Shortness of breath, or dyspnea, can make it difficult to relax, let alone get a restful night’s sleep. Whether it’s due to a chronic condition like COPD, asthma, heart failure, or simply a temporary respiratory issue, struggling to breathe while lying down can be both physically and emotionally exhausting.
Fortunately, your sleeping position can make a big difference. Certain postures help open up the airways, improve lung expansion, and reduce pressure on the chest, making it easier to breathe. In this article, we’ll explore the best sleeping positions for relieving shortness of breath and promoting better rest.
Download our free guide that has over 100+ of the best tips for healthy lungs.
What is the Best Sleeping Position for Shortness of Breath?
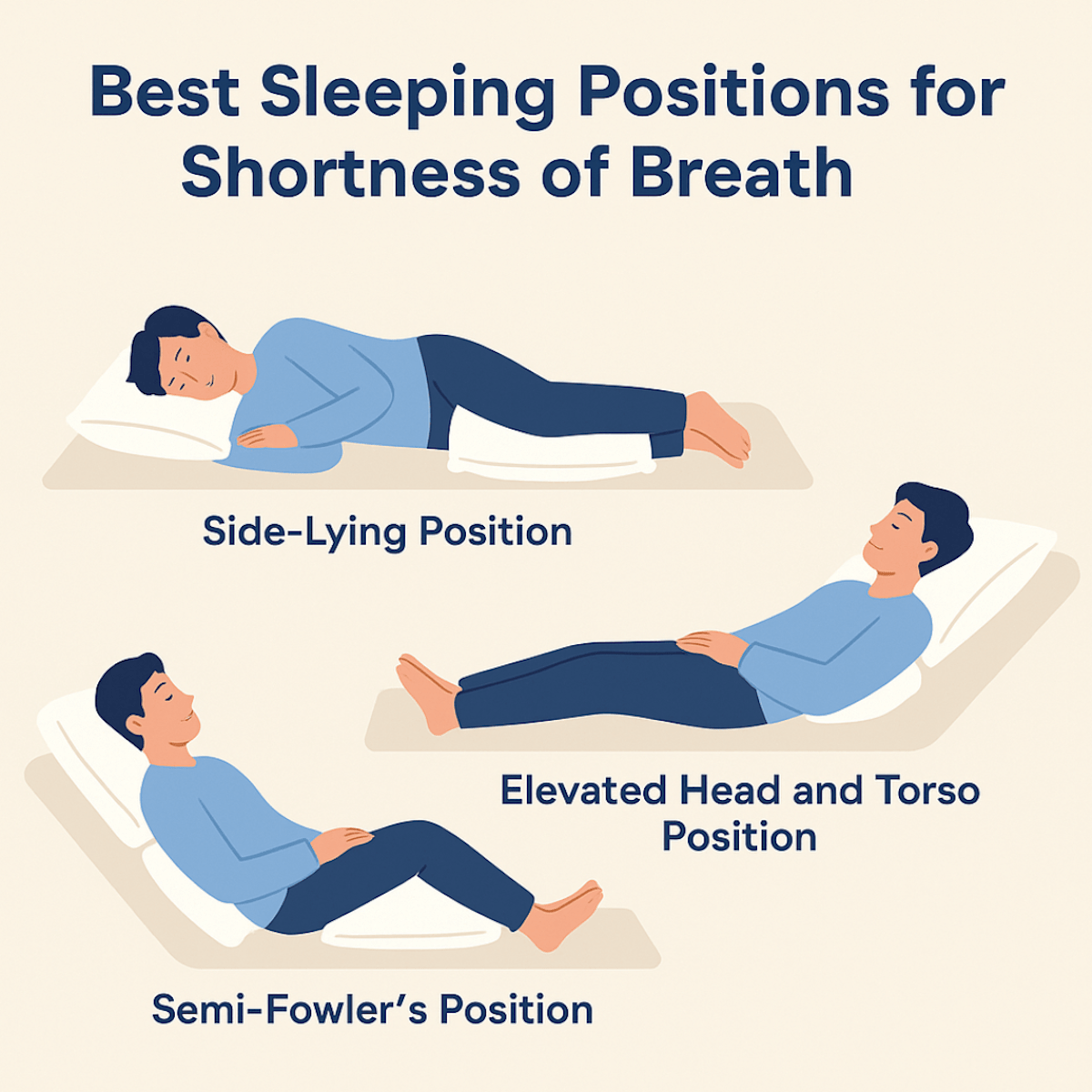
The best sleeping position for shortness of breath is typically one that promotes open airways and reduces pressure on the lungs and diaphragm. The semi-Fowler’s position, where the head and torso are elevated at a 30 to 45-degree angle, is often recommended. This position uses gravity to ease breathing and prevent fluid from pooling in the lungs.
Side-lying, particularly on the left side, can also help reduce pressure on the chest and improve airflow. These positions are especially helpful for individuals with conditions like COPD, heart failure, or sleep apnea.
Note: Avoid lying flat on your back, as this can worsen symptoms by compressing the lungs or obstructing the airway. Always consult a healthcare provider for personalized advice.
Understanding Shortness of Breath During Sleep
Shortness of breath at night disrupts rest, reduces sleep quality, and may signal underlying health conditions. Sleep position, medical history, and certain symptoms should be carefully considered to ensure proper care and comfort.
Common Causes of Nighttime Breathlessness
Nighttime breathlessness, known as nocturnal dyspnea, can result from several underlying conditions. Congestive heart failure is a common contributor, causing fluid buildup in the lungs when lying down. Asthma and chronic obstructive pulmonary disease (COPD) may also trigger or worsen breathing trouble at night.
Obstructive sleep apnea is another frequent cause, where the airways collapse during sleep. Allergies, GERD (gastroesophageal reflux disease), and obesity can further aggravate symptoms. Recognizing the specific cause can help direct the proper management and improve nighttime breathing.
How Sleep Position Impacts Breathing
The way a person positions their body during sleep can have a direct effect on their ability to breathe comfortably. Lying flat on the back may cause the tongue and soft tissues in the throat to obstruct the airway, especially for people with sleep apnea or obesity.
Sleeping on the left side can reduce pressure on the heart and improve lung function in some individuals. Elevating the upper body with extra pillows may help minimize fluid buildup in the lungs. For those with respiratory issues, experimenting with head and body angles can provide noticeable improvement in nighttime breathing.
Recognizing When to Seek Medical Advice
Frequent or severe shortness of breath during sleep should not be ignored. Warning signs include waking up gasping for air, persistent coughing, or experiencing chest pain at night. Blue-tinged lips, confusion, or a rapid heartbeat can signal a medical emergency and require immediate attention.
A healthcare provider should be consulted if symptoms disrupt sleep multiple times per week. Existing heart or lung problems can increase the risk, making it important to discuss any changes openly with a doctor. Prompt medical advice can help diagnose the cause and prevent complications.
Best Sleeping Positions for Shortness of Breath
Sleeping posture can impact airflow, chest expansion, and oxygen intake overnight. Adjusting body alignment supports better breathing for people with shortness of breath.
Side-Lying Position Benefits
Resting on the side, especially the left, can help keep airways open. This position may reduce the risk of the tongue or soft palate collapsing toward the throat at night, supporting a clearer pathway for air.
Side-lying can be particularly effective for people with obstructive sleep apnea and those who snore. Placing a pillow between the knees helps align the spine and relieve lower back strain, making it easier to maintain the position through the night.
Those with heart failure or acid reflux may also prefer this posture, as it can decrease pressure on the lungs and improve comfort. Using a supportive pillow under the head keeps the neck neutral, further aiding breathing.
Elevated Head and Torso Position
Raising the head and torso with pillows or an adjustable bed elevates the upper body above the horizontal level. This position uses gravity to prevent fluid from pooling in the chest, which can ease breathing for those with congestive heart failure or lung conditions.
Sleeping at a gentle incline can also reduce nasal congestion. By using extra pillows or a wedge pillow, the shoulders and back receive support, minimizing strain on the neck and spine.
People should avoid steep angles, which may cause discomfort or sliding off the bed. An incline of 30 to 45 degrees is typically recommended for effective support without significant discomfort.
Semi-Fowler’s Position for Comfort
The Semi-Fowler’s position involves lying on the back with the head and torso elevated to between 30 and 45 degrees, often with knees slightly bent. Hospitals use this position for patients with breathing issues, as it helps lung expansion and reduces pressure on the diaphragm.
With a few supportive pillows at the head, neck, and under the knees, users can achieve this position at home. The Semi-Fowler’s position can ease symptoms of chronic obstructive pulmonary disease (COPD) or other lung restrictions.
Maintaining this posture helps prevent the collapse of the upper airway during sleep. Care should be taken to adjust pillow placement for comfort and to reduce muscle strain.
Positions to Avoid With Shortness of Breath
Certain sleeping positions can increase breathing difficulty, especially for individuals with respiratory concerns. It is important to recognize which positions tend to worsen symptoms due to gravity, airway mechanics, or pressure on the chest and lungs.
Risks of Sleeping Flat on Your Back
Lying flat on the back, or the supine position, can allow gravity to cause the tongue and soft tissues of the throat to partially block the airway. This is particularly common in people who snore, have sleep apnea, or suffer from obesity. For those with shortness of breath, back sleeping may lead to increased airway resistance and less expansion of the lungs.
Fluid can also accumulate at the back of the throat or in the lungs when on the back, worsening symptoms in people with conditions like heart failure or pulmonary disease. This position may also increase the risk of nighttime coughing or choking sensations, disrupting sleep and overall comfort.
Drawbacks of Prone (Stomach) Sleeping
Stomach sleeping places additional pressure on the chest and abdominal area. This pressure can make it harder for the lungs to fully expand, limiting the amount of oxygen the body receives during sleep. Individuals with shortness of breath may notice more frequent awakenings or shallow breathing in this position.
The neck and spine may also be strained, leading to muscle discomfort and poor quality sleep. Stomach sleeping may force the head and neck to turn sharply to one side, further restricting airflow through the windpipe. For these reasons, prone sleeping is generally not advised for those with difficulties breathing at night.
Tips for Adjusting Your Sleep Environment
A well-planned sleep environment can play a critical role in reducing shortness of breath at night. Key factors include pillow support, mattress type, and maintaining optimal air quality and humidity.
Choosing Supportive Pillows
The right pillow setup can help promote open airways and minimize effort when breathing. People with breathing issues often benefit from wedge-shaped pillows or stacking two firm pillows to keep the upper body elevated. This semi-upright position can decrease pressure on the lungs and airway.
It is important to avoid pillows that are too high or too stiff, as they may strain the neck. Memory foam pillows that contour to the head and neck provide consistent support and alignment. For those who sleep on their side, using a body pillow can also maintain alignment and prevent rolling onto the back, which sometimes worsens symptoms.
Pillow covers made from hypoallergenic materials help reduce allergens and dust mites, which can irritate breathing. Wash pillowcases and covers weekly in hot water to further limit exposure to triggers.
Mattress Recommendations
Selecting a mattress that offers both firmness and support can help keep the spine and torso well-positioned. Inadequate mattress support can lead to slouching or twisting, which may compress the chest and restrict airflow.
Medium-firm mattresses are often recommended because they provide enough support to keep the body aligned, yet have enough cushioning for comfort. Mattresses made from memory foam or latex tend to offer excellent contouring while minimizing pressure points. It is helpful to avoid old or sagging mattresses, which can make it harder to find a comfortable breathing position.
For added height and ease of adjustment, some people benefit from an adjustable bed frame. Raising the head of the bed several inches allows for customized elevation, helpful for those with chronic shortness of breath or reflux at night.
Bedroom Air Quality and Humidity
Maintaining clean air in the bedroom can reduce respiratory irritation. Regularly use an air purifier with a HEPA filter to trap dust, pollen, and allergens. Keep windows closed if outdoor air quality is poor, especially during allergy seasons or high pollution days.
Humidity levels should be kept between 30% and 50%. Air that is too dry can cause airways to become irritated, while excess moisture can promote mold and dust mites. Use a hygrometer to monitor humidity and operate a humidifier or dehumidifier as needed.
Remove sources of dust collection, such as heavy drapes, stuffed animals, or unnecessary carpeting, to limit allergens in the sleeping area. Clean the bedroom regularly and wash bedding in hot water to reduce buildup of irritants that can trigger shortness of breath.
Positioning Strategies for Specific Conditions
Different health conditions can affect breathing in unique ways during sleep. Adjusting body position can support airway openness, lung efficiency, and heart function depending on the underlying issue.
Optimizing Sleep for Asthma
People with asthma often benefit from sleeping on their back with the upper body slightly elevated using pillows or a wedge. This reduces airway resistance and helps keep nasal passages open, which can lessen nighttime asthma symptoms.
Side sleeping may also help, but stomach sleeping is discouraged as it can compress the chest. Using hypoallergenic bedding can minimize triggers like dust mites. It’s important to keep the bedroom environment clean, and pillows should be supportive but not overly thick, as too much elevation can strain the neck.
Avoid sleeping completely flat, since this position can increase postnasal drip and worsen asthma symptoms. Consistency with these strategies can help improve nighttime breathing and reduce awakenings related to shortness of breath.
COPD-Focused Positioning
For people with chronic obstructive pulmonary disease (COPD), positioning strategies aim to maximize lung expansion and ease diaphragm movement. Sleeping on the side with a pillow between the knees often provides relief. This posture helps align the spine and keeps the airway unobstructed.
Some individuals find it helpful to sleep in a semi-upright position, such as with the head and torso propped up using several pillows. This can reduce pressure on the lungs and minimize the risk of fluid buildup.
It is important to avoid sleeping on the stomach, as this position can restrict chest movement and make breathing harder. Keeping a consistent routine and using the right support can make a noticeable difference for those with COPD.
Congestive Heart Failure Adaptations
Congestive heart failure often leads to fluid buildup and increased shortness of breath when lying flat. Elevating the head and upper body by 30 to 45 degrees with pillows or a wedge can decrease pressure on the lungs and heart, making breathing easier during sleep.
Sleeping on the left side is sometimes preferred, as it may reduce pressure on the heart. However, people should avoid lying completely flat or on the right side if it worsens symptoms.
Using extra pillows under the knees can also help to keep the body in a comfortable, partially reclined position. Elevated sleeping positions can lower fluid accumulation in the lungs, relieve discomfort, and support restful sleep for individuals living with heart failure.
Practical Steps to Reduce Nighttime Breathlessness
Managing shortness of breath at night often requires both physical and mental preparation. Simple strategies before bedtime can support easier breathing and contribute to better sleep quality.
Breathing Exercises Before Sleep
Breathing techniques can reduce anxiety and improve oxygen flow. Pursed-lip breathing involves inhaling slowly through the nose and exhaling gently through pursed lips, helping the lungs release trapped air. Diaphragmatic breathing, or belly breathing, encourages deeper breaths by engaging the diaphragm rather than the chest.
For those unfamiliar, it may help to count to four while inhaling, pause, then slowly exhale to a count of six or eight. Practicing these exercises for five to ten minutes before lying down can ease the sensation of tightness in the chest.
Maintaining a semi-upright sitting posture while practicing can further support lung expansion. Individuals with chronic respiratory conditions often find regular practice of these techniques most beneficial.
Establishing a Relaxing Bedtime Routine
A consistent routine helps signal the body that it’s time to wind down, reducing both stress and physical symptoms of breathlessness. Activities such as reading, gentle stretching, or listening to calm music can lower tension and heart rate.
Avoid caffeine, large meals, and strenuous activities at least two hours before bed. Keeping the bedroom cool and free from strong odors may also contribute to easier nighttime breathing.
Using an extra pillow to prop up the head and chest can help airways stay open. Light, loose-fitting pajamas can prevent overheating, which may aggravate breathing difficulties at night.
Special Considerations for Pregnant Individuals
Pregnant individuals may notice increased shortness of breath, especially as pregnancy progresses. The growing uterus can push up against the diaphragm, reducing lung capacity and making breathing feel more difficult.
Side-sleeping, especially on the left side, is often recommended. This position can help maximize blood flow and reduce pressure on major blood vessels and organs. It also may alleviate some of the pressure that makes breathing harder while lying on the back.
Avoiding the supine (flat-back) position is generally advised after the first trimester. Lying flat can place extra pressure on the vena cava, a major vein, further restricting blood flow and worsening breathlessness.
Using pillows for support can provide added comfort. For example, placing a pillow between the knees or behind the back can maintain proper alignment and reduce strain. Many find that raising the upper body slightly with a wedge pillow can improve breathing comfort.
Wearing loose sleepwear, keeping the sleeping environment cool, and practicing gentle breathing exercises before bed can help make rest easier. If symptoms of shortness of breath are persistent or severe, it is important to consult a healthcare provider.
Sleep Position Aids and Devices
Devices such as wedge pillows and adjustable beds help maintain comfortable sleeping angles. Positional therapy tools can make it easier to breathe by supporting the body and promoting healthier airflow during rest.
Wedge Pillows and Adjustable Beds
Wedge pillows elevate the upper body at a gentle incline, which can prevent the diaphragm from being compressed during sleep. This position can reduce the pooling of fluids and make breathing smoother. Wedge pillows also suit people who find flat sleeping uncomfortable due to shortness of breath.
Adjustable beds allow for custom elevation using a remote or manual controls. Raising just the head or both the head and legs can relieve pressure on the chest and lungs. Many models also come with extra features such as memory foam and adjustable firmness.
Sleeping with an elevated torso is especially helpful for individuals with conditions like heart failure or chronic obstructive pulmonary disease (COPD). It can minimize the risk of waking up due to breathlessness.
Benefits of Positional Therapy Devices
Positional therapy devices help maintain specific sleeping positions throughout the night. Some devices are worn around the waist or back to prevent rolling onto the back, which can worsen shortness of breath.
These devices are lightweight and do not restrict movement fully, allowing users to adjust without losing support. They serve as physical reminders to stay in preferred sleeping positions and can be helpful for those who move unconsciously during sleep.
Using positional therapy devices may also reduce snoring and sleep interruptions by keeping airways open. They are commonly recommended by sleep specialists for people who do not respond well to pillows or beds alone.
FAQs About Sleep and Shortness of Breath
Can Sleeping Position Cause Shortness of Breath?
Yes, your sleeping position can contribute to shortness of breath, especially if you lie flat on your back. This posture can cause your tongue and soft tissues to collapse backward, narrowing the airway.
In people with conditions like COPD, heart failure, or sleep apnea, lying flat can make breathing more difficult. Elevating your upper body or sleeping on your side can often improve airflow and reduce the feeling of breathlessness during sleep.
Can You Sleep With Shortness of Breath?
It is possible to sleep with shortness of breath, but it can be challenging. Finding the right sleeping position and using pillows to support the upper body can help ease breathing. For some individuals, sleeping in a reclined or upright position—such as in a recliner or with an adjustable bed—may be more comfortable.
Note: Persistent shortness of breath during sleep may signal an underlying condition, so it’s important to consult a healthcare provider for evaluation and treatment.
How Should I Sleep With Shortness of Breath?
Sleeping with shortness of breath often requires adjustments in position to open the airway and reduce pressure on the chest. The most recommended methods include sleeping on your side with a pillow between your legs or propping yourself up with pillows to elevate the upper body.
These positions can help reduce fluid buildup in the lungs and improve breathing. Avoid lying completely flat, as this can worsen symptoms, especially for those with respiratory or cardiac conditions.
Does Lying Down Help With Shortness of Breath?
Lying down flat can sometimes worsen shortness of breath, particularly in people with heart or lung issues. This position may lead to fluid shifting or airway collapse, making it harder to breathe. However, lying on your side or in an elevated position can help alleviate symptoms.
Note: If you frequently feel short of breath when lying down, it may be a sign of an underlying condition such as orthopnea or heart failure, and you should seek medical advice.
What Is The Best Position To Sleep In To Clear Your Lungs?
The best position to help clear your lungs is lying on your side with your head and upper body slightly elevated. This posture encourages better lung expansion and drainage of secretions, especially when combined with deep breathing techniques.
Some individuals also benefit from prone (stomach) positioning, which has been used in hospitals for lung improvement. Proper positioning can help reduce mucus buildup and make breathing easier, particularly for people with lung conditions like pneumonia or COPD.
What Is The Best Position To Sleep In To Stop Mouth Breathing?
Sleeping on your side with your head slightly elevated is often the best position to reduce mouth breathing. This helps maintain an open nasal passage and can discourage the jaw from falling open.
Using a supportive pillow and keeping the head in a neutral position may also help. In some cases, a chin strap or nasal breathing aids may be necessary. Mouth breathing during sleep can be a sign of nasal congestion or sleep apnea, so further evaluation might be needed.
Final Thoughts
Finding the right sleeping position can be a game-changer for anyone dealing with shortness of breath. Whether you prefer lying on your side with pillows for support or elevating your upper body to ease lung function, small adjustments in how you sleep can lead to noticeable improvements in breathing comfort.
Always listen to your body and consult with a healthcare provider if breathing difficulties persist. With the right approach, you can breathe easier and sleep more soundly.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Zhang Y, Xiao A, Zheng T, Xiao H, Huang R. The Relationship between Sleeping Position and Sleep Quality: A Flexible Sensor-Based Study. Sensors (Basel). 2022.
- Oksenberg A, Silverberg DS. The effect of body posture on sleep-related breathing disorders: facts and therapeutic implications. Sleep Med Rev. 1998.
- Menon A, Kumar M. Influence of body position on severity of obstructive sleep apnea: a systematic review. ISRN Otolaryngol. 2013.
- Lee JB, Park YH, Hong JH, Lee SH, Jung KH, Kim JH, Yi H, Shin C. Determining optimal sleep position in patients with positional sleep-disordered breathing using response surface analysis. J Sleep Res. 2009.