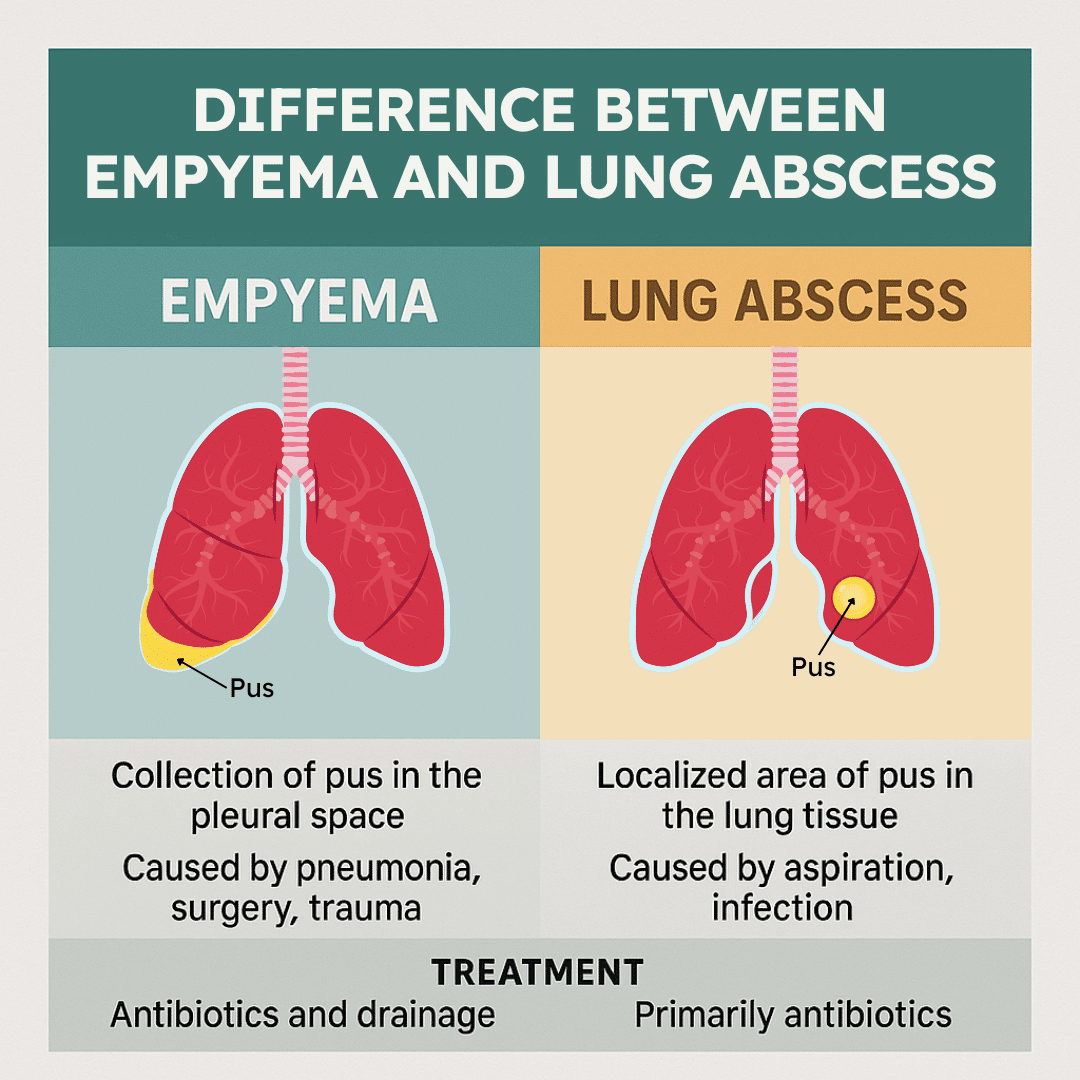
Empyema and lung abscess are two serious but distinct complications of pulmonary infection that can significantly impact respiratory health. While both involve the presence of pus and infection within the chest, their location, causes, and treatment strategies differ in important ways.
An empyema occurs when pus accumulates in the pleural space, the thin cavity surrounding the lungs, often as a complication of pneumonia or chest trauma. A lung abscess, on the other hand, develops as a localized pocket of pus within the lung tissue itself, typically due to aspiration or severe bacterial infection.
Understanding the differences between these conditions is essential for accurate diagnosis, timely treatment, and improved patient outcomes.
Download our free guide that has over 100+ of the best tips for healthy lungs.
What is the Difference Between an Empyema and a Lung Abscess?
An empyema and a lung abscess are both infections involving pus in the chest, but they differ in location and development. An empyema is a collection of pus within the pleural space, the thin cavity between the lung and chest wall, usually following pneumonia, surgery, or trauma. It results from bacteria spreading into this space, causing fluid buildup and impaired lung expansion.
In contrast, a lung abscess is a localized pocket of pus within the lung tissue itself, often caused by aspiration of oropharyngeal secretions or severe pneumonia.
While both conditions can present with fever, cough, and chest pain, treatment approaches differ, with empyema often requiring drainage and a lung abscess treated primarily with antibiotics.
What Is an Empyema?
An empyema is a collection of thick pus within the pleural space, the cavity between the lung and chest wall. It usually arises as a complication of pneumonia, lung surgery, or trauma, leading to infection in the pleural fluid.
The condition involves inflammation of the pleura and accumulation of purulent material, which can restrict lung expansion and cause systemic infection. Treatment often includes antibiotics and drainage procedures to remove pus from the pleural space.
What Is a Lung Abscess?
A lung abscess is a localized cavity filled with pus within the lung tissue itself. It typically develops from a bacterial infection that causes lung tissue necrosis, often due to aspiration or unresolved pneumonia.
The abscess forms as the body attempts to isolate and contain the infection, resulting in a fluid-filled cavity surrounded by inflamed lung tissue. Management usually requires prolonged antibiotic therapy and sometimes drainage if the abscess is large or not responding.
Summary of Key Differences
Empyema occurs outside the lung in the pleural space, whereas a lung abscess is inside the lung tissue. Empyema involves purulent pleural fluid; lung abscess involves necrotic lung tissue and a pus-filled cavity.
Empyema often needs thoracentesis or chest tube drainage, while lung abscesses primarily require antibiotics, with drainage less frequently necessary.
Note: The underlying causes differ slightly, and imaging studies such as CT scans help distinguish the two.
Etiology and Risk Factors
Empyema and lung abscess both result from infections but differ in their origins and contributing factors. Their causes involve various pathogens and conditions that impair lung or pleural defenses.
Common Causes of Empyema
Empyema typically arises from bacterial infections that spread into the pleural space. The most common source is pneumonia, especially caused by Streptococcus pneumoniae, Staphylococcus aureus, and Haemophilus influenzae.
Other causes include thoracic surgery, trauma to the chest wall, or esophageal rupture leading to contamination of the pleural space. Tuberculosis can also cause chronic empyema in endemic areas.
The infection progresses as pus accumulates between the lung and chest wall, often after inadequate treatment of a parapneumonic effusion or complicated pneumonia.
Predisposing Factors for Lung Abscess
Lung abscess forms when lung tissue becomes necrotic due to infection. Aspiration of oropharyngeal contents, particularly anaerobic bacteria like Bacteroides and Fusobacterium, is the leading cause.
Other factors include bronchial obstruction from tumors or foreign bodies, immunosuppression, and chronic lung diseases such as bronchiectasis.
Poor dental hygiene or alcoholism increases risk by facilitating aspiration. Patients with a history of seizures or altered consciousness are also more susceptible to aspiration and subsequent abscess formation.
Patient Demographics and Associations
Empyema occurs in all age groups but is more frequent in adults with comorbidities like diabetes, malignancy, or immunosuppression. Men have a slightly higher incidence.
Lung abscess tends to affect middle-aged adults with risk factors for aspiration such as alcohol use disorder or neurologic impairment. Chronic smokers and patients with underlying lung disease are also more prone.
Both conditions are linked to healthcare exposure, especially when invasive procedures or mechanical ventilation are involved, increasing the risk of secondary infections.
Pathophysiology
Empyema and lung abscess both result from infections involving the lung and pleural space but differ in their anatomical locations and progression mechanisms. Their pathophysiology involves distinct processes leading to pus accumulation either in the pleural cavity or within lung parenchyma.
Empyema Formation Process
Empyema develops when a bacterial infection extends from pneumonia or direct pleural contamination into the pleural space. Initially, a sterile exudative pleural effusion forms due to inflammation. With bacterial invasion, this fluid becomes purulent as neutrophils and bacteria accumulate.
The infection causes fibrin deposition, which leads to loculation and thickening of the pleura. This creates multiple compartments within the pleural space. Chronic empyema may result in a thick fibrothorax limiting lung expansion.
Common causative organisms include Staphylococcus aureus, Streptococcus pneumoniae, and anaerobes. The process involves a shift from simple effusion to complex, organized infection confined by pleural membranes.
Lung Abscess Development Mechanisms
Lung abscesses develop due to necrosis of lung tissue following bacterial infection. Aspiration of oropharyngeal contents introduces anaerobic bacteria into the lung parenchyma. The body’s immune response leads to localized tissue destruction and pus formation.
The abscess cavity forms with a necrotic center surrounded by an inflammatory capsule. Common organisms include anaerobes such as Bacteroides and Fusobacterium, and aerobic bacteria like Staphylococcus aureus.
Obstruction of bronchi or impaired drainage contributes to abscess formation by creating a favorable environment for bacterial growth. The process is mainly localized within the lung tissue, distinguishing it from empyema’s pleural involvement.
Clinical Presentation
Empyema and lung abscess share some respiratory symptoms but differ in onset, severity, and specific clinical signs. Careful assessment of symptoms can help distinguish between these two conditions early in their course.
Symptoms of Empyema
Empyema typically presents with fever, chills, and pleuritic chest pain localized to the affected side. Patients often report a persistent cough producing purulent or foul-smelling sputum.
Dyspnea is common, worsening as the fluid accumulates in the pleural space. Physical examination may reveal decreased breath sounds and dullness to percussion over the involved area.
Systemic signs such as malaise, night sweats, and weight loss occur, especially in prolonged or untreated cases. Symptoms usually develop over days to weeks following pneumonia or thoracic surgery.
Symptoms of Lung Abscess
Lung abscess often begins with a high-grade fever accompanied by a productive cough that yields thick, foul-smelling sputum or sometimes blood-tinged sputum. The cough is typically more persistent than in empyema.
Chest pain is usually less localized but may increase on inspiration. Patients may experience night sweats, fatigue, and weight loss, which can reflect the ongoing infection.
Breath sounds may be diminished, with possible crackles or bronchial breath sounds on auscultation. The onset tends to be more insidious, often developing after aspiration or pneumonia complications.
Diagnosis and Imaging
Accurate diagnosis of empyema and lung abscess relies heavily on imaging techniques combined with clinical findings. Each condition presents distinct features on imaging that help differentiate between the two.
Imaging Modalities
A chest X-ray is usually the first imaging test performed. It can identify fluid collections and changes in lung parenchyma, but has limitations in distinguishing empyema from lung abscess.
A computed tomography (CT) scan provides detailed images of the pleural space and lung tissue. It can detect loculated pleural fluid, thickened pleura, and cavities with air-fluid levels. CT is more sensitive and specific, especially for early or complex cases.
Ultrasound is valuable in identifying pleural fluid and guiding thoracentesis. It detects septations within pleural collections, aiding in the diagnosis of an empyema.
Diagnostic Criteria for Empyema
Empyema is diagnosed by evidence of infected pleural fluid. Imaging shows pleural fluid that is often loculated with thickened, enhancing pleural membranes on CT.
Key signs include a split pleura sign—a visible separation between the visceral and parietal pleura due to inflammation. The fluid typically appears purulent or turbid when sampled via thoracentesis.
Laboratory analysis of pleural fluid confirms diagnosis with low pH (<7.2), low glucose, elevated lactate dehydrogenase (LDH), and positive bacterial cultures. Combined imaging and fluid analysis confirm empyema.
Diagnostic Criteria for Lung Abscess
A lung abscess appears as a cavity with an air-fluid level within consolidated lung tissue on CT or X-ray. The cavity typically has thick, irregular walls. Unlike empyema, the fluid is within the lung parenchyma and not the pleural space. Surrounding lung tissue shows consolidation and inflammation.
Sputum culture, blood tests, and sometimes bronchoscopy help identify causative organisms. Imaging findings of a solitary or multiple thick-walled cavities with air-fluid levels strongly indicate a lung abscess.
Treatment Approaches
Effective management involves targeted antibiotic use, fluid evacuation, and in some cases, surgery. Treatment varies depending on the extent of the infection and the patient’s response.
Medical Management
Empyema and lung abscess both require antibiotic therapy tailored to the likely pathogens. Empiric treatment often covers anaerobes, aerobic bacteria, and sometimes methicillin-resistant Staphylococcus aureus (MRSA). Therapy typically lasts 3 to 6 weeks, with adjustments made based on clinical and radiographic improvement.
For lung abscess, oral or IV antibiotics targeting anaerobic bacteria and Streptococcus species are essential. Monitoring for resolution through imaging helps guide duration. Empyema patients may receive similar antibiotics, but often need more aggressive initial therapy due to pleural space infection.
Drainage Procedures
In empyema, drainage of purulent pleural fluid is critical. This is commonly done using chest tube thoracostomy under imaging guidance. Prompt fluid removal reduces bacterial load and alleviates symptoms.
Lung abscess drainage is less common but considered if the abscess is large, fails to respond to antibiotics, or risks rupture into the pleura. Percutaneous catheter drainage under CT guidance may be employed in selected cases to evacuate necrotic material.
Surgical Intervention
Surgery is reserved for complicated or persistent cases. In empyema, video-assisted thoracoscopic surgery (VATS) allows for decortication to remove fibrous peel and facilitate lung re-expansion. Open thoracotomy may be necessary if VATS fails.
For lung abscess, lobectomy or segmentectomy is rarely indicated but considered when medical and drainage treatments fail or malignancy cannot be excluded. Surgery carries a higher risk and is a last resort after less invasive methods are exhausted.
Complications and Prognosis
Empyema and lung abscess share risks tied to infection and tissue damage. The outcomes depend on prompt diagnosis, treatment response, and the patient’s overall health.
Potential Complications
Empyema can lead to chronic pleural thickening and trapped lung if untreated. It may cause bronchopleural fistulas, leading to persistent air leaks. Sepsis and multiorgan failure are risks associated with the spread of systemic infection.
Lung abscess complications include rupture into the pleural space, causing empyema or pneumothorax. Hemorrhage from erosion of blood vessels may occur. Persistent abscess or spread to the bloodstream can result in septicemia.
Note: Both conditions may require surgical drainage or resection if medical therapy fails. Delayed treatment increases the risk of long-term lung function impairment.
Prognostic Factors
Early intervention with antibiotics and drainage improves prognosis in both conditions. The size and location of the empyema or abscess influence recovery time. Comorbidities like diabetes, chronic lung disease, or immunosuppression worsen outcomes. Advanced age and delayed treatment correlate with higher morbidity and mortality.
Microbial etiology matters; infections with resistant or anaerobic bacteria complicate management. Radiologic resolution and clinical improvement within weeks indicate a better prognosis.
FAQs About an Empyema vs. a Lung Abscess
Are Empyema and Lung Abscesses the Same?
No, empyema and lung abscesses are not the same, though both involve infection and pus. An empyema is pus that collects in the pleural space, which is the cavity between the lung and chest wall.
In contrast, a lung abscess forms within the lung tissue itself as a pocket of pus. Their causes, symptoms, and treatments also differ. Empyema often requires drainage procedures, while lung abscesses are usually treated with long-term antibiotics.
What Is Another Name for Empyema?
Empyema is sometimes referred to as “pyothorax” or “purulent pleuritis.” Both terms highlight the presence of pus within the pleural cavity surrounding the lungs. While “empyema” is the most commonly used medical term, these alternatives emphasize the same condition: infection in the pleural space, typically following pneumonia, chest trauma, or surgery.
Note: Regardless of terminology, empyema requires medical evaluation and timely treatment to prevent complications such as lung restriction, sepsis, or chronic respiratory problems.
What Is the Difference Between Empyema and Effusion?
A pleural effusion refers to the buildup of excess fluid between the lungs and chest wall, which may be clear, bloody, or infected. Empyema is a type of pleural effusion specifically caused by infection, leading to pus in the pleural space.
While not all effusions are empyemas, all empyemas are considered complicated effusions. Effusions can result from heart failure, cancer, or liver disease, while empyema is almost always due to infection. Correct diagnosis is crucial for proper treatment.
Can You Have an Abscess Without Pus?
By definition, an abscess is a collection of pus that develops due to infection, so having a true abscess without pus is not possible. Pus is made of dead white blood cells, bacteria, and tissue debris, and its presence defines the condition.
However, early in the process of infection, inflammation may occur before significant pus forms, which can sometimes mimic an abscess. In such cases, imaging and medical evaluation help confirm whether it is a true abscess or another condition.
How Are Lung Abscess and Empyema Diagnosed?
Diagnosis involves a combination of clinical evaluation, imaging, and laboratory tests. A chest X-ray or CT scan is typically performed to identify whether the infection is localized inside the lung tissue (abscess) or in the pleural space (empyema).
Doctors may also use ultrasound to guide drainage in suspected empyema cases. Blood tests can reveal infection, and sputum cultures may identify the causative bacteria. In some cases, fluid samples from the pleural cavity are analyzed to confirm empyema.
If I Don’t Have Empyema, What Other Condition Might I Have?
If empyema is ruled out, other conditions that may mimic its symptoms include simple pleural effusion, pneumonia, or lung abscess. Pleural effusions can occur due to heart failure, cancer, or liver disease, and are not always infected.
Pneumonia may cause fever, cough, and chest pain, but it does not always spread to the pleural space. A lung abscess, meanwhile, forms within lung tissue rather than around it. Accurate diagnosis requires imaging studies and sometimes fluid analysis.
What Is the Difference Between Empyema and Parapneumonic Effusion?
A parapneumonic effusion is fluid in the pleural space that occurs as a complication of pneumonia. Not all parapneumonic effusions are infected; some may remain sterile. Empyema represents the more advanced stage of a parapneumonic effusion, in which the fluid becomes infected and turns into pus.
In other words, all empyemas begin as parapneumonic effusions, but not all parapneumonic effusions progress to empyema. Early detection and treatment of parapneumonic effusions can help prevent empyema from developing.
What Is the Difference Between Empyema and Pleural Effusion?
Pleural effusion is a general term for any buildup of fluid in the pleural space. This fluid can be watery (transudate), protein-rich (exudate), bloody, or purulent. Empyema is a specific type of pleural effusion where the fluid is purulent, meaning it contains pus from infection.
While pleural effusion can result from conditions like heart failure, kidney disease, or cancer, empyema nearly always results from infection. The distinction is important, as empyema requires drainage plus antibiotics.
What Is the Difference Between Pneumonia and Empyema?
Pneumonia is an infection of the lung tissue itself, leading to symptoms like cough, fever, chest pain, and shortness of breath. Empyema, however, is a complication that occurs when infection spreads from pneumonia into the pleural space, causing pus accumulation around the lungs.
Not every case of pneumonia leads to empyema; however, untreated or severe infections increase the risk. Pneumonia is typically treated with antibiotics, while empyema often requires drainage procedures in conjunction with medical therapy.
When to See a Doctor for Empyema or Lung Abscess?
You should see a doctor promptly if you experience a persistent cough, fever, chest pain, difficulty breathing, or coughing up foul-smelling sputum. These can be warning signs of lung abscess or empyema, which require timely treatment.
Delaying medical care can lead to complications such as sepsis, chronic infection, or permanent lung damage. Anyone with pneumonia symptoms that worsen or fail to improve with antibiotics should also seek urgent medical evaluation to rule out empyema or abscess formation.
Final Thoughts
Although empyema and lung abscess share similarities in that both involve infection and pus formation, their key differences lie in location, underlying causes, and treatment approaches.
An empyema affects the pleural space and often requires surgical or procedural drainage, while a lung abscess forms within lung tissue and typically responds to prolonged antibiotic therapy.
Recognizing these distinctions is crucial for clinicians to choose the most effective management strategy. For patients, understanding these conditions can highlight the importance of seeking medical attention early when symptoms such as persistent cough, chest pain, or fever arise. With timely diagnosis and treatment, outcomes for both empyema and lung abscess can be significantly improved.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Iguina MM, Sharma S, Danckers M. Thoracic Empyema. [Updated 2024 Dec 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.
- Sabbula BR, Rammohan G, Sharma S, et al. Lung Abscess. [Updated 2024 Jun 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.