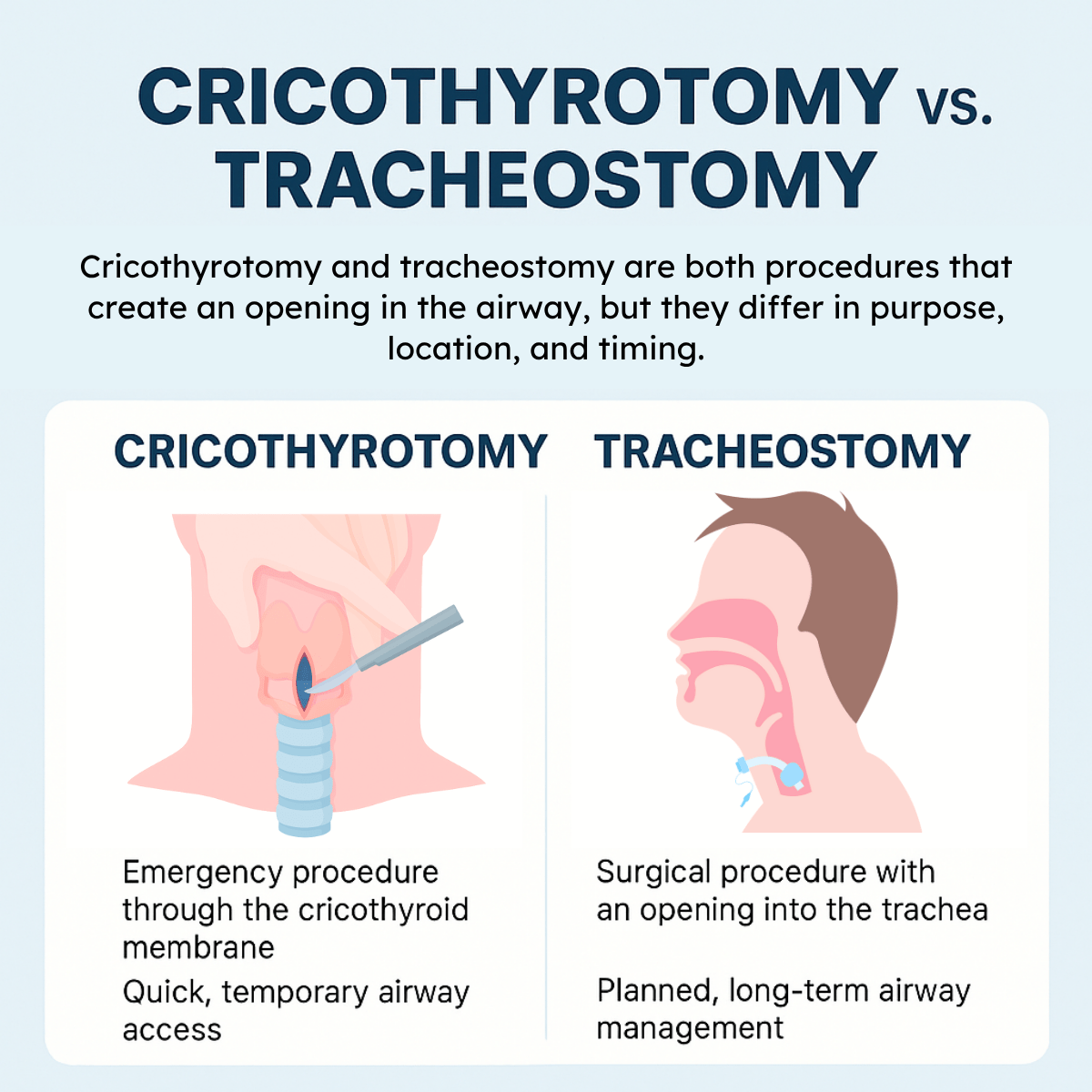
When a patient’s airway becomes compromised, healthcare providers may need to establish an alternate route for breathing. Two commonly discussed procedures are cricothyrotomy and tracheostomy.
While both involve creating an opening in the airway to allow air to reach the lungs, they serve different purposes, are performed in different locations, and are used in different clinical situations.
Understanding the distinction between the two is essential for both medical professionals and students, as it highlights not only the urgency and temporary nature of a cricothyrotomy but also the planned, long-term role of a tracheostomy in patient care.
Download our free guide that has over 100+ of the best tips for healthy lungs.
What is the Difference Between a Cricothyrotomy and a Tracheostomy?
A cricothyrotomy and a tracheostomy are both procedures that create an opening in the airway, but they differ in purpose, location, and timing. A cricothyrotomy is an emergency procedure performed through the cricothyroid membrane, just below the Adam’s apple, to provide rapid airway access when other methods fail. It is quick and lifesaving but generally considered temporary due to risks of complications if left in place.
A tracheostomy, on the other hand, is a surgical procedure done in a controlled setting where an opening is made directly into the trachea, usually between the second and third tracheal rings. It is designed for long-term airway management in patients who require prolonged mechanical ventilation or have upper airway obstructions.
Overview of Cricothyrotomy and Tracheostomy
Cricothyrotomy and tracheostomy are both surgical procedures designed to secure an airway. Each has specific indications, anatomical targets, and risks, influencing their use in emergency and planned contexts.
Cricothyrotomy
Cricothyrotomy is an emergency airway procedure that involves making an incision through the skin and the cricothyroid membrane. This membrane connects the thyroid cartilage to the cricoid cartilage in the neck.
The goal is to establish a rapid airway when intubation is not possible or has failed. The procedure is typically performed in acute, life-threatening situations like severe facial trauma or airway obstruction. It is faster and less complex than tracheostomy but is considered a temporary measure.
Tracheostomy
Tracheostomy is a surgical procedure that creates a direct airway through an incision in the trachea, below the cricoid cartilage. This is usually done in a controlled, non-emergency setting.
It provides a long-term airway for patients needing prolonged ventilation or airway protection. The stoma allows for better airway management, secretion clearance, and reduced airway resistance compared to endotracheal tubes.
Indications and Contraindications
Both cricothyrotomy and tracheostomy are airway management techniques used in critical situations. Their choice depends on the patient’s condition, urgency, and anatomical considerations.
Indications for a Cricothyrotomy
Cricothyrotomy is primarily indicated in emergency scenarios when endotracheal intubation is impossible or has failed. Examples include severe facial trauma, airway obstruction from swelling or foreign bodies, and upper airway burns.
It is favored when immediate airway access is required due to its rapid and relatively simple procedure. Cricothyrotomy can also be indicated in prehospital settings where rapid airway control is essential.
Note: It is not suitable for prolonged airway support but provides a vital bridge until definitive airway management is possible.
Indications for a Tracheostomy
Tracheostomy is indicated for long-term airway management, especially in patients requiring extended ventilation support. It is also appropriate in cases of upper airway obstruction below the level manageable by cricothyrotomy.
Patients with tumors, congenital anomalies, or stenosis in the upper airway often require tracheostomy. It is used electively when prolonged airway access is anticipated.
Note: A tracheostomy may also be indicated to facilitate airway clearance in patients unable to protect their airway due to neurological impairment.
Contraindications for a Cricothyrotomy
Cricothyrotomy is contraindicated in children under 12 years due to the risk of damaging the cricoid cartilage and the small size of the cricothyroid membrane. It should be avoided in cases where the anatomy is distorted by tumors, abscesses, or previous surgery in the neck. Severe coagulopathy increases bleeding risk and is a relative contraindication.
If an alternative airway can be established safely, cricothyrotomy is not preferred due to its temporary nature and potential complications like subglottic stenosis.
Contraindications for a Tracheostomy
Tracheostomy is contraindicated in uncontrolled neck infections or cellulitis due to the risk of spreading infection. Patients with uncorrected coagulopathy are at higher risk for bleeding complications.
Anatomical abnormalities such as a short neck or a high-riding innominate artery can pose significant risks. Tracheostomy is also less suitable in emergency airway situations requiring immediate access due to its more complex procedure. In some cases, tracheostomy may be deferred until the patient is stable enough to tolerate the surgery.
Procedural Techniques
Both cricothyrotomy and tracheostomy involve creating an airway through the neck but differ in anatomical site, urgency, and complexity. Each requires precise steps and specific tools to ensure patient safety and airway patency.
Step-by-Step Cricothyrotomy Procedure
The patient is positioned supine with neck extension to expose the cricothyroid membrane. The provider palpates the membrane, located between the thyroid and cricoid cartilages. After cleaning the area, a vertical skin incision is made over the membrane. A horizontal incision is then performed through the cricothyroid membrane itself.
A dilator or finger is used to enlarge the opening, followed by insertion of a cuffed endotracheal tube or tracheostomy tube. Proper tube placement is confirmed by ventilation and breath sounds. The procedure typically takes under 5 minutes and is used in emergent airway obstruction.
Step-by-Step Tracheostomy Procedure
The patient lies supine with neck extended. The provider identifies the tracheal rings, usually between the second and third or third and fourth rings. A horizontal or vertical neck incision is made, and subcutaneous tissues are dissected to expose the trachea. Care is taken to avoid damage to the thyroid isthmus and other vital structures.
A window or flap is created in the tracheal wall. Then, a tracheostomy tube is inserted through the opening and secured. The tube is connected to ventilation, and placement is verified by capnography and breath sounds. This procedure is more controlled and used in planned or prolonged airway management.
Required Equipment
For cricothyrotomy, essential equipment includes a scalpel (typically size 11 or 10), a tracheal dilator or hemostat, and a cuffed endotracheal or tracheostomy tube (6.0–7.0 mm internal diameter).
Tracheostomy requires a scalpel, hemostats, curved scissors, tracheal dilator, tracheostomy tubes of various sizes, suction apparatus, and sterile drapes. Sterile gloves and local anesthetic are also crucial.
Note: Both procedures require oxygen delivery and monitoring equipment immediately before and after tube placement. Proper preparation reduces complications and improves success rates.
Risks and Complications
Both cricothyrotomy and tracheostomy involve significant risks that vary depending on timing and technique. Complications can occur immediately during the procedure or develop over time, and strategies exist to reduce these risks.
Immediate Complications
Cricothyrotomy carries risks such as bleeding, misplacement of the airway tube, and injury to the vocal cords or thyroid gland. It can also cause subcutaneous emphysema or pneumothorax if air escapes into surrounding tissues.
Tracheostomy risks during insertion include hemorrhage, damage to the trachea or nearby blood vessels, and accidental puncture of the esophagus. Both procedures can result in airway obstruction if the tube becomes blocked or dislodged.
Long-Term Complications
Tracheostomies pose risks like tracheal stenosis, infection around the stoma site, and formation of granulation tissue. Prolonged use can lead to tracheomalacia or fistula development between the trachea and esophagus.
Cricothyrotomy, typically a temporary measure, may lead to scarring or voice changes if left for an extended period. Long-term complications are less frequent due to its emergency use but can occur if converted late to a formal tracheostomy.
Risk Mitigation Strategies
Proper technique and anatomical knowledge are essential to minimize injury during both procedures. Use of ultrasound or imaging, when available, reduces the risk of vascular injury.
Prompt conversion from cricothyrotomy to tracheostomy lowers long-term risks. Routine tube care, infection control, and monitoring for complications guide safer tracheostomy management. Training and simulation improve procedural success and decrease complication rates.
Recovery and Aftercare
Recovery from cricothyrotomy and tracheostomy requires close attention to airway stability, infection prevention, and proper healing. Patients need specific monitoring and care practices to avoid complications and ensure optimal outcomes.
Post-Procedure Management
After either procedure, securing the airway and monitoring respiratory status are priorities. Vital signs, oxygen saturation, and signs of airway obstruction must be assessed frequently. Pain management is important, but sedatives should be used cautiously to avoid respiratory depression. The patient may require humidified oxygen to prevent drying of airway mucosa.
Regular suctioning of secretions minimizes blockage risk. Nurses and caregivers must be trained and vigilant, especially during the initial 48-72 hours when complications are more common.
Wound Care Considerations
The incision site requires daily inspection for redness, swelling, or discharge indicating infection. Sterile technique is essential during dressing changes to reduce contamination risk.
Moist wound care with non-adherent dressings supports epithelialization without damaging surrounding tissues. Both cricothyrotomy and tracheostomy wounds may develop granulation tissue needing medical evaluation.
Patients or caregivers should be instructed on signs of infection: fever, increased pain, or foul-smelling drainage. Early intervention improves healing outcomes and minimizes hospital stays.
Decannulation Process
Decannulation timing depends on the patient’s ability to maintain airway patency and effective cough. For cricothyrotomy, this often occurs once swelling subsides and airway obstruction resolves.
Tracheostomy decannulation involves gradual downsizing of the tube while monitoring breathing and oxygen levels. Capping trials test the patient’s tolerance before tube removal.
Close supervision post-decannulation is vital to identify respiratory distress early. Follow-up includes airway assessments and possible rehabilitation for voice and swallowing functions.
Comparative Outcomes and Prognosis
Cricothyrotomy and tracheostomy differ significantly in their immediate results, long-term effects, and impact on daily living. Each procedure’s effectiveness and risks must be considered, depending on the clinical situation and patient needs.
Short-Term Outcomes
Cricothyrotomy provides rapid airway access, often within 1-3 minutes, making it vital in emergency settings where time is critical. It carries a higher risk of bleeding, infection, and injury to vocal cords due to the procedure’s proximity to delicate structures.
Tracheostomy requires more time to perform but generally results in a more stable airway with less acute trauma. However, it is associated with risks like pneumothorax and tracheal cartilage damage, though these are less common than in cricothyrotomy.
Long-Term Prognosis
Long-term complications from cricothyrotomy are more frequent, including subglottic stenosis and voice changes because of its incision site. Many emergency cricothyrotomies require conversion to tracheostomies for sustained airway management.
Tracheostomy offers better long-term airway maintenance with fewer strictures or scarring. It supports prolonged ventilation and speaking valve use, making it preferable when extended airway support is anticipated.
Patient Quality of Life
Cricothyrotomy often leads to temporary disruptions in voice and swallowing function, impacting quality of life in the early recovery phase. Due to potential complications, ongoing monitoring is essential to avoid chronic issues.
Patients with tracheostomies may experience better overall comfort and mobility with appropriate care. They can engage in speech and eating activities more effectively, but require regular stoma care and monitoring to prevent infections.
FAQs About a Cricothyrotomy vs. Tracheostomy
Is a Cricothyrotomy and a Tracheostomy the Same?
No, a cricothyrotomy and a tracheostomy are not the same. A cricothyrotomy is an emergency procedure where an opening is made through the cricothyroid membrane to quickly establish an airway. It is typically temporary and used only when other methods, such as intubation, have failed.
A tracheostomy, however, is a surgical procedure performed in a controlled setting, where an opening is created directly into the trachea. It is intended for long-term airway management in patients who need ongoing support.
What Are the Risks of a Cricothyrotomy?
Cricothyrotomy is lifesaving but carries certain risks, especially because it is often performed under emergency conditions. Potential complications include bleeding, damage to nearby structures such as the vocal cords or thyroid gland, infection, and airway scarring.
Misplacement of the tube can also occur, leading to inadequate ventilation. Since the cricothyroid membrane is close to critical structures, precision is essential. Additionally, cricothyrotomy is generally considered a temporary solution, as prolonged use increases the risk of airway injury and long-term complications.
What Are the Complications of a Tracheostomy?
A tracheostomy, while generally safe when performed in a surgical setting, can still lead to complications. Early risks include bleeding, infection, accidental tube dislodgement, or injury to the esophagus or major blood vessels.
Long-term complications may include tracheal narrowing (stenosis), tracheoesophageal fistula, or difficulty speaking and swallowing.
Blockage of the tracheostomy tube by mucus plugs can also be dangerous. However, with proper care and monitoring, many complications can be prevented, making tracheostomy a reliable method for long-term airway management.
Are There Alternatives to Cricothyrotomy and Tracheostomy?
Yes, there are alternatives, though they depend on the clinical situation. Endotracheal intubation through the mouth or nose is the most common method for establishing an airway and is usually attempted first.
In cases where intubation fails, noninvasive ventilation, such as CPAP or BiPAP, may be considered if the patient is stable enough. In rare cases, advanced techniques such as retrograde intubation or the use of supraglottic airway devices can serve as temporary measures. However, in emergencies, cricothyrotomy remains the definitive option.
When Is a Tracheostomy Used?
A tracheostomy is typically used when patients require long-term ventilatory support or have upper airway obstructions that prevent normal breathing. It may be indicated in conditions such as severe head or neck trauma, vocal cord paralysis, or chronic respiratory failure requiring prolonged mechanical ventilation.
Tracheostomy can also help patients with neuromuscular diseases who have difficulty clearing secretions. Beyond airway support, it improves patient comfort compared to prolonged intubation and allows for easier communication and swallowing rehabilitation in certain cases.
When Is a Cricothyrotomy Used?
A cricothyrotomy is used in life-threatening emergencies when other methods of securing an airway, such as intubation, are not possible or have failed. It is often performed in cases of severe facial trauma, airway obstruction, or swelling (such as anaphylaxis) that prevents passage of a breathing tube.
The procedure is chosen because it can be performed quickly with minimal equipment. Unlike a tracheostomy, it is not intended for long-term use but rather as a rapid intervention to save a patient’s life.
Which Is More Dangerous, a Cricothyrotomy or a Tracheostomy?
Both procedures carry risks, but a cricothyrotomy is generally considered more dangerous due to the emergency circumstances under which it is performed. The urgency often leaves little time for preparation or precision, increasing the risk of injury to nearby structures, bleeding, or misplacement of the airway.
A tracheostomy, on the other hand, is usually performed in a controlled surgical environment, making it safer and more suitable for long-term management. While both have potential complications, cricothyrotomy is typically riskier and more temporary.
Final Thoughts
Although cricothyrotomy and tracheostomy both provide direct access to the airway, they are distinct in their indications, techniques, and intended duration of use. Cricothyrotomy is a rapid, emergency procedure performed when immediate airway access is needed, while tracheostomy is a more controlled surgical intervention designed for long-term management.
Recognizing these differences is vital for safe clinical practice and ensures that patients receive the appropriate intervention based on their condition and needs.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- McMahon K, Tariq A, Morley EJ. Cricothyroidotomy. [Updated 2025 Apr 18]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.
- Raimonde AJ, Gaston S, Wang CF. Tracheostomy. [Updated 2025 Sep 15]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.