A thorough assessment helps respiratory therapists understand a patient’s current physiological status, identify underlying problems, and anticipate clinical trends. It guides therapy selection, prioritizes interventions, and strengthens communication across the healthcare team.
This article provides a practical, clinically focused approach to patient assessment in respiratory care, emphasizing organization, reasoning, and real-world application.
What Is a Patient Assessment?
A patient assessment is a structured process used to gather, analyze, and interpret information about a patient’s health status. It combines both subjective data (what the patient reports) and objective data (what the clinician observes or measures) to form a complete clinical picture.
In respiratory care, patient assessment focuses heavily on cardiopulmonary function but must always consider the patient as a whole. Respiratory problems rarely exist in isolation. Cardiac disease, neurological impairment, infection, metabolic imbalance, and even anxiety can significantly affect breathing and oxygenation.
A thorough assessment answers several critical questions:
- How is the patient breathing right now?
- Is gas exchange adequate?
- Are current therapies effective?
- Is the patient improving, stable, or deteriorating?
- What problems need immediate attention?
Note: Assessment is not a one-time event. It is a continuous process that begins before you enter the patient’s room and continues throughout the course of care.
Why Patient Assessment Matters in Respiratory Care
Patient assessment is the foundation of safe and effective respiratory therapy practice. Every treatment decision, from oxygen delivery to ventilator management, should be based on assessment findings rather than routine or habit.
Some of the key purposes of patient assessment include:
Establishing a Baseline
The initial assessment provides a reference point. Without a baseline, it is impossible to determine whether a patient is improving or worsening. Baseline findings allow future assessments to be compared objectively.
Identifying Abnormalities Early
Changes in respiratory rate, work of breathing, mental status, or breath sounds often precede major deterioration. Early detection allows for earlier intervention and prevents escalation of illness.
Guiding Clinical Decision-Making
Assessment findings determine whether therapy should be initiated, adjusted, escalated, or discontinued. They help tailor interventions to the patient’s specific needs.
Monitoring Response to Therapy
A treatment is only effective if it produces measurable improvement. Assessment confirms whether interventions are working and whether modifications are required.
Ensuring Patient Safety
Assessment helps identify risks such as airway compromise, hypoxemia, hypercapnia, fatigue, or impending respiratory failure. Recognizing these risks protects patients from harm.
Supporting Team Communication
Clear, accurate assessment findings allow respiratory therapists to communicate effectively with physicians, nurses, and other clinicians. This ensures coordinated and consistent care.
In short, assessment is what transforms respiratory therapy from task-based care into clinical practice.
Preparing for the Patient Encounter
Effective assessment begins before you ever lay eyes on the patient. Preparation improves efficiency, accuracy, and confidence.
Review the Medical Record
Before entering the room, review available information such as:
- Diagnosis and reason for admission
- Recent progress notes
- Physician orders
- Relevant lab values
- Imaging reports
- Previous respiratory assessments
Note: This background helps you anticipate potential problems and focus your assessment.
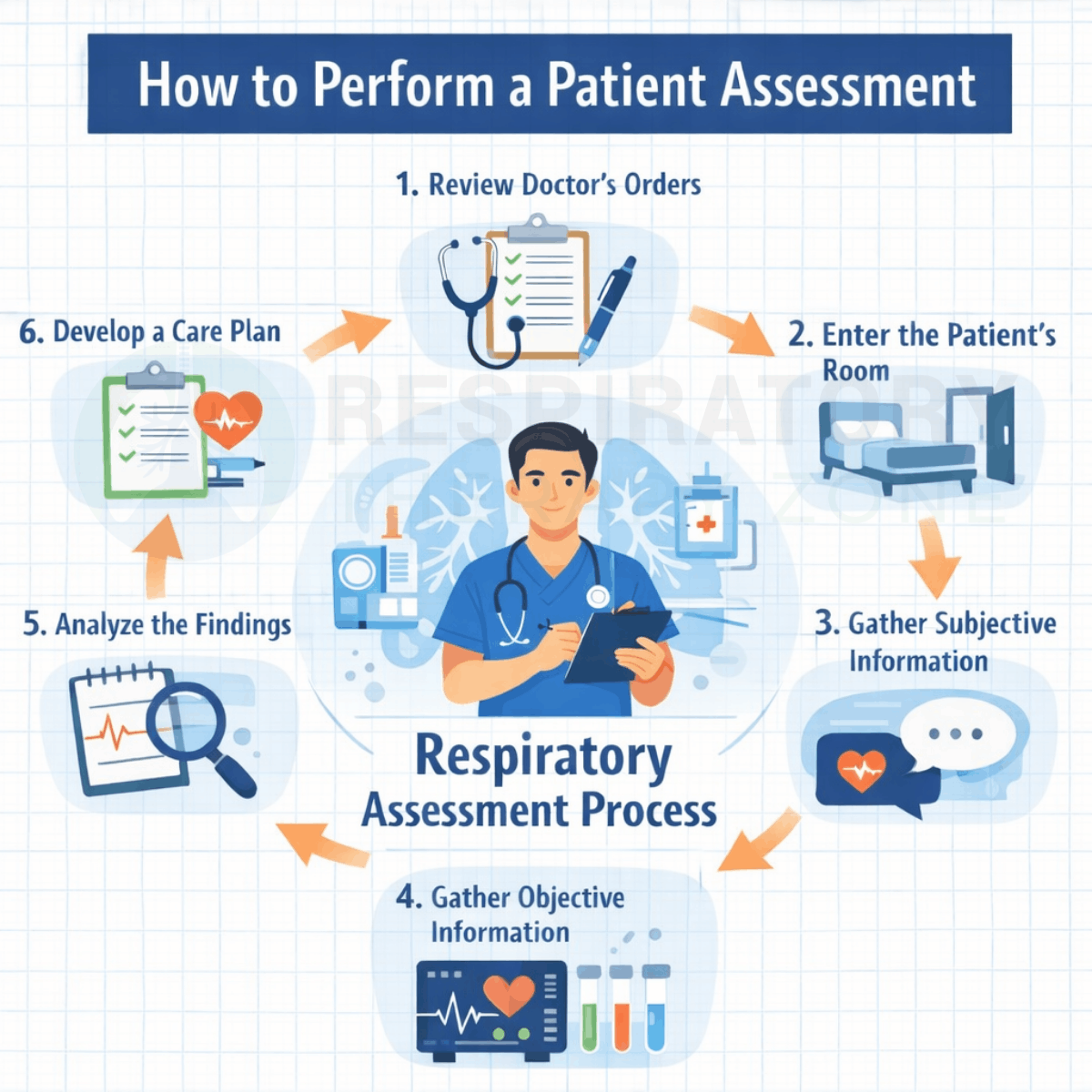
Verify the Doctor’s Order
Checking the physician’s order is the formal starting point of the assessment process. Orders clarify what is expected, what therapies are authorized, and whether specific evaluations are requested. This step ensures that your actions are appropriate and within scope.
Gather Necessary Equipment
Having the right tools readily available prevents interruptions and improves patient confidence. Common items include:
- Stethoscope
- Pulse oximeter
- Blood pressure cuff
- Watch or timer
- Personal protective equipment (PPE), if required
Prepare Yourself
Hand hygiene, proper PPE, and a professional mindset are essential. Enter the encounter focused, observant, and ready to listen.
Entering the Patient’s Room
The moment you enter the patient’s room, assessment begins. Your first impression provides valuable information before any formal questioning or examination occurs. Observe the patient’s position, level of alertness, facial expression, and apparent comfort. Note whether they are sitting upright, using accessory muscles, or appearing distressed.
Introduce yourself clearly, explain your role, and describe the purpose of your visit. Simple communication builds trust and encourages honest responses. A calm, respectful approach often leads to better cooperation and more accurate subjective information.
Environmental factors also matter. Take note of oxygen delivery devices, monitor readings, alarms, and the general condition of the room. These details provide context for your findings.
Gathering Subjective Patient Information
Subjective data comes directly from the patient or caregiver. It reflects how the patient feels and perceives their condition.
Key components include:
Chief Complaint
Ask the patient why they are seeking care or how they are feeling now. Shortness of breath, chest tightness, cough, fatigue, or dizziness may all be relevant.
Symptom Analysis
Explore symptoms in more detail by asking about:
- Onset and duration
- Severity
- Triggers or relieving factors
- Progression over time
Medical History
A focused history helps explain current findings. Important areas include:
- Previous respiratory conditions
- Cardiac history
- Recent infections
- Hospitalizations or surgeries
- Current medications and allergies
Lifestyle and Risk Factors
Smoking history, occupational exposures, exercise tolerance, and sleep habits can significantly affect respiratory status. Subjective information provides context. While it cannot be measured, it often points you toward the underlying problem.
Objective Assessment in Respiratory Care
Once subjective information has been gathered, the respiratory therapist transitions into objective assessment. This phase provides measurable, observable data that either supports or challenges what the patient reports. Objective findings are critical because they reveal how the body is functioning in real time and often uncover problems the patient may not recognize or communicate.
In respiratory care, objective assessment extends far beyond reading numbers on a monitor. It requires careful observation, hands-on examination, and thoughtful interpretation of findings within the clinical context. The goal is not simply to collect data, but to understand what that data means for the patient’s respiratory status and overall stability.
Vital Signs: The Foundation of Objective Assessment
Vital signs provide a rapid snapshot of physiological function and are often the first indicators of deterioration. Even subtle changes can carry significant clinical meaning.
Respiratory Rate
Respiratory rate is one of the most important vital signs in respiratory care and one of the most frequently overlooked. An increased rate may indicate hypoxemia, metabolic acidosis, anxiety, pain, or respiratory distress. A decreased rate may signal fatigue, neurological impairment, or medication effects.
Equally important is how the rate is measured. It should be observed, not assumed, and assessed in conjunction with effort and pattern.
Oxygen Saturation (SpO₂)
Pulse oximetry estimates the percentage of hemoglobin saturated with oxygen. While useful, it must be interpreted carefully. A normal SpO₂ does not guarantee adequate ventilation, nor does it rule out carbon dioxide retention.
Factors such as poor perfusion, motion, nail polish, and abnormal hemoglobin can affect accuracy. Oxygen saturation should always be interpreted alongside clinical appearance and, when available, arterial blood gas results.
Heart Rate and Blood Pressure
Tachycardia may be a compensatory response to hypoxemia or respiratory distress. Bradycardia can indicate severe hypoxia, advanced fatigue, or neurological involvement. Blood pressure trends provide insight into perfusion, shock, or fluid status, all of which influence respiratory function.
Temperature
Fever raises metabolic demand and oxygen consumption, often increasing respiratory workload. Hypothermia may depress respiratory drive. Temperature abnormalities should always be considered during respiratory assessment.
General Observation: The Power of Visual Assessment
Before touching the patient, a great deal of information can be obtained through observation alone.
Level of Consciousness
Changes in mental status are often early indicators of respiratory failure. Restlessness, agitation, confusion, or lethargy may reflect hypoxemia or hypercapnia. A calm but drowsy patient may be more concerning than an anxious one.
Positioning
Patients in respiratory distress often assume positions that maximize airflow, such as sitting upright or leaning forward. Inability to tolerate a supine position can suggest severe dyspnea or air hunger.
Work of Breathing
Assess for signs of increased work of breathing, including:
- Use of accessory muscles
- Nasal flaring
- Intercostal or suprasternal retractions
- Paradoxical chest movement
Note: These findings suggest increased respiratory demand or muscle fatigue and warrant immediate attention.
Skin Color and Condition
Cyanosis indicates increased deoxygenated hemoglobin and is often a late sign of hypoxemia. Pallor, diaphoresis, or mottling may suggest poor perfusion or shock.
Physical Examination of the Respiratory System
A systematic physical examination provides deeper insight into respiratory mechanics and lung function. This typically follows a structured approach.
Inspection
Inspection involves observing chest shape, symmetry, and movement. Unequal chest expansion may indicate pneumothorax, atelectasis, or consolidation. Barrel chest suggests chronic air trapping. Scars, deformities, or medical devices may provide additional clues.
Palpation
Palpation allows assessment of chest expansion and tactile fremitus. Decreased chest movement on one side may signal obstruction or lung collapse. Increased fremitus may be associated with consolidation, while decreased fremitus may indicate pleural effusion or pneumothorax.
Percussion
Percussion helps determine the density of underlying tissue. Dullness may suggest fluid or consolidation, while hyperresonance may indicate trapped air. Although sometimes underutilized, percussion can quickly narrow diagnostic possibilities.
Auscultation
Auscultation is a cornerstone of respiratory assessment. Listening systematically to all lung fields allows identification of abnormal breath sounds and ventilation patterns.
Common findings include:
- Crackles, often associated with fluid or alveolar collapse
- Wheezes, indicating airway narrowing
- Diminished or absent breath sounds, suggesting poor ventilation
- Bronchial breath sounds, often heard over consolidated lung tissue
Note: Breath sounds must be interpreted in conjunction with symptoms and other findings rather than in isolation.
Assessing Ventilation and Gas Exchange
Objective assessment must always consider both ventilation and oxygenation.
Ventilation
Ventilation refers to carbon dioxide removal. A patient may appear adequately oxygenated while retaining CO₂. Signs of inadequate ventilation include:
- Rising PaCO₂
- Altered mental status
- Shallow breathing
- Fatigue
Note: Arterial blood gas analysis provides definitive information about ventilation status and acid–base balance.
Oxygenation
Oxygenation reflects how effectively oxygen moves from the lungs into the blood. Oxygen delivery devices, flow rates, and FiO₂ should be documented and assessed for adequacy.
Worsening oxygen requirements, declining SpO₂, or increasing work of breathing despite therapy are red flags that require prompt evaluation.
Diagnostic Data as Part of the Objective Assessment
Objective assessment extends beyond bedside examination to include diagnostic tests.
Arterial Blood Gases
ABGs provide essential information about oxygenation, ventilation, and acid–base balance. Trends are often more important than single values. ABG interpretation should always be linked back to the patient’s clinical presentation.
Pulmonary Function Testing
When available, pulmonary function tests help quantify airflow limitation, restriction, and gas exchange impairment. These tests are especially valuable in chronic respiratory conditions and outpatient settings.
Chest Imaging
Chest X-rays and CT scans provide structural information that cannot be obtained through physical exam alone. Findings such as infiltrates, effusions, pneumothorax, or hyperinflation guide diagnosis and treatment decisions.
Cardiac Monitoring and EKG
Cardiac rhythm disturbances, ischemia, or ventricular strain can worsen respiratory status or mimic pulmonary pathology. Integrating cardiac findings into respiratory assessment ensures a more complete evaluation.
Putting Objective Findings Into Context
Objective data is only meaningful when interpreted correctly. Numbers and findings must be evaluated within the context of the patient’s baseline, diagnosis, and clinical trajectory.
A respiratory rate of 24 may be acceptable for one patient and dangerous for another. A “normal” oxygen saturation may still be inadequate if the patient is tiring or retaining CO₂. Trends, patterns, and correlations are far more informative than isolated values.
At this stage of the assessment, the respiratory therapist should be forming a clear understanding of:
- Severity of illness
- Stability or deterioration
- Effectiveness of current therapy
- Need for escalation or modification of care
Clinical Reasoning, Care Planning, and Reassessment in Respiratory Care
Patient assessment does not end once data has been collected. In many ways, the most important work begins after the assessment findings are gathered. This is the point where respiratory therapists transform information into understanding, and understanding into action.
Clinical reasoning is what separates meaningful assessment from simple data collection. It allows respiratory therapists to recognize patterns, prioritize problems, anticipate deterioration, and develop effective care plans. In this final part, we will explore how to analyze assessment findings, develop and implement a care plan, document appropriately, and reassess patients over time.
Analyzing Assessment Findings
Analysis involves synthesizing subjective and objective data to form a coherent clinical picture. Rather than viewing findings in isolation, respiratory therapists must ask how each piece of information relates to the others.
For example, an elevated respiratory rate paired with shallow breathing, rising PaCO₂, and increasing oxygen requirements suggests ventilatory failure rather than simple hypoxemia. Similarly, wheezing accompanied by prolonged expiratory phase and increased work of breathing points toward airway obstruction rather than parenchymal disease.
Effective analysis answers several key questions:
- What is the primary problem affecting this patient’s breathing?
- Are there secondary or contributing problems?
- Is the patient compensating, stable, or decompensating?
- How urgent is the situation?
Note: This process requires constant comparison between current findings and the patient’s baseline. A chronic COPD patient may tolerate values that would be dangerous for others. Context always matters.
Prioritizing Problems
Once analysis is complete, problems must be prioritized. Respiratory therapists often manage patients with multiple abnormalities, but not all issues require immediate intervention.
Priority is generally given to:
- Airway patency
- Adequacy of ventilation
- Adequacy of oxygenation
- Signs of fatigue or impending failure
- Hemodynamic instability affecting respiratory status
Note: For example, mild hypoxemia in a stable patient may be less urgent than signs of rising PaCO₂ with altered mental status. Prioritization ensures that interventions address the most life-threatening issues first.
Developing a Respiratory Care Plan
A care plan translates assessment findings into structured interventions. It should be individualized, evidence-based, and flexible.
A comprehensive respiratory care plan typically includes:
Identified Problems
Clear statements describing the patient’s respiratory issues, such as impaired gas exchange, ineffective airway clearance, or increased work of breathing.
Goals and Expected Outcomes
Goals should be specific and measurable. Examples include improved oxygen saturation, reduced respiratory rate, decreased work of breathing, or improved ABG values.
Interventions
Interventions may include oxygen therapy, bronchodilator administration, airway clearance techniques, ventilatory support, monitoring strategies, or patient education.
Monitoring Parameters
Define how response to therapy will be evaluated. This may include reassessment of breath sounds, vital signs, oxygen requirements, ABG results, or patient comfort.
Collaboration
Care plans should align with physician orders and integrate input from nursing, physical therapy, nutrition, and other disciplines when appropriate. The care plan should never be static. As the patient’s condition changes, the plan must be updated accordingly.
Implementing and Evaluating Interventions
Implementation is not simply delivering therapy. It involves continuous observation during and after interventions to assess effectiveness and detect complications.
For example, administering a bronchodilator requires monitoring for improved airflow, reduced wheezing, and decreased work of breathing, as well as potential side effects such as tachycardia or tremors. Oxygen therapy should be evaluated not only by SpO₂ but also by respiratory effort and mental status.
Note: Evaluation answers a critical question: Did the intervention achieve its intended goal? If not, reassessment and modification are required.
Reassessment: The Ongoing Nature of Patient Care
Reassessment is a defining feature of respiratory care. Patients’ respiratory status can change rapidly, especially in acute or critical settings.
Reassessment should occur:
- After any intervention
- When symptoms change
- At regular intervals based on acuity
- When concerns are raised by the patient or healthcare team
Reassessment follows the same principles as the initial assessment but often focuses on specific problem areas. Comparing new findings to previous data helps determine trends and guide next steps.
Note: Failure to reassess can lead to delayed recognition of deterioration or unnecessary continuation of ineffective therapy.
Documentation: Communicating Clinical Judgment
Accurate documentation is an essential component of patient assessment. It ensures continuity of care, supports clinical decisions, and serves as a legal record.
Effective documentation should:
- Reflect both subjective and objective findings
- Clearly describe assessment results
- Link findings to interventions
- Document patient response
- Use clear, objective language
Rather than listing numbers alone, documentation should tell the patient’s story. For example, documenting increased work of breathing and accessory muscle use provides more insight than reporting a respiratory rate alone.
Timely documentation ensures that other members of the healthcare team have access to current and relevant information.
Special Considerations in Different Patient Populations
ICU Patients
Assessments in the ICU are more frequent and complex. Mechanical ventilation, invasive monitoring, and multi-organ involvement require advanced interpretation skills and close collaboration with the healthcare team.
Pediatric and Neonatal Patients
Children and neonates have different normal values and often present differently than adults. Assessment relies heavily on observation, caregiver input, and age-appropriate norms.
Chronic Respiratory Patients
Patients with chronic disease often have adapted physiology. Understanding their baseline is essential to avoid over- or under-treatment.
Neurological or Sedated Patients
In patients unable to communicate, objective assessment and trend analysis become even more critical. Changes in vital signs or ventilator parameters may be the only clues to deterioration.
Patient Assessment Practice Questions
1. What is the primary purpose of patient assessment in respiratory care?
To gather and interpret clinical data in order to guide safe, effective, and individualized patient care.
2. Why is patient assessment considered more than a checklist or routine task?
Because it requires clinical reasoning to detect subtle changes that can affect patient safety and outcomes.
3. What role do respiratory therapists often play in early detection of patient deterioration?
They frequently identify early warning signs before alarms sound or lab values become critical.
4. What are the two main categories of data collected during a patient assessment?
Subjective data and objective data.
5. What is subjective data in a patient assessment?
Information reported directly by the patient, such as symptoms, sensations, or complaints.
6. What is objective data in a patient assessment?
Information that can be observed, measured, or verified by the clinician, such as vital signs and breath sounds.
7. Why must respiratory assessment consider the patient as a whole?
Because respiratory problems are often influenced by cardiac, neurological, metabolic, infectious, or psychological factors.
8. What key question does assessment answer regarding breathing?
How the patient is breathing at the present moment.
9. Why is evaluating gas exchange a critical component of patient assessment?
To determine whether oxygenation and ventilation are adequate.
10. How does patient assessment help determine the effectiveness of therapy?
By showing measurable changes that indicate improvement, stability, or deterioration.
11. Why is patient assessment considered a continuous process?
Because patient status can change over time and requires ongoing evaluation.
12. What is meant by establishing a baseline during patient assessment?
Creating an initial reference point for comparison with future assessments.
13. Why is a baseline assessment essential for tracking patient progress?
Without it, changes in condition cannot be accurately identified or quantified.
14. What types of changes often signal early respiratory deterioration?
Changes in respiratory rate, work of breathing, mental status, or breath sounds.
15. How does early identification of abnormalities improve patient outcomes?
It allows earlier intervention and prevents progression to severe illness.
16. How does patient assessment guide clinical decision-making?
It determines when therapy should be started, adjusted, escalated, or discontinued.
17. Why is monitoring response to therapy a key function of assessment?
Because treatments must produce measurable improvement to be considered effective.
18. How does patient assessment contribute to patient safety?
By identifying risks such as airway compromise, hypoxemia, fatigue, or impending respiratory failure.
19. In what way does patient assessment support interprofessional communication?
By providing clear, accurate clinical information to guide coordinated care.
20. How does thorough assessment elevate respiratory care from task-based to clinical practice?
By integrating observation, reasoning, and decision-making to deliver patient-centered care.
21. Why does effective patient assessment begin before entering the patient’s room?
Because reviewing background information improves efficiency, accuracy, and anticipation of potential problems.
22. What types of information should be reviewed in the medical record before seeing the patient?
Diagnosis, reason for admission, progress notes, physician orders, labs, imaging, and prior respiratory assessments.
23. How does reviewing prior respiratory assessments help guide the current evaluation?
It provides a baseline and reveals trends or changes in the patient’s condition.
24. Why is verifying the physician’s order a critical step before assessment?
It clarifies authorized therapies, requested evaluations, and ensures actions are appropriate and within scope.
25. What problems can occur if the physician’s order is not verified?
Inappropriate therapy, missed evaluations, or delays in care.
26. Why is gathering equipment before entering the room important?
It prevents interruptions, improves efficiency, and increases patient confidence.
27. What basic equipment is commonly required for a respiratory assessment?
Stethoscope, pulse oximeter, blood pressure cuff, timer or watch, and PPE if needed.
28. Why is hand hygiene considered part of assessment preparation?
Because infection prevention is essential for patient safety and clinician protection.
29. What is meant by entering the patient encounter with a “professional mindset”?
Being focused, observant, respectful, and prepared to listen.
30. When does patient assessment truly begin?
The moment the clinician enters the patient’s room.
31. What information can be obtained from the first visual impression of a patient?
Positioning, level of alertness, comfort, respiratory effort, and signs of distress.
32. Why is observing patient posture important during assessment?
Certain positions, such as sitting upright, may indicate increased work of breathing.
33. What does the use of accessory muscles suggest?
Increased respiratory effort or respiratory distress.
34. Why is introducing yourself and explaining your role important?
It builds trust and encourages accurate and honest patient responses.
35. How does effective communication improve the quality of subjective data?
Patients are more likely to share relevant symptoms and concerns.
36. What environmental factors should be noted upon entering the patient’s room?
Oxygen devices, monitor readings, alarms, and overall room setup.
37. Why are oxygen delivery devices part of the assessment?
They provide context for oxygenation status and current therapy.
38. What is subjective patient information?
Data reported directly by the patient or caregiver about symptoms and feelings.
39. What is the purpose of identifying the patient’s chief complaint?
To understand the primary reason for concern or change in condition.
40. What respiratory-related complaints commonly guide further assessment?
Shortness of breath, chest tightness, cough, fatigue, and dizziness.
41. Why is symptom onset and duration important?
They help distinguish acute conditions from chronic or progressive problems.
42. How does symptom severity influence clinical priorities?
More severe symptoms may require immediate intervention.
43. Why should triggers and relieving factors be explored?
They help identify underlying causes and guide treatment decisions.
44. What aspects of medical history are most relevant to respiratory assessment?
Prior lung disease, cardiac history, infections, surgeries, medications, and allergies.
45. Why is medication history important in respiratory assessment?
Medications can affect breathing, gas exchange, and respiratory drive.
46. How do lifestyle factors such as smoking influence respiratory status?
They increase risk for airway disease and impaired gas exchange.
47. Why is objective assessment necessary after gathering subjective data?
It provides measurable evidence of physiological function.
48. What is the primary goal of objective respiratory assessment?
To determine current respiratory function and stability.
49. Why should objective findings be interpreted in clinical context?
Because numbers alone may not reflect the patient’s true condition.
50. Why are vital signs considered the foundation of objective assessment?
They provide rapid insight into respiratory, cardiovascular, and metabolic status.
51. Why is respiratory rate one of the most important vital signs?
It is a sensitive indicator of respiratory distress or deterioration.
52. What conditions can cause an increased respiratory rate?
Hypoxemia, metabolic acidosis, pain, anxiety, or respiratory distress.
53. What may a decreased respiratory rate indicate?
Fatigue, neurological impairment, or medication effects.
54. Why should respiratory rate be directly observed rather than estimated?
Estimation often leads to inaccurate assessment.
55. Why must respiratory rate be evaluated along with effort and pattern?
Because rate alone does not reflect the work of breathing.
56. What does pulse oximetry measure?
The percentage of hemoglobin saturated with oxygen.
57. Why does a normal SpO₂ not guarantee adequate ventilation?
Because carbon dioxide retention may still be present.
58. What factors can interfere with accurate pulse oximetry readings?
Poor perfusion, motion, nail polish, and abnormal hemoglobin.
59. Why should SpO₂ be interpreted alongside clinical appearance?
Because oxygen saturation does not reflect ventilation or work of breathing.
60. What does tachycardia often indicate during respiratory distress?
A compensatory response to hypoxemia or increased workload.
61. Why is blood pressure important in respiratory assessment?
It reflects perfusion, shock, and fluid status that influence breathing.
62. How can fever affect respiratory workload?
By increasing metabolic demand and oxygen consumption.
63. Why is temperature assessment relevant to respiratory care?
Abnormal temperature can alter respiratory drive and workload.
64. Why is general observation considered a critical part of patient assessment?
Because significant clinical information can be obtained before touching or questioning the patient.
65. What mental status changes may indicate early respiratory failure?
Restlessness, agitation, confusion, lethargy, or decreased alertness.
66. Why can a calm but drowsy patient be more concerning than an anxious one?
Because drowsiness may indicate CO₂ retention or worsening hypoxemia.
67. What patient position commonly indicates respiratory distress?
Sitting upright or leaning forward to maximize airflow.
68. What does inability to tolerate a supine position suggest?
Severe dyspnea or air hunger.
69. What clinical signs indicate increased work of breathing?
Accessory muscle use, nasal flaring, retractions, and paradoxical chest movement.
70. Why is paradoxical chest movement concerning?
It suggests respiratory muscle fatigue or impending ventilatory failure.
71. What does cyanosis indicate during respiratory assessment?
Increased deoxygenated hemoglobin and late-stage hypoxemia.
72. What skin findings may suggest poor perfusion or shock?
Pallor, diaphoresis, or mottling.
73. What is the purpose of inspecting the chest during assessment?
To evaluate chest shape, symmetry, and movement.
74. What does unequal chest expansion suggest?
Conditions such as pneumothorax, atelectasis, or consolidation.
75. What chest shape is commonly associated with chronic air trapping?
Barrel chest
76. Why is palpation used during respiratory assessment?
To assess chest expansion and tactile fremitus.
77. What does increased tactile fremitus indicate?
Lung consolidation
78. What conditions are associated with decreased tactile fremitus?
Pleural effusion or pneumothorax.
79. What information does percussion provide during assessment?
Insight into underlying tissue density.
80. What does dullness to percussion suggest?
Fluid accumulation or lung consolidation.
81. What does hyperresonance to percussion indicate?
Trapped air, such as in pneumothorax or emphysema.
82. Why is auscultation a cornerstone of respiratory assessment?
It helps identify abnormal breath sounds and ventilation patterns.
83. What lung sounds are commonly associated with alveolar fluid or collapse?
Crackles
84. What does wheezing typically indicate?
Airway narrowing or obstruction.
85. What does diminished or absent breath sounds suggest?
Poor ventilation or airway obstruction.
86. When are bronchial breath sounds considered abnormal?
When heard over peripheral lung fields.
87. Why must breath sounds be interpreted with other findings?
Because isolated sounds may not reflect the full clinical picture.
88. What does ventilation primarily refer to?
Carbon dioxide removal from the body.
89. What signs suggest inadequate ventilation?
Rising PaCO₂, altered mental status, shallow breathing, and fatigue.
90. What diagnostic test provides definitive information about ventilation?
Arterial blood gas analysis.
91. What does oxygenation reflect in respiratory assessment?
The effectiveness of oxygen transfer from the lungs to the blood.
92. Why should oxygen delivery devices and FiO₂ be documented?
To assess adequacy of oxygen therapy and changes in requirements.
93. What does increasing oxygen requirement despite therapy indicate?
Possible clinical deterioration.
94. Why are trends in ABG values more important than single results?
They reveal progression, improvement, or worsening over time.
95. What role do pulmonary function tests play in assessment?
They quantify airflow limitation, restriction, and gas exchange impairment.
96. Why is chest imaging essential in respiratory assessment?
It reveals structural abnormalities not detectable by physical exam.
97. What conditions can chest imaging help identify?
Infiltrates, effusions, pneumothorax, and hyperinflation.
98. Why should cardiac monitoring be included in respiratory assessment?
Cardiac abnormalities can worsen or mimic respiratory conditions.
99. Why must objective findings be interpreted within clinical context?
Because normal values may be unsafe depending on the patient’s baseline.
100. What is the role of clinical reasoning in patient assessment?
To transform collected data into meaningful, actionable decisions.
Final Thoughts
Patient assessment is the backbone of respiratory therapy practice. From preparation and observation to analysis, care planning, and reassessment, each step builds upon the last. Respiratory therapists who develop strong assessment skills are better equipped to recognize early deterioration, guide effective treatment, communicate clearly with the healthcare team, and improve patient outcomes.
Mastery of patient assessment is not achieved through memorization alone. It develops through practice, reflection, and a commitment to understanding the “why” behind every finding.
By approaching assessment as a dynamic, ongoing process, respiratory therapists ensure that their care remains patient-centered, responsive, and clinically sound.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Christalle E, Zill JM, Frerichs W, Härter M, Nestoriuc Y, Dirmaier J, Scholl I. Assessment of patient information needs: A systematic review of measures. PLoS One. 2019.