Diaphoresis refers to excessive, often profuse sweating that occurs beyond what the body needs for normal temperature regulation. While sweating is a natural response to heat or exercise, diaphoresis can be a clinical sign of an underlying medical condition.
For healthcare professionals, and especially respiratory therapists, recognizing diaphoresis is important because it can serve as a subtle but critical indicator of respiratory distress, cardiovascular compromise, or other systemic issues that require urgent attention.
What is Diaphoresis?
Diaphoresis is the medical term for excessive sweating that goes beyond what is necessary to regulate body temperature. Unlike normal perspiration from heat or exercise, diaphoresis often arises suddenly and can signal an underlying health problem.
It is typically caused by activation of the sympathetic nervous system, which may occur with fever, pain, anxiety, or serious medical conditions such as a heart attack, hypoxemia, or infection.
In respiratory care, diaphoresis is especially important because it may indicate that a patient is experiencing increased work of breathing, low oxygen levels, or systemic instability. Recognizing diaphoresis helps respiratory therapists identify patients in distress, monitor disease progression, and intervene early to prevent further complications.
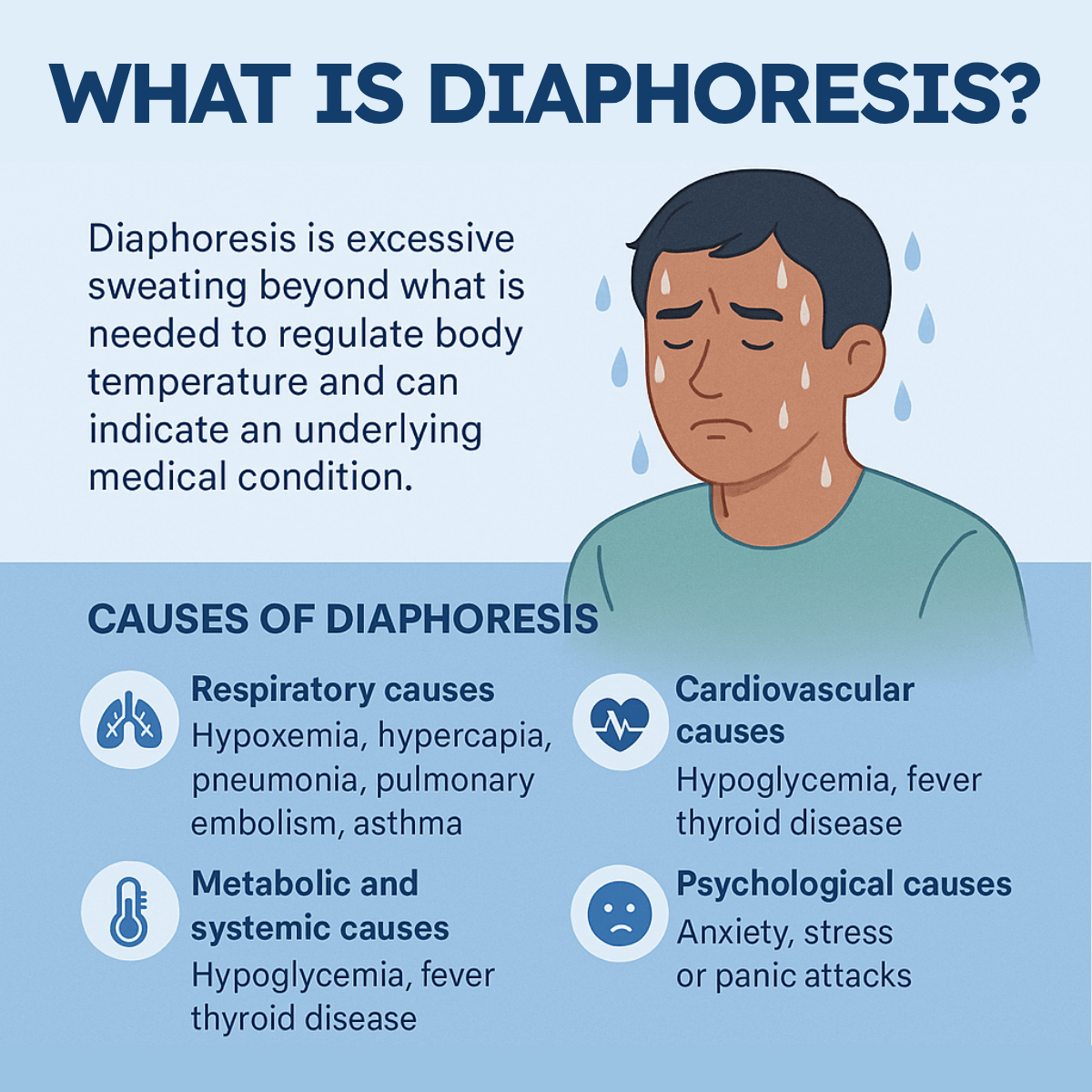
Causes of Diaphoresis
Diaphoresis can occur due to a wide range of medical conditions, many of which overlap with respiratory care:
- Respiratory causes: Hypoxemia, hypercapnia, pneumonia, pulmonary embolism, asthma exacerbations, and acute COPD flare-ups
- Cardiovascular causes: Myocardial infarction, shock, arrhythmias, heart failure
- Metabolic and systemic causes: Hypoglycemia, fever, infection, thyroid disease, and certain medications
- Psychological causes: Anxiety, stress, or panic attacks, which can also trigger acute dyspnea
Clinical Relevance in Respiratory Care
For respiratory therapists, diaphoresis is more than just a physical sign—it can be a clue to worsening patient status. Here’s why it matters:
1. Indicator of Increased Work of Breathing
When patients are in respiratory distress, they often recruit accessory muscles and expend significant energy just to maintain ventilation. This increased metabolic demand can trigger diaphoresis, even in a cool environment. A diaphoretic patient may be struggling with inadequate oxygenation or ventilation.
2. Early Warning Sign of Hypoxemia or Hypercapnia
Excessive sweating can accompany low oxygen saturation (SpO₂) or elevated carbon dioxide (PaCO₂). If a patient becomes diaphoretic along with tachypnea, tachycardia, or cyanosis, it signals the need for immediate assessment and possible escalation of respiratory support.
3. Marker of Systemic Instability
Diaphoresis often coexists with other signs of hemodynamic compromise, such as hypotension, tachycardia, or altered mental status. For example, a patient with diaphoresis and chest pain may be experiencing a myocardial infarction, which requires coordinated cardiopulmonary intervention.
4. Response to Medications and Therapies
Some medications used in respiratory care, such as bronchodilators (e.g., albuterol), can cause tremors and sweating as side effects. Recognizing whether diaphoresis is related to drug therapy versus worsening respiratory status helps guide proper clinical decisions.
Assessment and Monitoring
Respiratory therapists should be attentive to diaphoresis as part of a broader patient assessment. Key steps include:
- Observation: Note the presence, severity, and timing of sweating
- Vital signs: Check SpO₂, respiratory rate, heart rate, and blood pressure
- ABGs and labs: Evaluate oxygenation, ventilation, and metabolic balance
- Clinical correlation: Determine whether diaphoresis is associated with respiratory distress, cardiovascular instability, or systemic illness
Clinical Scenarios in Respiratory Care
- A patient with an acute COPD exacerbation who is diaphoretic, tachypneic, and using accessory muscles may require noninvasive ventilation or intubation
- A patient with suspected pulmonary embolism may present with sudden shortness of breath, chest pain, diaphoresis, and hypoxemia, signaling the need for rapid intervention
- A postoperative patient who becomes diaphoretic while desaturating could be experiencing atelectasis, pneumonia, or another respiratory complication
Diaphoresis Practice Questions
1. What is diaphoresis?
The medical term for excessive sweating that goes beyond what is needed to regulate body temperature.
2. How does diaphoresis differ from normal perspiration?
It often occurs suddenly, without heat or exercise, and may signal an underlying health problem.
3. What part of the nervous system typically triggers diaphoresis?
The sympathetic nervous system.
4. What are some common respiratory causes of diaphoresis?
Hypoxemia, hypercapnia, pneumonia, pulmonary embolism, asthma exacerbations, and COPD flare-ups.
5. What cardiovascular conditions can cause diaphoresis?
Myocardial infarction, shock, arrhythmias, and heart failure.
6. What metabolic or systemic causes may lead to diaphoresis?
Hypoglycemia, fever, infection, thyroid disease, and certain medications.
7. What psychological factors can trigger diaphoresis?
Anxiety, stress, and panic attacks.
8. Why is diaphoresis clinically relevant in respiratory care?
It can be an early sign of respiratory distress, hypoxemia, hypercapnia, or systemic instability.
9. How does increased work of breathing contribute to diaphoresis?
The body expends extra energy using accessory muscles, raising metabolic demand and causing sweating.
10. What other symptoms often accompany diaphoresis in respiratory distress?
Tachypnea, tachycardia, accessory muscle use, and cyanosis.
11. Why is diaphoresis an early warning sign of hypoxemia?
Because low oxygen levels can trigger sympathetic activation, leading to sweating.
12. How can hypercapnia present alongside diaphoresis?
Patients may become flushed, confused, and sweaty due to elevated carbon dioxide levels.
13. What systemic signs may accompany diaphoresis in unstable patients?
Hypotension, tachycardia, and altered mental status.
14. What condition should be suspected in a diaphoretic patient with chest pain?
Myocardial infarction
15. Which respiratory therapy medication may cause diaphoresis as a side effect?
Albuterol (a bronchodilator)
16. How can clinicians distinguish between medication side effects and clinical deterioration when diaphoresis occurs?
By correlating symptoms with vital signs, oxygenation status, and other clinical findings.
17. What vital signs should be checked when a patient is diaphoretic?
Respiratory rate, heart rate, blood pressure, and oxygen saturation (SpO₂).
18. What lab tests may be useful in evaluating a diaphoretic patient?
Arterial blood gases (ABGs) and metabolic panels.
19. What does diaphoresis combined with desaturation in a postoperative patient suggest?
Possible atelectasis, pneumonia, or another respiratory complication.
20. What condition may present with sudden shortness of breath, chest pain, hypoxemia, and diaphoresis?
Pulmonary embolism
21. Why is diaphoresis often associated with increased sympathetic activity?
Because activation of the sympathetic nervous system stimulates sweat glands.
22. What does diaphoresis during mild activity or rest usually suggest?
An underlying medical condition rather than normal thermoregulation.
23. In which type of shock is diaphoresis a classic symptom?
Cardiogenic shock
24. Why might a patient with hypoglycemia present with diaphoresis?
Low blood sugar activates the sympathetic nervous system, triggering sweating.
25. What is a key difference between diaphoresis caused by fever and that caused by hypoxemia?
Fever-related sweating follows temperature elevation, while hypoxemia-related sweating occurs suddenly with respiratory distress.
26. How can anxiety-induced diaphoresis be differentiated from medical causes?
By ruling out hypoxemia, abnormal vital signs, or systemic illness.
27. What does diaphoresis combined with tachycardia and low SpO₂ typically indicate?
Respiratory compromise requiring urgent intervention.
28. Why is diaphoresis considered a nonspecific clinical sign?
Because it can result from multiple systems including respiratory, cardiac, metabolic, and psychological causes.
29. What finding in a COPD patient is especially concerning when accompanied by diaphoresis?
Accessory muscle use and tachypnea, suggesting impending respiratory failure.
30. Why is it important for respiratory therapists to document diaphoresis?
Because it can indicate worsening respiratory or systemic instability.
31. What type of pneumonia might present with diaphoresis, fever, and productive cough?
Bacterial pneumonia
32. How can diaphoresis complicate physical examinations?
It may interfere with monitoring equipment such as ECG electrodes or pulse oximetry sensors.
33. Why does diaphoresis increase metabolic water and electrolyte loss?
Because excessive sweating removes sodium, potassium, and fluids from the body.
34. What is the potential danger of ignoring diaphoresis in a patient receiving oxygen therapy?
It may be a missed sign of hypoxemia or increased work of breathing.
35. What does diaphoresis during nocturnal episodes of breathlessness suggest?
Possible heart failure with paroxysmal nocturnal dyspnea.
36. How can opioids contribute to diaphoresis?
By depressing respiratory drive and triggering hypoxemia or as a direct side effect.
37. What critical illness often presents with diaphoresis, hypotension, and altered mental status?
Sepsis
38. How does diaphoresis present in patients with thyroid disease?
Hyperthyroidism may cause excessive sweating due to increased metabolism.
39. What common anxiety-related condition often involves diaphoresis and shortness of breath?
Panic attacks
40. Why should sudden onset of diaphoresis in a patient with stable vitals still be taken seriously?
Because it may precede rapid deterioration.
41. What type of myocardial infarction commonly presents with diaphoresis?
Acute ST-elevation myocardial infarction (STEMI).
42. What should be the first step if a diaphoretic patient also shows cyanosis?
Assess oxygenation and provide immediate respiratory support.
43. Why does diaphoresis indicate increased oxygen consumption in the body?
Because sweating itself increases metabolic activity.
44. What role does diaphoresis play in evaluating patient response during pulmonary rehabilitation?
It may indicate overexertion or poor oxygen delivery.
45. How might diaphoresis interfere with noninvasive ventilation (NIV) use?
Sweating can reduce mask seal effectiveness and patient comfort.
46. What should be done if a patient becomes diaphoretic while on bronchodilator therapy?
Evaluate whether the sweating is a medication side effect or a sign of worsening respiratory status.
47. Why is it important to correlate diaphoresis with arterial blood gas results?
Because ABGs can confirm hypoxemia, hypercapnia, or metabolic imbalance causing sweating.
48. What is a concerning finding if diaphoresis is accompanied by bradycardia?
Severe hypoxemia or advanced cardiac dysfunction.
49. How does diaphoresis differ from hyperhidrosis?
Diaphoresis is excessive sweating due to an underlying condition, while hyperhidrosis is chronic overactive sweating without systemic illness.
50. What should be the respiratory therapist’s immediate action if diaphoresis occurs with sudden desaturation?
Escalate oxygen therapy and assess for causes such as airway obstruction, pulmonary embolism, or acute respiratory failure.
51. Why might a patient with pulmonary embolism present with diaphoresis?
Because sudden obstruction in pulmonary circulation triggers sympathetic activation and distress.
52. What is the relationship between diaphoresis and hypoxemia in acute asthma?
Excessive sweating may indicate the patient is tiring and not ventilating effectively.
53. Why does diaphoresis sometimes signal impending respiratory failure?
Because it reflects severe work of breathing and metabolic stress.
54. How can diaphoresis assist in triaging patients in the emergency department?
It helps identify unstable patients who may require immediate intervention.
55. What is a potential complication of prolonged diaphoresis in critically ill patients?
Dehydration and electrolyte imbalance.
56. What does diaphoresis during mechanical ventilation suggest?
Possible hypoxemia, patient-ventilator asynchrony, or discomfort.
57. Why is diaphoresis a red flag during weaning trials from mechanical ventilation?
It can indicate fatigue, increased work of breathing, or intolerance of the trial.
58. What is the likely cause if diaphoresis occurs with a sudden drop in blood pressure?
Shock or hemodynamic collapse.
59. Why is diaphoresis a useful clinical sign in septic patients?
It often accompanies fever, tachycardia, and systemic inflammatory response.
60. How can diaphoresis provide an early warning of hypoglycemia in diabetic patients?
Sweating is one of the first autonomic symptoms before neuroglycopenia develops.
61. What role does diaphoresis play in post-operative monitoring?
It may signal pain, hypoxemia, or early infection.
62. Why should diaphoresis in a patient with tracheostomy be closely evaluated?
It could indicate airway obstruction, hypoxemia, or infection.
63. What condition should be suspected if diaphoresis occurs with pallor and dizziness?
Syncope or presyncope due to reduced perfusion.
64. Why might diaphoresis occur during chest physiotherapy?
Because the therapy increases energy expenditure and mobilizes secretions.
65. What should a therapist do if diaphoresis appears during bronchoscopy?
Assess for hypoxemia or anxiety and provide appropriate support.
66. How might diaphoresis complicate pulse oximetry readings?
Excess moisture can interfere with sensor adhesion and accuracy.
67. Why can diaphoresis be an important sign during sleep studies?
It may indicate nocturnal hypoxemia, apnea, or sympathetic surges.
68. What condition is suggested by diaphoresis, tremors, and palpitations together?
Hypoglycemia
69. Why is diaphoresis concerning in a patient receiving opioids?
It may indicate respiratory depression and hypoventilation.
70. What action should be taken if a COPD patient becomes diaphoretic while using accessory muscles?
Escalate respiratory support, possibly initiating noninvasive ventilation.
71. Why does diaphoresis increase oxygen demand?
Because sweating requires metabolic energy and raises workload on the body.
72. What systemic disorder can present with chronic excessive diaphoresis?
Hyperthyroidism
73. What diagnostic tool is most useful in correlating diaphoresis with hypoxemia?
Pulse oximetry
74. How does diaphoresis support the diagnosis of myocardial infarction?
It often occurs alongside chest pain, dyspnea, and hypotension.
75. Why is diaphoresis important to note during patient transport?
Because it may indicate deterioration requiring immediate intervention.
76. What condition may be suspected if diaphoresis occurs with flushing and wheezing?
Anaphylaxis
77. Why is diaphoresis during exertion concerning in cardiac patients?
It may indicate underlying ischemia or poor perfusion.
78. How can diaphoresis complicate noninvasive respiratory support?
Excess sweat can impair mask fit and reduce therapy effectiveness.
79. What does diaphoresis with altered mental status suggest?
Severe hypoxemia, hypercapnia, or shock.
80. Why should diaphoresis not be dismissed in anxious patients?
Because it may mask or coexist with a true medical emergency such as hypoxemia or MI.
81. Why does diaphoresis often appear in patients with advanced respiratory distress?
Because the body is under extreme sympathetic drive to maintain ventilation and oxygen delivery.
82. What is the clinical significance of diaphoresis during a pulmonary rehabilitation session?
It may signal that the patient is exceeding safe exercise tolerance.
83. Which neurological condition can present with diaphoresis due to autonomic dysfunction?
Parkinson’s disease
84. Why is diaphoresis an important observation during a 6-minute walk test?
It can indicate exertional hypoxemia or cardiovascular compromise.
85. How might diaphoresis be a side effect of antipyretic therapy?
As fever breaks, sweating occurs to lower body temperature.
86. Why is diaphoresis concerning in a patient undergoing intubation?
It may indicate hypoxemia, anxiety, or excessive sympathetic stimulation.
87. What systemic emergency often presents with diaphoresis and severe chest tightness?
Acute myocardial infarction.
88. Why does diaphoresis occur in patients experiencing severe pain?
Pain activates the sympathetic nervous system, increasing sweat production.
89. What gastrointestinal emergency may present with diaphoresis and abdominal pain?
Acute pancreatitis
90. Why might diaphoresis be observed during acute arrhythmias?
Because reduced cardiac output triggers sympathetic activation.
91. What endocrine disorder may cause diaphoresis due to increased catecholamine release?
Pheochromocytoma
92. How does diaphoresis help differentiate between stable and unstable angina?
Unstable angina often presents with diaphoresis, reflecting greater cardiac stress.
93. Why should diaphoresis in an elderly patient be carefully evaluated?
Because it may be a subtle sign of infection, sepsis, or cardiac ischemia.
94. What critical respiratory condition is suggested by diaphoresis and retractions in a pediatric patient?
Severe asthma exacerbation.
95. How does diaphoresis complicate patient comfort in the ICU?
It increases risk of skin breakdown and interferes with monitoring equipment.
96. What is the most likely explanation for diaphoresis after administration of epinephrine?
Sympathetic stimulation from the medication.
97. Why might a patient with pneumonia present with diaphoresis?
Because fever and increased metabolic demand stimulate sweating.
98. What should be suspected if diaphoresis occurs with unilateral chest pain and sudden hypoxemia?
Pneumothorax.
99. How does diaphoresis support the clinical suspicion of shock?
It reflects poor perfusion and high sympathetic activity.
100. Why is documenting diaphoresis essential in patient care notes?
Because it provides evidence of possible deterioration and guides urgent interventions.
Final Thoughts
Diaphoresis is an important clinical sign that respiratory therapists must not overlook. While it may seem non-specific, in the context of respiratory care, it often signals increased work of breathing, hypoxemia, or systemic compromise.
Careful assessment of diaphoresis, combined with vital signs, ABG analysis, and physical examination, helps guide timely interventions that can make the difference between stability and deterioration.
By remaining vigilant for diaphoresis and understanding its implications, respiratory therapists can play a key role in identifying distress early, ensuring patient safety, and improving outcomes in critical care and beyond.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Odeh M. Profuse diaphoresis as an important sign for the differential diagnosis of acute respiratory distress. Intensive Care Med. 1992.

