The inspiratory-to-expiratory ratio, often abbreviated as I:E ratio, is a fundamental concept in respiratory physiology and mechanical ventilation. It describes the proportion of time spent inhaling (inspiration) compared to the time spent exhaling (expiration) during each breathing cycle.
While it may seem like a simple measurement, the I:E ratio has significant implications for patient comfort, gas exchange, and overall respiratory mechanics, making it an essential concept for respiratory therapists and other healthcare professionals.
Take our free course to master the basics of mechanical ventilation with clear explanations and helpful practice questions.
What is the I:E Ratio?
The inspiratory-to-expiratory ratio (I:E ratio) is a measure of the relationship between the time spent inhaling and exhaling during a single respiratory cycle. In a healthy adult at rest, the I:E ratio is typically about 1:2, meaning exhalation lasts twice as long as inhalation.
This natural balance allows for effective oxygen intake while giving the lungs enough time to expel carbon dioxide. The ratio can shift depending on activity, lung health, or when mechanical ventilation is used.
For instance, patients with restrictive lung disease may require a prolonged inspiratory phase to improve oxygenation, while those with obstructive disease often need longer exhalation times to prevent air trapping. Understanding and adjusting the I:E ratio is critical for respiratory therapists to optimize breathing mechanics and patient care.
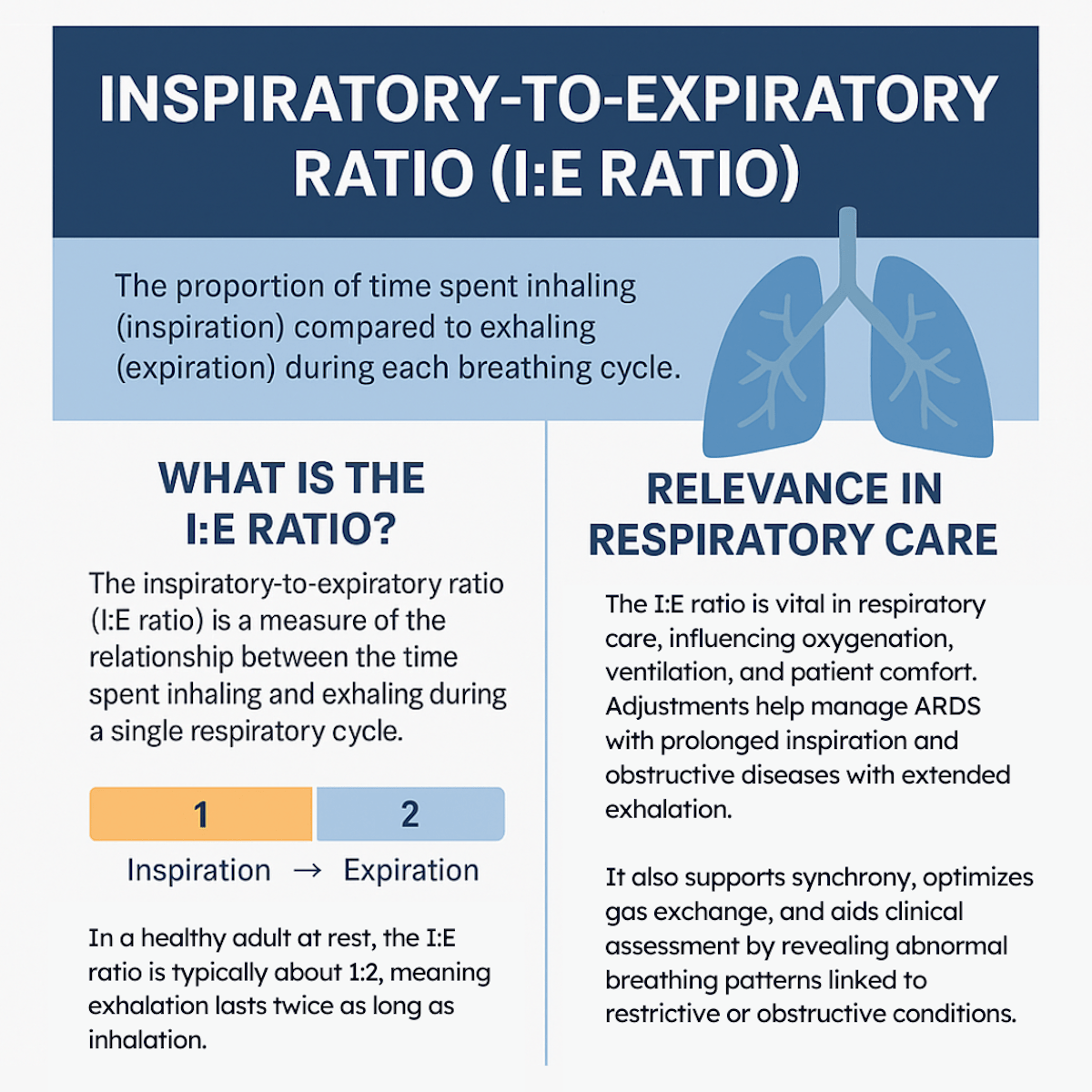
Relevance in Respiratory Care
1. Mechanical Ventilation
In mechanically ventilated patients, controlling the I:E ratio is crucial. Adjusting this setting can optimize oxygenation and ventilation:
- Prolonged inspiration (inverse ratio ventilation, e.g., 2:1) can improve oxygenation in patients with acute respiratory distress syndrome (ARDS) by increasing mean airway pressure and alveolar recruitment.
- Prolonged expiration (e.g., 1:3 or greater) is often necessary for patients with obstructive diseases such as COPD or asthma to prevent dynamic hyperinflation and auto-PEEP.
2. Patient Comfort and Synchrony
Maintaining an appropriate I:E ratio ensures that mechanical breaths feel natural to the patient. Mismatches in timing may cause patient–ventilator asynchrony, discomfort, and increased work of breathing.
3. Gas Exchange Efficiency
The I:E ratio affects mean airway pressure and time available for alveolar ventilation. Proper adjustment can improve oxygen delivery, carbon dioxide removal, and overall respiratory efficiency.
4. Clinical Assessment
Respiratory therapists use the I:E ratio when evaluating patients’ breathing patterns. Observing shortened expiratory times may indicate conditions such as asthma exacerbations, while abnormally prolonged inspiratory times may suggest restrictive lung disease or ventilator setting errors.
Why It Matters to Respiratory Therapists
Respiratory therapists are responsible for setting, monitoring, and adjusting ventilator parameters tailored to each patient’s condition. Understanding the impact of the I:E ratio allows therapists to:
- Recognize abnormal breathing patterns in spontaneous breathing patients.
- Tailor ventilator settings to improve patient outcomes.
- Prevent complications such as barotrauma, volutrauma, or auto-PEEP.
- Educate patients and families about breathing mechanics and ventilatory support.
Note: Mastering the I:E ratio gives respiratory therapists the ability to fine-tune care and respond quickly to a patient’s changing needs. By applying this knowledge, RTs not only enhance patient safety and comfort but also strengthen their role as vital members of the healthcare team.
I:E Ratio in Mechanical Ventilation
The inspiratory-to-expiratory (I:E) ratio plays a central role in managing patients on mechanical ventilation, as it directly influences gas exchange, airway pressures, and overall patient safety. While a normal spontaneous breathing pattern maintains an approximate ratio of 1:2, this balance can be adjusted on the ventilator to meet specific clinical demands.
In restrictive lung conditions such as acute respiratory distress syndrome (ARDS), clinicians may employ an inverse I:E ratio (e.g., 2:1 or 3:1). By prolonging the inspiratory phase, mean airway pressure increases, which can improve oxygenation and enhance alveolar recruitment. However, this strategy must be carefully monitored to avoid hemodynamic compromise due to higher intrathoracic pressures.
In contrast, patients with obstructive lung diseases like chronic obstructive pulmonary disease (COPD) or asthma benefit from extended exhalation times. Lowering the I:E ratio (e.g., 1:3, 1:4, or even longer) allows sufficient time for air to exit the lungs, preventing air trapping, dynamic hyperinflation, and auto-PEEP.
Ultimately, the I:E ratio must be individualized, taking into account lung mechanics, disease state, and therapeutic goals. Meticulous adjustment by respiratory therapists ensures optimal ventilation while reducing the risks of barotrauma, volutrauma, and impaired gas exchange.
I:E Ratio Practice Questions
1. What is the normal inspiratory-to-expiratory (I:E) ratio in a healthy adult?
1:2
2. What is the I:E ratio used for in mechanical ventilation?
To calculate and set the appropriate timing between inspiration and expiration.
3. The I:E ratio and inspiratory flow together determine what key aspect of ventilation?
They determine the timing and efficiency of gas exchange during mechanical ventilation.
4. What is the term for the total time required to complete one full breath cycle (inspiration + expiration)?
Total Cycle Time (TCT)
5. What formula represents the relationship between inspiratory time (TI), expiratory time (TE), and the total cycle time?
TCT = TI + TE
6. If the inspiratory time (TI) is 2 seconds and the expiratory time (TE) is 4 seconds, what is the total cycle time (TCT)?
6 seconds
7. If the inspiratory time (TI) is 1 second and the total cycle time (TCT) is 4 seconds, what is the expiratory time (TE)?
3 seconds
8. What formula is used to calculate the respiratory rate (f) from the total cycle time (TCT)?
f = 60 ÷ TCT
9. If the total cycle time (TCT) is 6 seconds, what is the respiratory rate (f)?
10 breaths per minute (bpm)
10. If TI is 1 second and TE is 3 seconds, what is the total cycle time?
4 seconds
11. If TE is 3 seconds and the TCT is 3.5 seconds, what is the inspiratory time (TI)?
0.5 seconds
12. Given a respiratory rate of 30 bpm, what is the total cycle time (TCT)?
2 seconds
13. What does the abbreviation “TI” stand for in respiratory calculations?
Inspiratory Time – the duration of inhalation
14. What does the abbreviation “TE” stand for in respiratory calculations?
Expiratory Time – the duration of exhalation
15. True or False: The I:E ratio is especially important when managing patients on mechanical ventilation.
True
16. Why is a longer expiratory time needed in patients with obstructive diseases like asthma or COPD?
To allow complete exhalation and prevent air trapping
17. True or False: Expiratory time is usually shorter than inspiratory time in normal breathing.
False – Exhalation typically lasts longer
18. If insufficient time is given for exhalation during mechanical ventilation, what adverse effect can occur?
Increased intrathoracic pressure leading to air trapping or auto-PEEP
19. If the inspiratory time (TI) is 1.25 seconds and the expiratory time (TE) is 4.75 seconds, what is the I:E ratio?
1:3.8
20. What does the formula Vt = V × TI represent in respiratory mechanics?
The relationship between tidal volume, inspiratory flow, and inspiratory time
21. In the formula Vt = V × TI, what does each variable stand for?
Vt = Tidal Volume, V = Flow (in L/sec), TI = Inspiratory Time
22. What must be done to the units of Vt and flow before solving the equation Vt = V × TI?
Convert Vt to liters and flow from L/min to L/sec
23. If the tidal volume is 700 mL and the flow is 40 L/min, what is the inspiratory time (TI)?
1.05 seconds
24. If a ventilator is set to an I:E ratio of 1:3 with a respiratory rate of 15, what does that mean for the timing of each breath?
Each breath lasts 4 seconds with 1 second of inspiration and 3 seconds of expiration
25. Why is the I:E ratio often adjusted in patients with restrictive lung disease like ARDS?
To prolong inspiration and improve alveolar recruitment and oxygenation
26. During assist-control (A/C) mechanical ventilation, what two variables most directly affect the I:E ratio?
Inspiratory time (I-time) and expiratory time (E-time)
27. In volume-control A/C ventilation, how is inspiratory time calculated?
I-time = Volume (L) ÷ Flow (L/sec)
28. In pressure-control A/C ventilation, how is the inspiratory time typically set?
It is directly set by the clinician
29. How is expiratory time (E-time) determined in either A/C mode?
E-time = Total cycle time – Inspiratory time
30. Why is it often necessary to decrease the I:E ratio in patients with severe obstructive diseases like COPD?
To allow longer exhalation and avoid air trapping or auto-PEEP
31. What are typical I:E ratios seen in spontaneously breathing patients with obstructive lung disease?
1:4 or 1:5
32. What complication can occur if these patients do not have sufficient expiratory time during mechanical ventilation?
Auto-PEEP (air trapping)
33. If a patient has auto-PEEP and an I:E ratio of 1:2, what is the first adjustment you should make?
Decrease the I:E ratio to allow more time for exhalation
34. How can you decrease the I:E ratio on a ventilator?
By increasing expiratory time and/or decreasing inspiratory time
35. What are two methods to increase E-time in assist-control volume control ventilation?
Decrease respiratory rate and/or switch to low-rate SIMV
36. What are two methods to decrease I-time in volume control ventilation?
Increase inspiratory flow and/or decrease tidal volume
37. What is a method to decrease I-time in pressure control ventilation?
Decrease the set inspiratory time or %I-time
38. If a patient is developing auto-PEEP due to a high ventilator rate and short E-time, what is one effective adjustment?
Lower the set respiratory rate
39. What formula is used to calculate total cycle time (TCT) based on respiratory rate?
TCT = 60 seconds ÷ respiratory rate (f)
40. What is the formula to convert flow from L/min to L/sec?
Flow (L/sec) = Flow (L/min) ÷ 60
41. How long would it take to deliver a tidal volume of 1000 mL at a flow rate of 90 L/min?
0.66 seconds
42. What is the inspiratory time for a flow of 45 L/min and tidal volume of 900 mL?
1.2 seconds
43. If Vt = 900 mL, flow = 45 L/min, and rate = 20 bpm, what is the expiratory time?
1.8 seconds
44. Given a Vt of 900 mL, flow of 45 L/min, and rate of 12 bpm, what is the I:E ratio?
1:3.17
45. In general, how does increasing flow rate affect inspiratory time in volume-controlled ventilation?
Increases in flow cause a decrease in inspiratory time
46. How does increasing tidal volume affect inspiratory time in volume-controlled ventilation?
Increasing Vt increases inspiratory time
47. If you increase respiratory rate but do not change flow or Vt in volume control, what happens to expiratory time?
Expiratory time decreases
48. If you increase respiratory rate with fixed inspiratory time, what happens to the I:E ratio?
The I:E ratio increases (becomes more balanced), and the numbers contract
49. If a physician increases the rate but wants to keep the same I:E ratio and tidal volume, what adjustment must be made?
You must increase the inspiratory flow
50. In which mode of ventilation does changing the flow rate have a direct effect on inspiratory time?
Volume-controlled ventilation
51. Why might switching to low-rate SIMV help a patient with auto-PEEP or ventilator asynchrony?
It allows for longer expiratory time and better patient-ventilator synchrony
52. What happens to TCT when the respiratory rate is increased from 12 to 20 bpm?
TCT decreases from 5 seconds to 3 seconds
53. If inspiratory time is fixed at 1 second and the respiratory rate increases, what must happen to expiratory time?
Expiratory time must decrease
54. What is the primary goal of adjusting I:E ratio in patients with asthma or COPD on mechanical ventilation?
To allow sufficient time for complete exhalation
55. In volume control ventilation, what two factors determine inspiratory time?
Tidal volume and inspiratory flow rate
56. A 75 kg, 5’10” male patient is ventilated with a tidal volume of 600 mL, a flow of 45 L/min, and a respiratory rate of 15. If inspiratory time (Tinsp) is 0.8 seconds, what is his expiratory time (Texp)?
3.2 seconds
57. If a patient’s inspiratory time is 0.8 seconds and expiratory time is 3.2 seconds, what is the I:E ratio?
1:4
58. A patient has a tidal volume of 750 mL, a flow of 45 L/min, and a respiratory rate of 15 breaths per minute. What are the calculated time parameters?
Ttotal = 4.0 sec, Tinsp = 1.0 sec, Texp = 3.0 sec, I:E ratio = 1:3
59. If you must keep the respiratory rate the same but increase the tidal volume, how can you maintain the same I:E ratio?
Increase the inspiratory flow
60. What happens to inspiratory time when changing from a square waveform to a decelerating or sinusoidal flow pattern?
Inspiratory time increases
61. Does increasing inspiratory flow generally result in a decrease in inspiratory time?
Yes
62. If you want to lengthen inspiratory time, what should you do to the inspiratory flow rate?
Decrease the flow
63. What happens to inspiratory time if tidal volume is increased while flow remains the same?
Inspiratory time increases
64. What adjustment to flow is needed to decrease inspiratory time?
Increase the flow
65. If the respiratory rate is increased, what happens to expiratory time, and how might you compensate using Tinsp?
Expiratory time decreases, and you may need to decrease Tinsp to allow more time for exhalation
66. Do large tidal volumes generally require higher inspiratory flow?
Yes
67. Do high respiratory rates generally require higher inspiratory flow?
Yes
68. Why are lower inspiratory flows typically used in patients with restrictive lung disease?
To prolong inspiratory time and increase mean airway pressure
69. To maintain the same I:E ratio when reducing tidal volume and keeping the respiratory rate the same, what must be done to flow?
Reduce the flow
70. If the respiratory rate is increased and the tidal volume remains the same, what must be done to flow to maintain the same I:E ratio?
Increase the flow
71. When changing the flow waveform from square to decelerating, what happens to inspiratory time?
Inspiratory time increases
72. In the equation A = B / C, if B increases, what happens to A?
A increases
73. In the equation A = B / C, if C increases, what happens to A?
A decreases
74. In the equation A = B / C, how can you increase the value of A?
Increase B or decrease C
75. In the equation A = B / C, how can you decrease the value of A?
Decrease B or increase C
76. According to the formula FLOW = VOLUME / TIME, what is the equation for inspiratory time?
Tinsp = Volume / Flow
77. What is the relationship between inspiratory time and flow?
They are inversely related
78. If flow decreases and volume remains constant, what happens to inspiratory time?
Inspiratory time increases
79. If tidal volume decreases and flow remains constant, what happens to inspiratory time?
Inspiratory time decreases
80. What is the relationship between tidal volume and inspiratory time when flow is constant?
They are directly related
81. What is the most effective initial adjustment to reduce auto-PEEP in a volume-controlled patient with obstructive lung disease?
Increase the inspiratory flow to shorten inspiratory time and lengthen expiratory time
82. A ventilator is set to a respiratory rate of 10 breaths/min. What is the total cycle time per breath?
6 seconds (Ttotal = 60 / 10)
83. A patient has an I-time of 1.5 seconds and a total cycle time of 5 seconds. What is the expiratory time and I:E ratio?
Texp = 3.5 seconds, I:E = 1:2.33
84. In volume-controlled ventilation, what happens to inspiratory time if the inspiratory flow is halved?
Inspiratory time doubles
85. What ventilator adjustment is most appropriate if a patient exhibits signs of air trapping and auto-PEEP?
Decrease the respiratory rate to allow for a longer expiratory phase
86. How does switching from VC to PC ventilation affect the control of inspiratory time?
In PC, inspiratory time is directly set by the clinician
87. Which ventilator setting should be increased to decrease inspiratory time without affecting tidal volume?
Increase inspiratory flow
88. What does an I:E ratio of 1:1 indicate about the time allocated for inspiration and expiration?
Inspiratory and expiratory times are equal
89. What happens to the I:E ratio if tidal volume is increased but flow remains constant?
The I:E ratio increases (shorter expiratory time)
90. What is a potential consequence of insufficient expiratory time in a patient with COPD?
Development of auto-PEEP and air trapping
91. How can you calculate I:E ratio from known inspiratory and expiratory times?
Divide each by the inspiratory time (e.g., I:E = 1 : Texp/Tinsp)
92. What is the result of setting a very low inspiratory flow rate in volume-controlled ventilation?
Prolonged inspiratory time and reduced expiratory time
93. In pressure control mode, what factors influence the I:E ratio?
Set inspiratory time and respiratory rate
94. A patient’s total cycle time is 5 seconds with an I-time of 1.25 seconds. What is the I:E ratio?
1:3 (Texp = 3.75 sec → 3.75 / 1.25 = 3)
95. Why is a decelerating flow pattern often used in pressure-controlled ventilation?
It improves gas distribution and patient comfort, but increases inspiratory time
96. What is the clinical implication of using an I:E ratio of 2:1 in ARDS patients?
It may improve oxygenation by increasing mean airway pressure
97. What is the typical I:E ratio used for patients with normal lungs?
1:2
98. How does increasing the respiratory rate without changing flow or tidal volume affect I:E ratio?
It shortens expiratory time and increases the I:E ratio
99. When would a clinician choose an I:E ratio of 1:4?
In patients with obstructive lung disease to allow for full exhalation
100. How does decreasing tidal volume affect the I:E ratio if flow and rate remain constant?
Inspiratory time decreases, lengthening expiratory time and lowering the I:E ratio
Final Thoughts
The inspiratory-to-expiratory ratio (I:E ratio) is more than just a number—it reflects the balance between inhalation and exhalation that sustains life. For respiratory therapists, mastering this concept is critical for optimizing mechanical ventilation, ensuring patient comfort, and promoting effective gas exchange.
Whether in the ICU or during bedside assessment, the I:E ratio remains a cornerstone of respiratory care, guiding clinical decisions that can profoundly impact patient outcomes.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Boros SJ. Variations in inspiratory:expiratory ratio and airway pressure wave form during mechanical ventilation: the significance of mean airway pressure. J Pediatr. 1979.