Pulmonary agenesis represents one of the most severe congenital malformations of the respiratory system, characterized by the complete absence of one or both lungs along with their corresponding bronchi and pulmonary vessels.
This rare developmental anomaly occurs during embryonic life when the lung bud fails to develop properly, resulting in a spectrum of abnormalities ranging from complete absence of lung tissue to partial developmental arrest.
Understanding pulmonary agenesis is crucial for healthcare providers, as early recognition and appropriate management can significantly impact patient outcomes and quality of life.
Download our free guide that has over 100+ of the best tips for healthy lungs.
What is Pulmonary Agenesis?
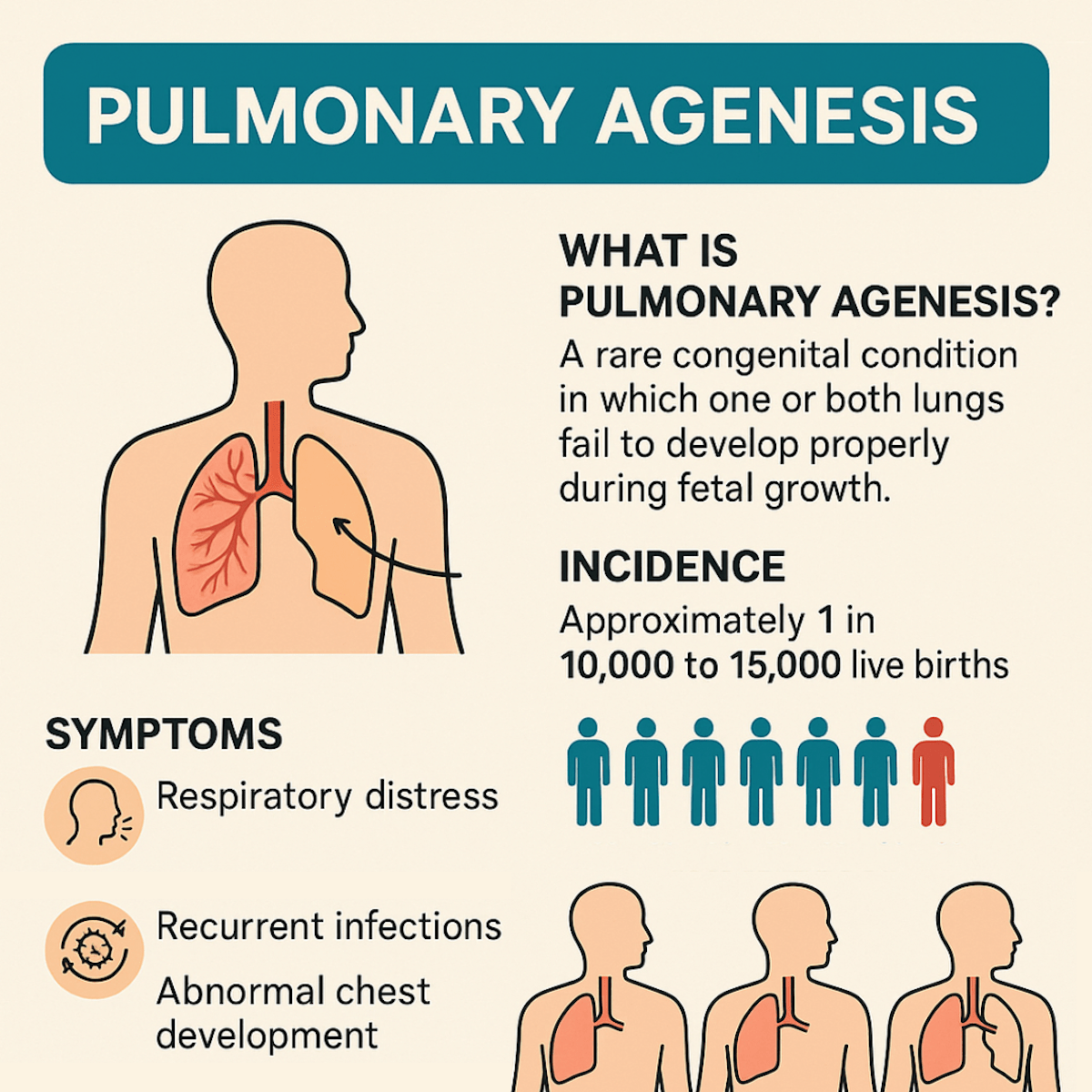
Pulmonary agenesis is a rare congenital condition in which one or both lungs fail to develop properly during fetal growth. In complete pulmonary agenesis, the lung tissue, bronchial tree, and pulmonary vasculature are entirely absent on the affected side. It most commonly affects only one lung (unilateral), with the right side being less common but more severe due to the heart’s position and vascular implications.
Symptoms vary depending on the extent of the defect but may include respiratory distress, recurrent infections, and abnormal chest development. Diagnosis is typically made through imaging studies such as CT or MRI. There is no cure, but treatment focuses on supportive care.
Embryological Development and Pathogenesis
During normal embryonic development, the respiratory system begins to form around the fourth week of gestation. The lung buds emerge from the ventral aspect of the foregut endoderm and subsequently undergo a complex process of branching morphogenesis. In pulmonary agenesis, this developmental process is disrupted at its earliest stages.
The pathogenesis involves failure of the primitive lung bud to develop or premature arrest of lung development. Several key developmental pathways are implicated, including the Sonic hedgehog (Shh) signaling pathway, fibroblast growth factor (FGF) signaling, and bone morphogenetic protein (BMP) pathways. These molecular mechanisms are essential for proper lung bud formation, branching, and vascular development.
The timing of the developmental arrest determines the extent of the malformation. If the arrest occurs very early, complete agenesis results, while later arrests may lead to varying degrees of hypoplasia or dysplasia. The condition can be unilateral or bilateral, with bilateral agenesis being incompatible with life.
Classification and Types
Pulmonary agenesis is classified into three main categories based on the extent of developmental arrest:
- Type I (Complete Agenesis): This represents the most severe form, characterized by the complete absence of the lung, bronchus, and pulmonary vessels on the affected side. The main bronchus is entirely absent, and no respiratory tissue is present.
- Type II (Agenesis with Rudimentary Bronchus): In this form, a rudimentary main bronchus is present but ends blindly without any associated lung tissue or alveolar development. The bronchus may be variable in length but contains no functional respiratory elements.
- Type III (Aplasia): This category involves the presence of a rudimentary bronchus with some primitive lung tissue, but the tissue is non-functional and severely underdeveloped. Some vascular elements may be present, but are typically abnormal.
Note: Unilateral pulmonary agenesis is more common than bilateral disease, with right-sided agenesis being slightly more frequent than left-sided involvement. The laterality can influence the clinical presentation and associated anomalies.
Clinical Presentation and Symptoms
The clinical manifestations of pulmonary agenesis vary significantly depending on the extent of the malformation, the presence of associated anomalies, and the patient’s age at presentation. Many cases are now diagnosed prenatally through advanced imaging techniques, but some may not be recognized until later in life.
- Neonatal Presentation: Newborns with pulmonary agenesis may present with respiratory distress, cyanosis, and feeding difficulties. The severity of symptoms often correlates with the degree of mediastinal shift and compression of the remaining lung. Some infants may appear relatively asymptomatic initially, particularly if the remaining lung compensates adequately.
- Pediatric Presentation: Children may present with recurrent respiratory infections, exercise intolerance, chest pain, or failure to thrive. The diagnosis is sometimes made incidentally during imaging for other conditions. Growth retardation may occur due to chronic respiratory insufficiency.
- Adult Presentation: Adults with previously undiagnosed pulmonary agenesis may present with dyspnea, reduced exercise tolerance, or complications related to the anatomical abnormalities. Some cases are discovered incidentally during routine chest imaging.
- Physical Examination Findings: Physical examination typically reveals decreased chest expansion on the affected side, absent breath sounds, and dullness to percussion. The mediastinum is shifted toward the affected side, and the remaining lung may demonstrate compensatory hyperexpansion. Cardiac examination may reveal displacement of heart sounds due to mediastinal shift.
Associated Anomalies and Syndromes
Pulmonary agenesis is frequently associated with other congenital anomalies, occurring as isolated defects in only about 50% of cases. The presence of associated anomalies significantly impacts the prognosis and management approach.
- Cardiovascular Anomalies: Congenital heart defects are among the most common associated abnormalities, occurring in approximately 50-60% of patients. These may include ventricular septal defects, atrial septal defects, patent ductus arteriosus, tetralogy of Fallot, and complex cyanotic heart disease. The combination of pulmonary agenesis with significant cardiac anomalies substantially increases morbidity and mortality.
- Skeletal Anomalies: Vertebral defects, rib abnormalities, and scoliosis are frequently observed. The VACTERL association (Vertebral defects, Anal atresia, Cardiac defects, Tracheo-esophageal fistula, Renal abnormalities, and Limb defects) is particularly relevant, as pulmonary agenesis can occur as part of this spectrum.
- Genitourinary Anomalies: Renal abnormalities, including renal agenesis, horseshoe kidney, and urogenital malformations, are commonly associated with pulmonary agenesis. These associations reflect the common developmental origins of these organ systems.
- Gastrointestinal Anomalies: Tracheoesophageal fistula, esophageal atresia, and other gastrointestinal malformations may occur concurrently. These anomalies can complicate the clinical presentation and management.
- Neurological Anomalies: Central nervous system malformations, including neural tube defects and brain malformations, have been reported in association with pulmonary agenesis.
Diagnostic Approach
The diagnosis of pulmonary agenesis requires a comprehensive imaging approach, often supplemented by additional diagnostic studies to evaluate associated anomalies and functional capacity.
- Prenatal Diagnosis: Advances in prenatal imaging, particularly fetal magnetic resonance imaging (MRI), have enabled earlier detection of pulmonary agenesis. Prenatal ultrasound may show mediastinal shift, cardiac displacement, and absent lung tissue. Fetal MRI provides superior soft tissue contrast and can better delineate the extent of the malformation.
- Postnatal Imaging: Chest radiography typically shows complete opacification of the affected hemithorax with mediastinal shift toward the affected side. The remaining lung demonstrates compensatory hyperexpansion. However, chest X-rays alone may not definitively distinguish between agenesis and severe hypoplasia.
- Computed Tomography (CT): High-resolution CT scanning provides detailed anatomical information about the extent of the malformation, the presence of any rudimentary bronchial structures, and the degree of mediastinal shift. CT angiography can evaluate the pulmonary vascular anatomy and identify associated vascular anomalies.
- Magnetic Resonance Imaging (MRI): MRI offers excellent soft tissue contrast and can provide detailed information about the mediastinal anatomy, cardiovascular structures, and any associated anomalies. MRI is particularly useful for evaluating the heart and great vessels when cardiac anomalies are suspected.
- Bronchoscopy: Flexible bronchoscopy can directly visualize the tracheobronchial tree and confirm the absence of the main bronchus on the affected side. This procedure is particularly useful for distinguishing between complete agenesis and cases with rudimentary bronchial structures.
- Echocardiography: Given the high frequency of associated cardiac anomalies, comprehensive echocardiographic evaluation is essential in all patients with pulmonary agenesis. This assessment helps identify structural heart defects and evaluate cardiac function.
- Pulmonary Function Testing: In older children and adults, pulmonary function testing can assess the functional capacity of the remaining lung and guide management decisions. These studies typically show reduced total lung capacity and may demonstrate airflow limitations.
Management and Treatment
The management of pulmonary agenesis is primarily supportive and aimed at optimizing the function of the remaining lung while addressing associated anomalies and complications. There is no surgical intervention that can restore the absent lung, so treatment focuses on maximizing respiratory function and preventing complications.
- Respiratory Management: The cornerstone of management involves optimizing respiratory function through various strategies. Chest physiotherapy, including postural drainage and percussion, helps prevent secretion retention and reduces the risk of respiratory infections. Bronchodilators may be beneficial in patients with reactive airway disease or bronchospasm.
- Infection Prevention: Patients with pulmonary agenesis are at increased risk for respiratory infections due to altered pulmonary mechanics and potential for secretion retention. Vaccination against respiratory pathogens, including influenza and pneumococcal disease, is essential. Prompt treatment of respiratory infections with appropriate antibiotics is crucial.
- Cardiac Management: When associated cardiac anomalies are present, appropriate cardiac intervention may be necessary. This may include surgical correction of structural defects or medical management of heart failure. The timing and approach to cardiac interventions must be carefully coordinated with the patient’s overall respiratory status.
- Nutritional Support: Adequate nutrition is essential for optimal growth and development, particularly in children with pulmonary agenesis. Nutritional assessment and support may be necessary to ensure adequate caloric intake and growth velocity.
- Exercise and Activity Modification: While patients should be encouraged to maintain an active lifestyle, activities may need to be modified based on individual tolerance and respiratory capacity. Supervised exercise programs can help optimize cardiovascular fitness within the constraints of the condition.
- Surgical Considerations: In rare cases, surgical intervention may be considered for specific complications. For example, if severe scoliosis develops and threatens respiratory function, spinal fusion may be necessary. However, any surgical intervention must be carefully evaluated considering the patient’s limited respiratory reserve.
Prognosis and Long-term Outcomes
The prognosis for patients with pulmonary agenesis varies significantly based on several factors, including the presence and severity of associated anomalies, the degree of mediastinal shift, and the functional capacity of the remaining lung.
- Factors Affecting Prognosis: The most significant prognostic factor is the presence of associated anomalies, particularly complex cardiac defects. Patients with isolated pulmonary agenesis generally have a better prognosis than those with multiple system involvement. The degree of mediastinal shift and compression of the remaining lung also influences outcomes.
- Survival Rates: Historical data suggest that patients with isolated unilateral pulmonary agenesis have survival rates approaching 70-80%, while those with significant associated anomalies have considerably lower survival rates. Early diagnosis and appropriate management have improved outcomes in recent decades.
- Long-term Complications: Patients who survive to adulthood may experience various long-term complications, including exercise intolerance, recurrent respiratory infections, and potential cardiac complications related to chronic changes in pulmonary circulation. Progressive scoliosis may develop and require monitoring.
- Quality of Life: Many patients with pulmonary agenesis can achieve a reasonable quality of life with appropriate management. However, activity limitations and the need for ongoing medical care may impact overall well-being. Psychological support and counseling may be beneficial for patients and families.
- Reproductive Considerations: Adults with pulmonary agenesis who are considering pregnancy require careful counseling and monitoring, as the increased metabolic demands of pregnancy may exceed the functional capacity of a single lung.
Differential Diagnosis
Several conditions may present with similar clinical and radiological features to pulmonary agenesis, making accurate diagnosis challenging in some cases.
- Severe Pulmonary Hypoplasia: This condition involves underdevelopment of the lung with some residual lung tissue present. Unlike agenesis, hypoplastic lungs retain some bronchial and vascular structures, which can be identified on advanced imaging.
- Congenital Diaphragmatic Hernia: Large diaphragmatic hernias can cause severe mediastinal shift and may be confused with pulmonary agenesis on initial chest radiography. CT or MRI can differentiate these conditions by identifying herniated abdominal contents.
- Massive Pleural Effusion: Extensive pleural fluid accumulation can cause complete opacification of a hemithorax with mediastinal shift. However, the clinical history and response to thoracentesis help distinguish this from agenesis.
- Extensive Pulmonary Consolidation: Severe pneumonia or other infectious processes can cause complete opacification of a lung. The acute clinical presentation and response to treatment differentiate these conditions from agenesis.
- Pulmonary Sequestration: Large pulmonary sequestrations may present with mediastinal shift, but imaging typically reveals the presence of lung tissue with anomalous blood supply rather than complete absence of the lung.
Current Research and Future Directions
Research into pulmonary agenesis continues to focus on understanding the molecular mechanisms underlying normal lung development and the factors that lead to developmental arrest. Several areas of investigation hold promise for improving outcomes and potentially developing new therapeutic approaches.
- Molecular Biology and Genetics: Ongoing research is identifying specific genetic mutations and molecular pathways involved in lung development disorders. Understanding these mechanisms may lead to targeted therapeutic interventions or genetic counseling approaches.
- Stem Cell Therapy: Experimental approaches using stem cells to regenerate lung tissue are being investigated. While still in early stages, these approaches may eventually offer therapeutic options for patients with severe lung developmental anomalies.
- Tissue Engineering: Advances in bioengineering and tissue engineering may eventually allow for the creation of artificial lung tissue or scaffolds that could support lung regeneration. These approaches remain experimental but represent potential future therapeutic options.
- Prenatal Intervention: Research into fetal interventions for severe lung developmental anomalies continues, although current approaches remain limited. Future advances may enable prenatal treatments that could improve outcomes.
- Improved Diagnostic Techniques: Continued refinement of imaging techniques and the development of new diagnostic modalities may enable earlier and more accurate diagnosis of pulmonary agenesis and associated anomalies.
Final Thoughts
Pulmonary agenesis remains a rare but clinically significant congenital anomaly that requires specialized multidisciplinary care throughout the patient’s life. While the condition cannot be cured, appropriate management can significantly improve outcomes and quality of life for affected individuals.
Early diagnosis, comprehensive evaluation for associated anomalies, and coordinated care by specialists in pediatric pulmonology, cardiology, and other relevant disciplines are essential for optimal outcomes. The prognosis depends largely on the presence and severity of associated anomalies, with isolated pulmonary agenesis generally having a more favorable outlook.
Continued research into the molecular mechanisms of lung development and potential therapeutic interventions offers hope for improved treatments in the future. Healthcare providers caring for patients with pulmonary agenesis must remain vigilant for complications and work closely with patients and families to optimize care and support throughout the patient’s life.
The rarity of this condition makes it essential for healthcare providers to be aware of its presentation and management principles, as early recognition and appropriate care can significantly impact patient outcomes. As our understanding of developmental biology continues to advance, new therapeutic approaches may emerge that could transform the care of patients with this challenging condition.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Fukuoka S, Yamamura K, Nagata H, Toyomura D, Nagatomo Y, Eguchi Y, Uike K, Hirata Y, Inoue H, Ochiai M, Ohga S. Clinical outcomes of pulmonary agenesis: A systematic review of the literature. Pediatr Pulmonol. 2022.