Lung cancer is one of the most serious and life-threatening diseases affecting the respiratory system. It begins when abnormal cells grow uncontrollably in the lungs, often forming tumors that interfere with normal breathing and gas exchange.
Because the lungs are essential for delivering oxygen to the body and removing carbon dioxide, any disruption can have a profound impact on overall health.
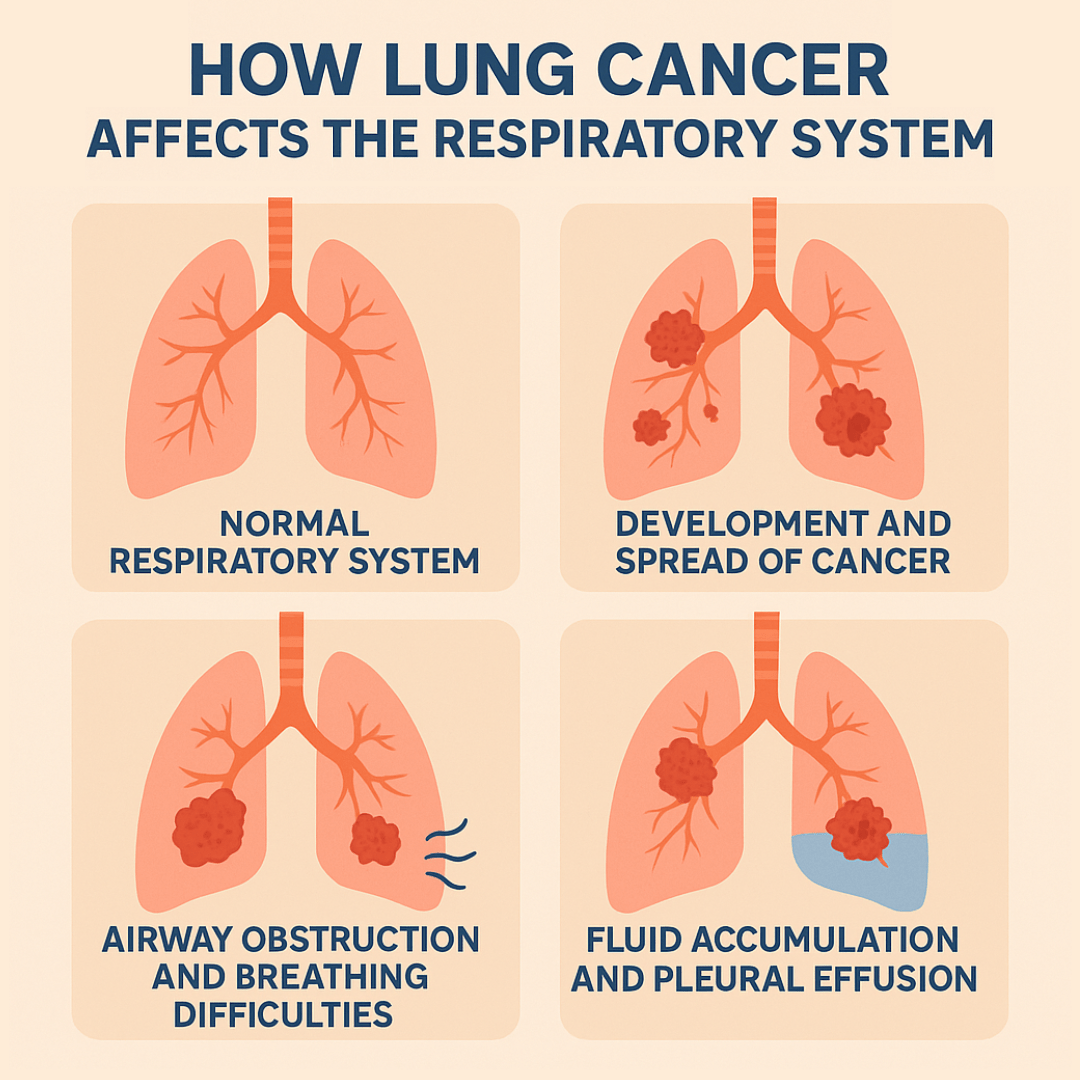
This article examines the impact of lung cancer on the respiratory system, including its effects on obstructing airflow, damaging lung tissue, and causing breathing difficulties and other complications.
Download our free guide that has over 100+ of the best tips for healthy lungs.
How Does Lung Cancer Affect the Respiratory System?
Lung cancer significantly impacts the respiratory system by interfering with the normal function of the lungs. Tumors can obstruct airways, making it more difficult to breathe and leading to symptoms such as coughing, wheezing, and shortness of breath.
As the cancer grows, it may reduce lung capacity, limit oxygen exchange, and cause chest pain. Some tumors also trigger fluid buildup (pleural effusion) between the lungs and chest wall, further restricting breathing. Additionally, cancer cells can damage surrounding lung tissue and spread (metastasize) to other parts of the body, worsening respiratory symptoms.
In advanced cases, lung cancer can lead to respiratory failure, which occurs when the lungs can no longer provide adequate oxygen or remove carbon dioxide effectively.
The Normal Respiratory System
Before examining how lung cancer affects respiratory function, it’s essential to understand how healthy lungs operate. The respiratory system comprises the airways, lungs, and respiratory muscles, which work together to facilitate gas exchange. Air enters through the nose or mouth, travels down the trachea, and branches into progressively smaller airways called bronchi and bronchioles, ultimately reaching the tiny air sacs known as alveoli.
The alveoli are where the critical process of gas exchange occurs. Oxygen from inhaled air passes through the thin alveolar walls into the bloodstream, while carbon dioxide moves from the blood into the alveoli to be exhaled.
Note: This process requires healthy lung tissue, clear airways, and adequate blood flow to function efficiently.
How Lung Cancer Develops and Spreads
Lung cancer typically begins when cells in the lung tissue undergo genetic mutations that cause them to grow and divide uncontrollably. These cancerous cells can originate in different parts of the lung, including the bronchi, bronchioles, or alveoli.
The two main types of lung cancer are non-small cell lung cancer, which accounts for approximately 85% of cases, and small cell lung cancer, which tends to grow and spread more rapidly.
As cancer cells multiply, they form tumors that can grow in size and spread to nearby tissues. This process, known as metastasis, can affect lymph nodes, other parts of the lung, and ultimately, distant organs. The location, size, and spread of these tumors directly impact the severity of the respiratory system’s involvement.
Airway Obstruction and Breathing Difficulties
One of the most immediate ways lung cancer affects the respiratory system is through airway obstruction. As tumors grow within or near the bronchi and bronchioles, they can partially or completely block these airways. This obstruction restricts airflow, making it increasingly difficult for air to reach the alveoli where gas exchange occurs.
The consequences of airway obstruction are progressive and debilitating. Patients may initially experience mild shortness of breath during physical activity, but as the obstruction worsens, breathing difficulties can occur even at rest. The body’s natural response to reduced oxygen levels includes an increased breathing rate and effort, which can lead to fatigue and further respiratory distress.
When airways become significantly blocked, sections of the lung may collapse, a condition called atelectasis. This collapse reduces the overall lung capacity, forcing the remaining healthy lung tissue to work harder to maintain adequate oxygen levels. The resulting strain on the respiratory system can lead to chronic fatigue and reduced exercise tolerance.
Impaired Gas Exchange
Lung cancer significantly disrupts the delicate process of gas exchange that occurs in the alveoli. Tumors can directly damage alveolar tissue, reducing the surface area available for oxygen and carbon dioxide exchange. Additionally, cancer cells can thicken the walls between alveoli and blood vessels, creating a barrier that reduces the efficiency of gas transfer.
The impact on gas exchange extends beyond the immediate tumor location. Cancer-related inflammation can affect surrounding healthy lung tissue, further compromising respiratory function. As the disease progresses, larger portions of the lung become unable to participate effectively in oxygenation, leading to hypoxemia —a condition in which blood oxygen levels fall below normal ranges.
Poor gas exchange also affects the removal of carbon dioxide from the body. When the lungs cannot efficiently eliminate carbon dioxide, it can accumulate in the bloodstream, leading to hypercapnia. This condition can cause symptoms including confusion, drowsiness, and, in severe cases, respiratory failure.
Fluid Accumulation and Pleural Effusion
Lung cancer frequently causes fluid to accumulate in various parts of the respiratory system. One of the most common complications is pleural effusion, where fluid builds up in the space between the lungs and the chest wall. This fluid accumulation can result from cancer cells directly affecting the pleura, the thin membrane surrounding the lungs, or from blocked lymphatic drainage.
Pleural effusion creates significant respiratory challenges by compressing the lungs and reducing their ability to expand fully during breathing. Patients with this condition often experience severe shortness of breath, chest pain, and a feeling of heaviness in the chest. The accumulated fluid essentially occupies space that should be available for lung expansion, forcing the respiratory system to work with reduced capacity.
The presence of pleural effusion also indicates that the cancer may be spreading beyond the original tumor site, suggesting a more advanced stage of disease. Treatment often requires drainage of the fluid to provide temporary relief, but the underlying cancer must be addressed to prevent recurrence.
Respiratory Muscle Dysfunction
Advanced lung cancer can affect the muscles responsible for breathing, particularly the diaphragm and intercostal muscles between the ribs. Tumors that grow near or invade these muscles can cause weakness or paralysis, severely compromising the mechanical aspects of breathing.
The diaphragm, the primary muscle responsible for breathing, can be affected when cancer spreads to the phrenic nerve, which controls its movement. Diaphragmatic dysfunction forces other respiratory muscles to compensate, leading to inefficient breathing patterns and increased work of breathing. This compensation mechanism is not sustainable long-term and contributes to progressive respiratory failure.
When intercostal muscles are affected, the chest wall’s ability to expand and contract during breathing becomes compromised. This restriction limits lung expansion and reduces the volume of air that can be inhaled with each breath, further diminishing respiratory efficiency.
Inflammation and Infection Complications
Lung cancer triggers chronic inflammation throughout the respiratory system, which compounds the direct effects of tumor growth. This inflammation can cause swelling in the airways, increased mucus production, and reduced ciliary function, which normally helps clear debris and pathogens from the lungs.
The combination of impaired immune function and structural changes in the lungs makes cancer patients particularly susceptible to respiratory infections. Pneumonia and other lung infections are common complications that can significantly worsen respiratory symptoms and overall prognosis. These infections can cause additional inflammation, further compromising already limited lung function.
Chronic inflammation also contributes to the development of chronic obstructive pulmonary disease (COPD)-like symptoms in some lung cancer patients. This overlap of conditions creates a complex clinical picture where multiple factors simultaneously impair respiratory function.
Systemic Effects on Respiratory Function
The impact of lung cancer on the respiratory system extends beyond local effects to include systemic changes that affect breathing and oxygenation. Cancer cachexia, a syndrome characterized by weight loss and muscle wasting, can weaken respiratory muscles and reduce overall breathing capacity.
Anemia, common in cancer patients, reduces the blood’s oxygen-carrying capacity, effectively diminishing the efficiency of gas exchange even when lung function is relatively preserved. This creates a situation where the respiratory system must work harder to deliver adequate oxygen to the body tissues.
The body’s response to chronic hypoxemia includes increased production of red blood cells, which can make blood more viscous and harder to pump, placing additional strain on both the cardiovascular and respiratory systems. This interconnected stress response demonstrates how lung cancer affects not just local respiratory function but the entire oxygen delivery system.
Progressive Respiratory Failure
As lung cancer advances, the cumulative effects on respiratory function can lead to progressive respiratory failure. This condition occurs when the lungs can no longer maintain adequate gas exchange to meet the body’s metabolic needs. The progression typically follows a predictable pattern, beginning with exercise intolerance and advancing to breathing difficulties at rest.
Early stages of respiratory compromise may be compensated by increased breathing effort and heart rate, but as the disease progresses, these compensatory mechanisms become insufficient. The development of cor pulmonale, a condition where the right side of the heart becomes enlarged and strained due to lung disease, represents a serious complication that can accelerate the decline in respiratory function.
Terminal respiratory failure in lung cancer patients often involves a combination of factors, including extensive tumor burden, fluid accumulation, infection, and exhaustion of respiratory muscles. Understanding this progression helps healthcare providers and families prepare for and manage end-stage respiratory symptoms.
Treatment Implications and Respiratory Recovery
The impact of lung cancer on the respiratory system has a significant influence on treatment decisions and outcomes. Surgical resection of lung tumors, while potentially curative, further reduces lung capacity and requires careful assessment of remaining respiratory function. Patients must have adequate pulmonary reserves to survive surgery and maintain a reasonable quality of life afterward.
Radiation therapy and chemotherapy can also impact respiratory function, sometimes leading to inflammation and scarring in healthy lung tissue. These treatment-related effects must be weighed against the potential benefits of controlling cancer growth. Modern targeted therapies and immunotherapies offer new hope for managing lung cancer while potentially causing fewer respiratory side effects.
Pulmonary rehabilitation programs play a crucial role in maintaining and improving respiratory function in patients with lung cancer. These programs focus on breathing exercises, physical conditioning, and education about managing respiratory symptoms. Even patients with advanced disease can benefit from interventions designed to optimize their remaining lung function.
FAQs About How Lung Cancer Affects the Respiratory System
What Damage Does Lung Cancer Do to the Respiratory System?
Lung cancer can obstruct airways, destroy healthy lung tissue, and limit the lungs’ ability to exchange oxygen and carbon dioxide. Tumors may block the bronchial tubes, leading to symptoms such as wheezing, coughing, or infections like pneumonia.
As cancer progresses, it reduces lung capacity and elasticity, making breathing difficult. Some cases also involve fluid buildup around the lungs (pleural effusion), which further compresses the lungs.
Note: These effects severely impair respiratory function and can lead to respiratory failure if not treated.
What Body Systems Are Impacted by Lung Cancer?
While lung cancer primarily affects the respiratory system, it can also impact several other body systems. The circulatory system may be involved if cancer cells enter the bloodstream and spread (metastasize) to distant organs like the liver, brain, or bones.
The lymphatic system is commonly affected, as cancer often spreads to lymph nodes. Additionally, the skeletal, nervous, and digestive systems may be affected, depending on the location of metastases and the overall progression of the disease.
Can Lung Cancer Cause Respiratory Distress?
Yes, lung cancer can lead to respiratory distress, especially in advanced stages. Tumors may obstruct major airways, reduce lung function, and cause inflammation or infection. Fluid buildup in the lungs or around the chest (pleural effusion) can also impair breathing.
Patients may experience rapid breathing, shortness of breath, and low oxygen levels. In severe cases, respiratory distress can become life-threatening and may require emergency intervention such as supplemental oxygen or mechanical ventilation.
How Long Can You Have Lung Cancer Without Knowing?
Lung cancer can develop silently for months or even years without noticeable symptoms. Early-stage lung cancer often goes undetected because it may not cause pain or obvious changes. Many cases are only found incidentally during imaging for unrelated issues.
By the time symptoms like coughing, chest pain, or weight loss appear, the cancer may already be advanced. This silent progression makes routine screening important, especially for individuals at high risk due to smoking or other factors.
What Are the First Signs of Lung Cancer?
The first signs of lung cancer are often subtle and easily mistaken for less serious conditions. Common early symptoms include a persistent cough that doesn’t go away, coughing up blood or rust-colored sputum, shortness of breath, chest pain that worsens with deep breathing or coughing, and a history of frequent respiratory infections.
Some people may also experience hoarseness, fatigue, or unexplained weight loss. Because these symptoms can mimic other illnesses, they’re often overlooked until the disease progresses.
What Causes Shortness of Breath With Lung Cancer?
Several factors can cause shortness of breath with lung cancer. Tumors may block airways, limiting airflow and causing wheezing or shortness of breath. Cancer can also destroy healthy lung tissue, reducing lung capacity.
In some cases, the disease leads to pleural effusion—fluid buildup between the lungs and chest wall, which restricts lung expansion. Additionally, lung cancer can lead to anemia or spread to other organs, both of which can contribute to a feeling of breathlessness, especially during physical activity.
Final Thoughts
Lung cancer profoundly affects the respiratory system through multiple mechanisms that progressively impair the lungs’ ability to oxygenate blood and remove carbon dioxide. From direct tumor growth that obstructs airways to systemic effects that compromise oxygen delivery, the disease creates a complex web of respiratory challenges that require comprehensive management.
Understanding these effects is crucial for early recognition of symptoms, informed treatment planning, and supportive care that can enhance the quality of life for patients and their families. While lung cancer remains a serious threat to respiratory health, advances in treatment and supportive care continue to offer hope for better outcomes and improved respiratory function even in the face of this challenging disease.
The respiratory system’s remarkable complexity becomes most apparent when examining how lung cancer disrupts its normal function. This understanding underscores the importance of lung cancer prevention, early detection, and comprehensive treatment approaches that address both the cancer itself and its effects on respiratory health.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Siddiqui F, Vaqar S, Siddiqui AH. Lung Cancer. [Updated 2023 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.
- Sarna L, Evangelista L, Tashkin D, Padilla G, Holmes C, Brecht ML, Grannis F. Impact of respiratory symptoms and pulmonary function on quality of life of long-term survivors of non-small cell lung cancer. Chest. 2004.


