Pulmonary toilet, also known as pulmonary hygiene, refers to a set of therapeutic techniques used to clear mucus and secretions from the airways to improve respiratory function and prevent complications such as pneumonia and atelectasis.
This approach is especially important for patients who are unable to clear their airways effectively due to conditions like chronic obstructive pulmonary disease (COPD), cystic fibrosis, neuromuscular disorders, or after major surgery.
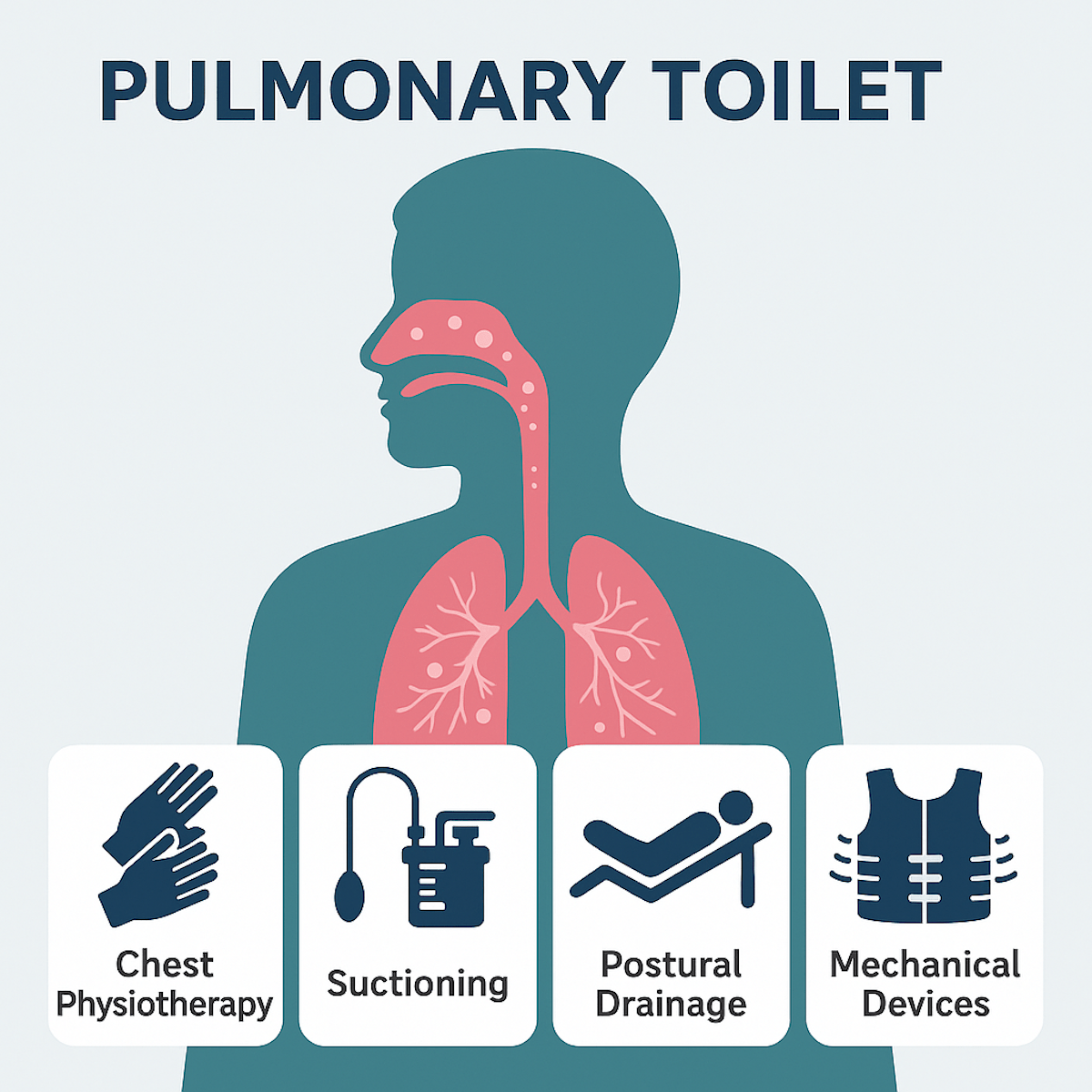
From chest physiotherapy and suctioning to postural drainage and mechanical devices, pulmonary toilet plays a critical role in maintaining airway patency and enhancing oxygenation. In this article, we’ll explore the different methods of pulmonary toilet, who benefits from it, and why it remains a vital component of respiratory care.
Download our free guide that has over 100+ of the best tips for healthy lungs.
What is Pulmonary Toilet?
Pulmonary toilet refers to a set of medical techniques designed to clear mucus and secretions from the lungs and airways. These methods play an important role in preventing respiratory complications and maintaining effective lung function.
Meaning of Pulmonary Toilet
Pulmonary toilet, also known as bronchial hygiene therapy, includes procedures that help remove secretions from the bronchial tree. These techniques may involve chest physiotherapy, postural drainage, suctioning, and coughing exercises.
The main goal is to prevent airway obstruction, reduce infection risk, and improve breathing efficiency. Pulmonary toilet is especially important for patients who have trouble clearing secretions on their own, such as those with chronic lung diseases or those after surgery.
Common reasons for using pulmonary toilet include conditions like pneumonia, cystic fibrosis, or neuromuscular disorders. Health care teams select techniques based on a patient’s needs and medical condition.
History and Evolution
The origins of pulmonary toilet can be traced to the early 20th century, when respiratory therapy began to gain recognition in clinical practice. Early strategies included manual chest percussion and postural drainage, which were often used for patients with tuberculosis or bronchiectasis.
Over time, advances in equipment and understanding of lung mechanics led to more refined techniques. The introduction of mechanical suction devices and positive expiratory pressure therapies improved the effectiveness of secretion removal.
Today, pulmonary toilet is a standard component of care in hospitals and long-term care settings. It has evolved with input from pulmonologists, respiratory therapists, and evidence-based research. Each advancement has aimed to make clearance procedures safer, more efficient, and comfortable for patients.
Mechanisms of Airway Clearance
Airway clearance relies on coordinated physiological actions and specialized structures within the respiratory system. Lesions or dysfunction in these pathways can result in impaired lung hygiene and increased risk for respiratory complications.
Physiological Processes
Airway clearance begins with the production of mucus by goblet cells and submucosal glands. This mucus traps inhaled particles, microorganisms, and debris, creating a barrier to deeper lung penetration.
Coughing is a key defense, triggered by sensory nerve endings detecting irritants or mucus buildup. A deep inhalation, followed by forced expiration against a closed glottis, produces high airflow velocities that dislodge and expel secretions.
Normal hydration of airway secretions is essential. Dehydrated or thick mucus is harder to mobilize, increasing obstruction risk. Gravity and changes in body position also contribute by shifting and moving mucus within the airways.
Mucociliary Escalator Function
The mucociliary escalator consists of ciliated epithelial cells lining the airways. These cilia beat in coordinated waves, moving mucus upwards toward the pharynx.
This movement is continuous, dependent on healthy cilia and the right mucus consistency. Impaired ciliary function or overly viscous mucus slows clearance, promoting stasis and infection risk.
Airway surface liquid is divided into a periciliary layer and the outer mucus layer. The cilia operate most effectively when both layers are of normal depth and composition. Smoking, pollution, and genetic disorders like cystic fibrosis commonly disrupt this system.
Indications for Pulmonary Toilet
Pulmonary toilet is necessary when airway clearance is compromised or secretions accumulate, risking serious respiratory complications. Identifying when intervention is required relies on understanding the specific clinical conditions and risk factors involved.
Clinical Conditions Requiring Airway Clearance
Certain diseases and surgical procedures make airway clearance crucial. Patients with chronic obstructive pulmonary disease (COPD) and cystic fibrosis often experience excess mucus production that their bodies struggle to clear. Bronchiectasis is another condition marked by persistent airway dilation and mucus buildup, making pulmonary toilet essential.
Neuromuscular disorders such as amyotrophic lateral sclerosis (ALS) and muscular dystrophy can weaken respiratory muscles, reducing effective cough and clearance. Those with pneumonia or who require prolonged mechanical ventilation frequently need airway clearance to prevent blockage and infection. After thoracic or abdominal surgery, patients may be unable to cough adequately due to pain or sedation, so routine pulmonary toilet becomes an important part of their care.
Risk Factors for Secretion Retention
Secretion retention can arise from a variety of risk factors even without a primary pulmonary diagnosis. People with decreased level of consciousness—such as after stroke, head injury, or as a result of sedation—are less able to clear secretions. Aging also decreases cough strength and mucociliary function, increasing risk.
Immobility—whether from critical illness, trauma, or prolonged bed rest—prevents deep breaths and effective coughing, increasing the chance of secretion accumulation. Dehydration thickens mucus, making it harder to clear. Intubated and tracheostomized patients are especially vulnerable due to impaired natural airway defenses and mechanical issues related to tubes. Recognizing these risk factors helps clinicians anticipate the need for pulmonary toilet.
Techniques and Methods
Pulmonary toilet relies on targeted interventions to clear secretions and improve lung function in patients who cannot effectively clear their own airways. Manual techniques and medical devices are commonly used for these purposes.
Manual Chest Physiotherapy
Manual chest physiotherapy involves a combination of physical maneuvers to mobilize and loosen mucus in the lungs. Techniques include percussion (clapping on the chest wall), vibration, and postural drainage, where the patient’s body is positioned to facilitate mucus drainage from different lung segments.
Percussion is performed by rhythmically striking the chest wall with cupped hands, which helps to dislodge mucus from airways. Vibration uses a gentle, shaking motion applied during exhalation to move secretions toward larger airways.
Postural drainage positions are selected based on which lung segment needs clearance. Sessions usually last 20–30 minutes and may be repeated several times a day. These techniques are frequently used for patients with chronic lung diseases or after surgery.
Suctioning Procedures
Suctioning removes secretions directly from the airway using a catheter connected to suction equipment. This procedure is essential for patients who are unable to cough or clear their secretions on their own, such as those who are intubated or have tracheostomies.
Suctioning can be performed through the nose (nasopharyngeal), mouth (oropharyngeal), or directly through a tracheostomy tube. It requires strict adherence to sterile technique to reduce infection risk.
Nurses and respiratory therapists monitor heart rate, oxygen saturation, and respiratory status before, during, and after suctioning. Complications can include hypoxemia and mucosal injury, so each suctioning episode should be as brief as possible, usually less than 15 seconds.
Mechanical Airway Clearance Devices
Mechanical airway clearance devices assist patients who have difficulty clearing pulmonary secretions with traditional methods. These devices use physical forces to help mobilize mucus and improve lung function in individuals with conditions like cystic fibrosis, bronchiectasis, and chronic obstructive pulmonary disease.
High-Frequency Chest Wall Oscillation
High-frequency chest wall oscillation (HFCWO) devices use an inflatable vest connected to an air pulse generator. The vest rapidly inflates and deflates, creating vibrations across the chest. These mechanical pulses loosen mucus from the airway walls and enhance mobilization toward the trachea for easier expectoration.
HFCWO is effective for patients who cannot perform manual chest physiotherapy or need frequent treatments. Sessions typically last 20 to 30 minutes, with oscillation frequencies and pressures that can be adjusted for comfort and effectiveness. These devices are commonly used in hospital settings and at home, especially for chronic pulmonary diseases. Regular use may reduce the risk of infection and hospitalizations.
Positive Expiratory Pressure Therapy
Positive expiratory pressure (PEP) therapy involves breathing out through a device that creates resistance, increasing pressure in the airways during exhalation. This back pressure helps keep smaller airways open, allowing trapped mucus to move toward larger air passages.
PEP devices are portable, easy to use, and suitable for both children and adults. Patients inhale deeply and exhale steadily through a mouthpiece or mask, repeating this process for several minutes. This therapy can be performed independently and is often combined with other airway clearance techniques. Regular, correct use can help decrease airway obstruction and improve lung expansion.
Implementation in Hospital Settings
Pulmonary toilet involves a combination of procedures that support airway clearance and secretion management. Specific protocols are adapted for critically ill individuals and for patients recovering from surgery to lessen respiratory complications.
Protocols for Critically Ill Patients
Critically ill patients often require mechanical ventilation, making airway clearance a priority. Chest physiotherapy—including percussion, vibration, and postural drainage—is performed by trained staff at set intervals. Regular suctioning is scheduled to prevent mucus plugging, particularly in sedated or immobile patients.
Protocols may specify the use of humidified oxygen to loosen secretions. Nebulized bronchodilators or mucolytics are sometimes added to assist in secretion mobilization. Strict infection control is essential, with disposable suction catheters and personal protective equipment (PPE) for all caregivers.
Team-based care involving respiratory therapists, nurses, and physicians ensures that airway clearance strategies are integrated with overall patient management. Documentation of each intervention, including time and response, helps adjust frequency and method as the patient’s condition changes.
Postoperative Pulmonary Toilet
After surgery, pulmonary toilet focuses on reducing the risk of atelectasis and pneumonia. Deep breathing exercises, often with incentive spirometry, are initiated as soon as the patient is able. Nurses or respiratory therapists supervise these exercises and encourage frequent coughing, preferably with proper splinting to minimize pain.
Early mobilization is promoted, with patients assisted to sit up and ambulate as soon as medically feasible. Hydration is maintained by monitoring fluid intake to thin respiratory secretions. Instruction in correct techniques for coughing and deep breathing is provided to the patient and family members.
Pain management is addressed to support effective respiratory efforts, and in some cases, scheduled bronchodilators or mucolytics are administered. Protocols are adjusted to the type of surgery and individual risk factors for pulmonary complications.
Pulmonary Toilet in Chronic Disease Management
Pulmonary toilet plays a crucial role in managing chronic diseases that involve abnormal mucus production, impaired airway clearance, or frequent respiratory infections. Techniques must be tailored to specific conditions for optimal results.
Cystic Fibrosis
In cystic fibrosis, thick, sticky mucus poses a constant risk of airway obstruction and infection. Pulmonary toilet is a cornerstone of daily therapy to maintain airway patency and reduce bacterial colonization.
Patients use chest physiotherapy, which includes manual percussion and vibration of the chest wall. Devices like positive expiratory pressure (PEP) masks and high-frequency chest wall oscillation vests help mobilize secretions. Regular, scheduled airway clearance is recommended several times daily, particularly during illness or exacerbations.
Inhaled medications such as hypertonic saline or dornase alfa are commonly used before airway clearance sessions to thin mucus and improve removal. The routine also often involves forced expiratory techniques, such as huff coughing, designed to clear mucus without collapsing airways.
Chronic Obstructive Pulmonary Disease
Chronic Obstructive Pulmonary Disease (COPD) often leads to chronic cough and sputum production, especially in chronic bronchitis. Pulmonary toilet can support these patients by enhancing clearance and limiting infection risk.
Physical methods include active cycle of breathing techniques, autogenic drainage, and occasionally, manual chest percussion for selected individuals. Patients may use handheld positive expiratory pressure (PEP) devices to aid secretion movement when conventional methods are insufficient.
Proper hydration and inhaled bronchodilators can help thin sputum and facilitate effective airway clearance. Smoking cessation and minimizing air pollution exposure remain vital, but integrating pulmonary toilet techniques can further reduce the chance of exacerbations and hospitalizations.
Pulmonary Toilet in Pediatrics
Pulmonary toilet in children focuses on safe, effective airway clearance techniques. Special care is required due to differences in anatomy, physiology, and tolerance of procedures compared to adults.
Special Considerations for Children
Children, especially infants, have smaller airways and weaker respiratory muscles, making them prone to mucus plugging and atelectasis. Techniques such as chest physiotherapy, postural drainage, and suctioning are often adjusted to match the child’s age, size, and underlying condition.
Caregivers and healthcare providers must consider the child’s comfort and ability to cooperate. Non-invasive approaches like incentive spirometry or bubble blowing may be used when possible. Monitoring for adverse reactions such as hypoxia or increased distress is critical. Clear communication with families about the goals and methods of pulmonary toilet helps reduce anxiety and improves compliance.
Complications and Risks
Pulmonary toilet is an important intervention, but it carries certain risks that must be carefully managed. Understanding both the possible adverse effects and strategies to minimize harm is essential for safer patient care.
Potential Adverse Effects
Common risks include airway trauma and infection. Suctioning and repeated procedures may cause irritation or bleeding of the bronchial or oropharyngeal tissues. Infection is a notable concern, especially if sterile technique is not followed. Introduction of organisms can result in pneumonia or tracheobronchitis.
Patients may also experience hypoxemia and bronchospasm during or after procedures. Both can rapidly worsen respiratory function, especially in those with existing lung disease.
Note: Less frequent but serious issues include pneumothorax, cardiac arrhythmias, or laryngospasm. The likelihood of complications may increase in patients with frail tissue or unstable respiratory status.
Prevention and Management Strategies
Careful technique reduces most risks of pulmonary toilet. Using sterile equipment and proper hand hygiene minimizes infection. Monitoring oxygen saturation and vital signs before, during, and after procedures helps detect problems early. If significant changes occur, pausing or modifying the intervention may be necessary.
Pre-oxygenating patients at risk for hypoxemia, using gentle suction, and limiting procedure duration decrease adverse events. Staff training and following institutional protocols support consistent safe practices.
When complications arise, prompt recognition and targeted treatment—such as supplemental oxygen, wound care, or medications—improve outcomes. Regular reassessment ensures the chosen method remains appropriate for the patient’s evolving condition.
Patient Education and Home Care
Proper education improves patient compliance and reduces complications related to pulmonary toilet. Knowledge of at-home techniques and support for caregivers is essential for safe, effective airway clearance.
Self-Management Techniques
Patients should be shown how to perform coughing and deep breathing exercises. These techniques help mobilize and clear respiratory secretions. Incentive spirometry, when used regularly, encourages lung expansion and prevents atelectasis.
Hydration is important, as adequate fluid intake keeps mucus thinner and easier to expel. Patients may also benefit from positioning strategies, such as sitting upright or using postural drainage, to promote mucus movement.
Consistency is key. Daily routines and using reminders or setting schedules can help keep airway clearance on track. Patients should learn to recognize signs of inadequate clearance, like increased coughing, shortness of breath, fever, or changes in sputum color, and when to report these to a healthcare provider.
Caregiver Training
Caregivers must understand proper hand hygiene and infection control before assisting with any airway clearance techniques. They should learn how to use and maintain devices like suction machines, nebulizers, or chest percussion tools.
Training involves hands-on demonstrations and supervised practice until the caregiver is comfortable and competent. Written instructions and visual aids support learning and recall.
Caregivers also need to recognize symptoms that require medical attention, such as sudden breathing difficulty or reduced oxygen saturation. Encouraging communication with healthcare teams and attending follow-up appointments support ongoing care and safety at home.
Emerging Approaches and Research
Recent advancements in pulmonary toilet focus on improving secretion clearance and minimizing patient discomfort. Research is evaluating the safety, effectiveness, and practicality of these methods in diverse patient groups.
Innovative Technologies
New devices such as high-frequency chest wall oscillation vests and mechanical insufflation-exsufflation machines are being adopted in clinical practice. These technologies are designed to mobilize airway secretions in patients unable to clear them independently.
High-frequency percussive ventilation, for instance, combines airway pressure and oscillatory flow. Some centers use portable intrapulmonary percussive ventilation for homecare. Mobile health apps and remote monitoring allow clinicians to track adherence and lung health, tailoring regimens for individual needs.
Notably, advances in aerosol delivery, like vibrating mesh nebulizers, provide more efficient drug deposition while limiting systemic exposure. These innovations seek to optimize respiratory therapy, reduce infection risk, and support chronic disease management.
Clinical Trials and Evidence
Ongoing clinical trials are assessing the efficacy of both traditional and novel pulmonary toileting techniques. Studies compare the benefits of oscillation devices versus manual CPT in populations with cystic fibrosis, neuromuscular disease, and critical illness.
Preliminary data suggests that mechanical devices may offer similar or greater secretion clearance compared to manual techniques in select patients. Investigators are also examining patient outcomes such as rates of ventilator-associated pneumonia and length of hospital stay.
While some trials indicate improved quality of life with newer interventions, evidence is mixed regarding long-term benefits. Clinicians must weigh factors like patient tolerance, cost, and accessibility when choosing among emerging options.
Pulmonary Toilet in Global Health Contexts
Pulmonary toilet plays a critical role in managing respiratory health worldwide. Low- and middle-income countries often face a higher burden of respiratory diseases due to limited resources, high pollution, and infectious diseases such as tuberculosis.
Access to basic airway clearance techniques, such as chest physiotherapy and controlled coughing, can help reduce complications in communities with few medical devices. However, healthcare worker training and access to equipment like suction devices are frequently limited in these settings.
In areas with limited hospital resources, families may be taught simple pulmonary toilet methods at home. Patient education and community health programs can increase awareness about the importance of airway clearance, especially for children and people with chronic lung diseases.
Global health organizations occasionally include pulmonary toilet protocols in guidelines for managing pneumonia and other respiratory infections. Emphasis is placed on adaptable methods such as positioning and assisted coughing to accommodate varying levels of resource availability.
Note: The practice of pulmonary toilet in global health requires consideration of cultural beliefs, health literacy, and resource constraints. Integrating locally appropriate techniques can improve outcomes for vulnerable populations.
FAQs About Pulmonary Toilet
What Does Pulmonary Toilet Mean in Medical Terms?
Pulmonary toilet, also known as pulmonary hygiene, is a medical term for a set of techniques used to clear mucus and secretions from the lungs and airways. These techniques help prevent respiratory complications such as pneumonia, atelectasis, or airway obstruction, especially in patients with impaired ability to clear their lungs.
It is commonly used in hospitals, especially for patients who are sedated, intubated, or suffering from chronic lung diseases like COPD or cystic fibrosis.
What Are the Exercises for Pulmonary Toilet?
Exercises for pulmonary toilet include deep breathing exercises, incentive spirometry, controlled coughing, and diaphragmatic breathing. These techniques help expand the lungs, loosen mucus, and make it easier to expectorate secretions.
Some patients may also benefit from pursed-lip breathing and segmental breathing exercises. These are often taught by respiratory therapists and are crucial for post-operative patients or individuals with chronic respiratory conditions to help improve ventilation and prevent complications like atelectasis or infections.
What Is Bronchial Toileting?
Bronchial toileting is another term for pulmonary toilet that specifically refers to the clearance of mucus and secretions from the bronchial tubes. This can be achieved through methods such as suctioning, postural drainage, chest physiotherapy, and coughing techniques.
The goal is to maintain clear airways and prevent mucus plugs, which can lead to infection or lung collapse. It is frequently used in critical care settings and for patients with tracheostomies, ventilators, or diseases that impair normal mucus clearance.
What Are Some Examples of Pulmonary Toilet?
Examples of pulmonary toilet techniques include chest physiotherapy (percussion and vibration), postural drainage, suctioning, incentive spirometry, and mechanical devices like high-frequency chest wall oscillation vests. Nebulized bronchodilators or mucolytics may also be used to loosen thick secretions before clearance techniques are applied.
Each method aims to improve airway clearance and lung function. These techniques are often used in combination depending on the patient’s condition and ability to participate in active therapies like coughing or breathing exercises.
What Are the Contraindications for Pulmonary Toilet?
Contraindications for pulmonary toilet vary depending on the technique used but may include recent head or spinal injury, rib fractures, active bleeding, or unstable cardiovascular conditions. For example, chest physiotherapy may be avoided in patients with osteoporosis or recent thoracic surgery.
Suctioning can cause complications in patients with increased intracranial pressure. Each case must be evaluated individually, and the risks weighed against the benefits before performing pulmonary toilet, especially in critically ill or postoperative patients.
Final Thoughts
Pulmonary toilet is an essential practice in both acute and long-term respiratory care. By helping to mobilize and remove secretions from the lungs, it reduces the risk of infection, improves breathing efficiency, and enhances patient outcomes.
Whether through manual techniques or advanced mechanical aids, effective pulmonary hygiene supports lung function and quality of life for individuals with compromised airway clearance. Understanding and applying these techniques can make a significant difference in respiratory health and recovery.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Jelic S, Cunningham JA, Factor P. Clinical review: airway hygiene in the intensive care unit. Crit Care. 2008.
- Baltazar GA, Chendrasekhar A, Akella K, Chow P, Rubinshteyn V, Cohen D, Ruiz C, Genovese-Scullin DF, Patwari J, Harris L. Pulmonary Hygiene Protocol Reduces Incidence of Lobar Collapse in Severe Traumatic Brain Injury. Cureus. 2020.