Cardiac tamponade is a medical emergency that respiratory therapists must be able to recognize quickly, even though it is primarily a cardiac condition. In acute care settings, patients with cardiac tamponade often present with severe respiratory distress, hypoxemia, and signs of shock that can easily be mistaken for primary pulmonary disease.
Because respiratory therapists are frequently involved in early patient assessment, oxygen delivery, mechanical ventilation, and emergency response, understanding cardiac tamponade is essential for timely intervention and patient survival.
What Is Cardiac Tamponade?
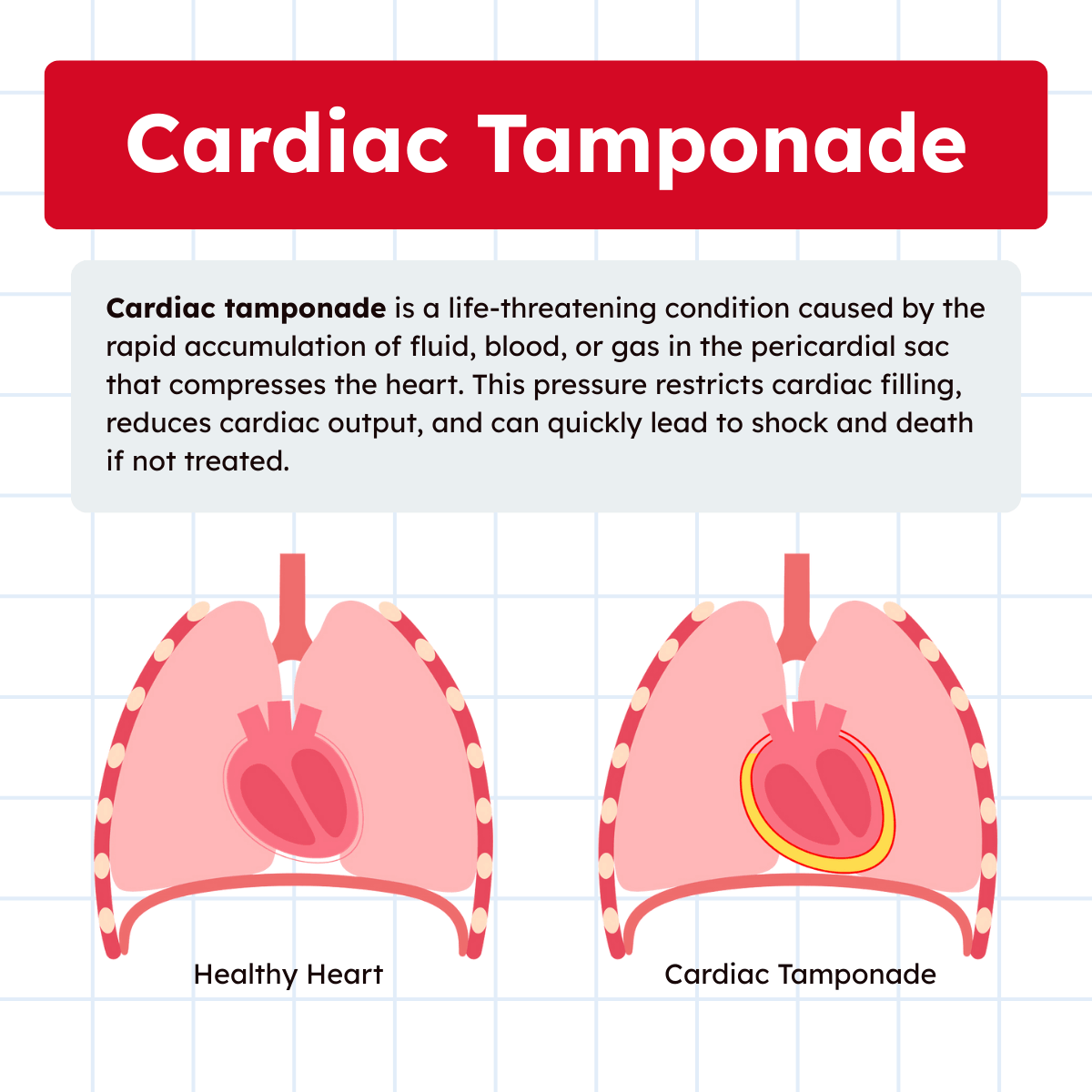
Cardiac tamponade is a life-threatening condition caused by compression of the heart due to the accumulation of blood, fluid, or gas under pressure within the pericardial sac. This increased intrapericardial pressure restricts normal cardiac filling during diastole, leading to a significant reduction in stroke volume and cardiac output.
Unlike chronic pericardial effusions, which may develop slowly and allow the pericardium to stretch, cardiac tamponade typically occurs when fluid accumulates rapidly. Even a relatively small volume can severely impair cardiac function if it builds up quickly. Without prompt recognition and treatment, cardiac tamponade can progress rapidly to shock and death.
Anatomy and Pathophysiology of the Pericardium
The heart is enclosed within the pericardium, a double-layered sac consisting of a fibrous outer layer and an inner serous pericardium. Between the two serous layers lies a thin film of pericardial fluid that reduces friction during cardiac motion.
Under normal conditions, this space contains a minimal amount of fluid. However, inflammation of the pericardium, known as pericarditis, can increase fluid production. Trauma, malignancy, infection, or post-cardiac surgery complications may also cause fluid, blood, or gas to accumulate in the pericardial space.
As intrapericardial pressure rises, the heart becomes compressed. Because the right atrium and right ventricle have thinner walls and lower pressures, they are affected first. Ventricular filling becomes impaired, venous return backs up, and systemic perfusion drops. The result is hypotension, reduced oxygen delivery to tissues, and compensatory tachycardia.
Causes of Cardiac Tamponade
Cardiac tamponade can occur in a variety of clinical settings, including:
- Pericardial effusion from infection or inflammation
- Chest trauma, including blunt or penetrating injury
- Post–cardiac surgery bleeding
- Malignancy involving the pericardium
- Uremia in patients with renal failure
- Aortic dissection
- Complications from invasive cardiac procedures
Note: From a respiratory care perspective, trauma patients, post-operative cardiac patients, and critically ill individuals are at particularly high risk and often require respiratory support during tamponade events.
Clinical Presentation and Key Signs
Patients with cardiac tamponade often present with signs of both cardiovascular collapse and respiratory distress. Common findings include:
- Hypotension
- Tachycardia
- Tachypnea
- Jugular venous distension
- Narrowed pulse pressure
- Severe dyspnea
- Anxiety and restlessness
Note: A classic combination known as Beck’s triad includes hypotension, jugular venous distension, and muffled heart sounds. While this triad is classically taught, it is not always fully present, especially in acute settings.
Jugular Venous Distension and Kussmaul Sign
Jugular venous distension (JVD) is a critical physical finding in cardiac tamponade. Normally, jugular venous pressure decreases during inspiration due to negative intrathoracic pressure drawing blood into the thorax.
In cardiac tamponade, however, the stiff, compressed heart cannot accommodate increased venous return. As a result, jugular venous pressure may paradoxically rise during inspiration, a phenomenon known as Kussmaul sign. This finding strongly suggests impaired right-sided cardiac filling and should immediately raise concern for tamponade or other obstructive cardiac conditions.
Pulsus Paradoxus and Respiratory Mechanics
One of the most important respiratory-related signs of cardiac tamponade is pulsus paradoxus, defined as an exaggerated drop in systolic blood pressure during inspiration. Although a small decrease in systolic pressure during inspiration is normal, a significant drop indicates impaired ventricular filling.
During inspiration, increased venous return to the right ventricle causes the interventricular septum to shift leftward in tamponade, further limiting left ventricular filling. This reduces stroke volume and systolic blood pressure. Pulsus paradoxus is also seen in severe airway obstruction, making differentiation critical for respiratory therapists.
Why Cardiac Tamponade Matters to Respiratory Therapists
Although cardiac tamponade is a cardiac diagnosis, respiratory therapists are often among the first clinicians to encounter these patients. Many present with acute shortness of breath, hypoxemia, or increased work of breathing, leading to early respiratory intervention.
Respiratory therapists play a vital role in:
- Recognizing abnormal breathing patterns and severe dyspnea
- Identifying signs of shock that do not improve with oxygen therapy
- Detecting pulsus paradoxus during assessment
- Noting jugular venous distension during patient positioning
- Alerting the medical team when respiratory distress is disproportionate to lung findings
Note: Importantly, positive-pressure ventilation can worsen cardiac tamponade by further reducing venous return. This makes careful ventilator management and clinical awareness essential.
Diagnostic Evaluation
The diagnostic test of choice for cardiac tamponade is echocardiography. In emergency and critical care settings, bedside echocardiography can rapidly identify pericardial effusion and signs of cardiac compression.
From a respiratory standpoint, tamponade should be considered when a patient presents with unexplained respiratory distress, hypotension, and elevated venous pressures, especially when lung sounds and imaging do not fully explain the severity of symptoms.
Other supportive findings may include:
- Low voltage on ECG
- Electrical alternans
- Chest imaging showing an enlarged cardiac silhouette
Management and Respiratory Considerations
The definitive treatment for cardiac tamponade is urgent removal of pericardial fluid, typically through pericardiocentesis or surgical drainage. This relieves pressure on the heart and restores cardiac output.
Respiratory therapists must carefully manage oxygenation and ventilation during this process. Supplemental oxygen is commonly required, but excessive positive pressure should be avoided when possible. If mechanical ventilation is necessary, the lowest effective pressures should be used to minimize further reductions in venous return.
Note: Close monitoring of respiratory status before, during, and after pericardial drainage is essential, as rapid hemodynamic changes can significantly affect gas exchange and ventilatory demand.
Cardiac Tamponade on the Board Exam
For respiratory therapy students, cardiac tamponade is a high-yield topic that frequently appears on board exams. Exam questions often focus on:
- Pulsus paradoxus
- Jugular venous distension
- Hypotension with clear lung fields
- Worsening hemodynamics after initiation of positive-pressure ventilation
- The need for echocardiography
Note: Recognizing that respiratory distress may be secondary to cardiac compression rather than lung pathology is a key exam and clinical concept.
Cardiac Tamponade Practice Questions
1. What is cardiac tamponade?
Cardiac tamponade is compression of the heart caused by the accumulation of blood, fluid, or gas under pressure within the pericardial sac.
2. What structure surrounds the heart and is involved in cardiac tamponade?
The pericardium
3. What is pericardial fluid?
A thin layer of fluid that normally separates the two layers of the serous pericardium and reduces friction during cardiac movement.
4. What condition results from inflammation of the pericardium?
Pericarditis
5. What is a pericardial effusion?
An abnormal accumulation of fluid between the layers of the pericardium.
6. How does a large pericardial effusion lead to cardiac tamponade?
Excess fluid increases intrapericardial pressure, compressing the heart and limiting ventricular filling.
7. What is the primary hemodynamic consequence of cardiac tamponade?
Reduced cardiac output due to impaired ventricular filling.
8. Why can cardiac tamponade lead to shock?
Decreased cardiac output results in inadequate systemic perfusion.
9. What classic triad is commonly associated with cardiac tamponade?
Hypotension, jugular venous distension, and muffled heart sounds.
10. What vital sign abnormality is commonly seen in cardiac tamponade?
Hypotension
11. Why does jugular venous distension occur in cardiac tamponade?
Blood backs up into the venous system due to impaired right heart filling.
12. What is pulsus paradoxus?
An exaggerated decrease in systolic blood pressure during inspiration.
13. Why does pulsus paradoxus occur in cardiac tamponade?
Inspiration further limits ventricular filling due to fixed pericardial pressure.
14. What respiratory signs may be present in cardiac tamponade?
Tachypnea and severe dyspnea.
15. How does pulse pressure typically change in cardiac tamponade?
Pulse pressure narrows.
16. What abnormal jugular venous finding may be seen during inspiration in cardiac tamponade?
An increase in jugular venous pressure known as Kussmaul sign.
17. What is jugular venous distension (JVD)?
Visible enlargement of the jugular veins more than 4 cm above the sternal angle.
18. Besides cardiac tamponade, what other conditions can cause JVD?
Right heart failure, left heart failure, tension pneumothorax, pulmonary hypertension, and mediastinal tumors.
19. Why is echocardiography important in suspected cardiac tamponade?
It can rapidly confirm pericardial effusion and assess cardiac compression.
20. What other life-threatening condition can echocardiography help rule out in emergencies?
Pulmonary embolism
21. How does cardiac tamponade affect venous return during inspiration?
Venous return is impaired, contributing to increased jugular venous pressure.
22. What heart rate abnormality is commonly seen in cardiac tamponade?
Tachycardia
23. Why does tachycardia occur in cardiac tamponade?
It is a compensatory response to reduced stroke volume.
24. Why is cardiac tamponade considered a medical emergency?
Rapid deterioration can occur, leading to shock and death if untreated.
25. What diagnostic test is most strongly recommended when cardiac tamponade is suspected?
Echocardiography
26. Why is cardiac tamponade considered especially important for respiratory therapists to recognize?
Because it often presents with respiratory distress and hypoxemia that can mimic primary pulmonary disease.
27. Why can cardiac tamponade be mistaken for a respiratory condition?
Patients frequently present with dyspnea, tachypnea, hypoxemia, and anxiety.
28. What is the underlying cause of cardiac tamponade?
Increased intrapericardial pressure that compresses the heart and restricts diastolic filling.
29. How does cardiac tamponade affect stroke volume?
Stroke volume decreases due to impaired ventricular filling.
30. How does cardiac tamponade ultimately reduce cardiac output?
Reduced ventricular filling leads to decreased stroke volume and cardiac output.
31. Why can a small amount of pericardial fluid cause tamponade if it accumulates rapidly?
The pericardium cannot stretch quickly enough to accommodate sudden fluid buildup.
32. How does acute cardiac tamponade differ from chronic pericardial effusion?
Acute tamponade occurs rapidly and causes severe hemodynamic compromise with smaller fluid volumes.
33. What layers make up the pericardium?
A fibrous outer layer and an inner serous pericardium.
34. What is the normal function of pericardial fluid?
To reduce friction between the pericardial layers during cardiac movement.
35. Which chambers of the heart are affected first in cardiac tamponade?
The right atrium and right ventricle.
36. Why are the right-sided heart chambers affected first?
They have thinner walls and operate at lower pressures.
37. How does cardiac tamponade affect venous return?
Venous return backs up due to impaired right heart filling.
38. What systemic effect results from reduced cardiac output in tamponade?
Decreased systemic perfusion leading to hypotension and shock.
39. What compensatory heart rate response occurs in cardiac tamponade?
Tachycardia
40. Why does tachycardia develop in cardiac tamponade?
To compensate for reduced stroke volume and maintain cardiac output.
41. What types of trauma can cause cardiac tamponade?
Blunt or penetrating chest trauma.
42. How can post–cardiac surgery patients develop cardiac tamponade?
From bleeding or fluid accumulation in the pericardial space.
43. Why are patients with malignancy at risk for cardiac tamponade?
Tumor involvement of the pericardium can cause fluid accumulation.
44. How does uremia contribute to cardiac tamponade?
It can cause pericardial inflammation and effusion.
45. Why is aortic dissection a potential cause of cardiac tamponade?
Blood can leak into the pericardial sac.
46. What vital sign pattern commonly suggests cardiac tamponade?
Hypotension with tachycardia.
47. Why is jugular venous distension a key sign of tamponade?
It reflects impaired right-sided cardiac filling and venous congestion.
48. Why may Beck’s triad be incomplete in acute tamponade?
Rapid onset may prevent classic signs from fully developing.
49. What is Beck’s triad?
Hypotension, jugular venous distension, and muffled heart sounds.
50. Why are muffled heart sounds heard in cardiac tamponade?
Fluid in the pericardial sac dampens sound transmission.
51. What is Kussmaul sign?
A paradoxical rise in jugular venous pressure during inspiration.
52. Why does Kussmaul sign occur in cardiac tamponade?
The heart cannot accommodate increased venous return during inspiration.
53. How does normal jugular venous pressure change during inspiration?
It decreases due to negative intrathoracic pressure.
54. What does an abnormal increase in JVP during inspiration indicate?
Impaired right ventricular filling.
55. What is pulsus paradoxus?
An exaggerated drop in systolic blood pressure during inspiration.
56. Why does pulsus paradoxus occur in cardiac tamponade?
Inspiratory septal shift further limits left ventricular filling.
57. How does inspiration affect ventricular interaction in tamponade?
Right ventricular filling compresses the left ventricle.
58. What effect does this ventricular interaction have on blood pressure?
It reduces systolic blood pressure during inspiration.
59. Why is pulsus paradoxus relevant to respiratory therapists?
It can also occur in severe airway obstruction, requiring careful differentiation.
60. What clinical finding helps differentiate tamponade from primary lung disease?
Jugular venous distension with hypotension.
61. Why is anxiety commonly seen in cardiac tamponade?
Reduced cardiac output and hypoxia stimulate sympathetic responses.
62. How does cardiac tamponade impair oxygen delivery?
Reduced cardiac output limits oxygen transport to tissues.
63. Why is cardiac tamponade considered rapidly fatal if untreated?
Progressive shock can lead to circulatory collapse and death.
64. What bedside diagnostic tool is most useful for confirming tamponade?
Echocardiography
65. Why is echocardiography critical in suspected tamponade?
It visualizes pericardial effusion and cardiac chamber compression.
66. What emergency intervention definitively treats cardiac tamponade?
Pericardial fluid drainage
67. Why must respiratory therapists remain vigilant for tamponade in ICU patients?
Critically ill patients may deteriorate quickly with overlapping respiratory symptoms.
68. How does cardiac tamponade affect mechanical ventilation decisions?
Positive pressure ventilation may further reduce venous return and worsen hypotension.
69. Why is careful assessment required before intubating a tamponade patient?
Intubation can exacerbate hemodynamic instability.
70. What is the key takeaway for respiratory therapists regarding cardiac tamponade?
Early recognition of cardiovascular causes of respiratory distress can be lifesaving.
71. Why are respiratory therapists often among the first clinicians to encounter cardiac tamponade?
Because patients frequently present with acute dyspnea, hypoxemia, and increased work of breathing.
72. Why can cardiac tamponade initially appear to be a primary respiratory problem?
Respiratory distress may be severe despite relatively clear lung sounds and imaging.
73. What respiratory assessment finding may suggest tamponade rather than lung disease?
Severe dyspnea that does not improve with oxygen therapy.
74. Why is recognizing disproportionate respiratory distress important?
It suggests a non-pulmonary cause such as impaired cardiac output.
75. What breathing pattern abnormality may be seen in cardiac tamponade?
Rapid, shallow breathing due to reduced perfusion and increased work of breathing.
76. Why should respiratory therapists assess for signs of shock in dyspneic patients?
Because shock-related hypoperfusion can cause respiratory distress independent of lung pathology.
77. How can respiratory therapists detect pulsus paradoxus at the bedside?
By observing a significant drop in systolic blood pressure during inspiration.
78. Why is pulsus paradoxus a key assessment finding for tamponade?
It reflects impaired ventricular filling during inspiration.
79. Why is jugular venous distension important to note during patient positioning?
Changes in neck vein distension may reveal impaired venous return.
80. What does persistent JVD in a dyspneic patient suggest?
Elevated central venous pressure due to cardiac compression.
81. Why should respiratory therapists alert the medical team when distress exceeds lung findings?
Because cardiac tamponade may be the underlying cause.
82. How does positive-pressure ventilation affect venous return?
It decreases venous return to the heart.
83. Why can positive-pressure ventilation worsen cardiac tamponade?
Reduced venous return further limits cardiac filling and output.
84. What ventilatory strategy should be used if mechanical ventilation is unavoidable?
Use the lowest effective airway pressures.
85. What diagnostic test is considered the gold standard for cardiac tamponade?
Echocardiography
86. Why is bedside echocardiography valuable in critical care settings?
It allows rapid identification of pericardial effusion and cardiac compression.
87. When should tamponade be suspected from a respiratory perspective?
When dyspnea, hypotension, and elevated venous pressures occur without clear lung pathology.
88. What ECG finding may support the diagnosis of cardiac tamponade?
Low voltage
89. What is electrical alternans?
Alternating amplitude of QRS complexes caused by a swinging heart within a fluid-filled pericardium.
90. What chest imaging finding may be seen in tamponade?
An enlarged cardiac silhouette.
91. What is the definitive treatment for cardiac tamponade?
Urgent removal of pericardial fluid.
92. What procedure is commonly used to remove pericardial fluid?
Pericardiocentesis
93. How does pericardial drainage improve respiratory status?
By restoring cardiac output and improving oxygen delivery.
94. Why must respiratory therapists closely monitor patients during pericardial drainage?
Rapid hemodynamic changes can alter ventilatory needs.
95. What respiratory support is commonly required before definitive treatment?
Supplemental oxygen.
96. Why should excessive airway pressures be avoided during tamponade management?
They can further reduce venous return and cardiac output.
97. What change may occur in gas exchange after successful pericardial drainage?
Improved oxygenation due to restored perfusion.
98. Why is cardiac tamponade considered a high-yield exam topic?
Because it presents with classic signs frequently tested on board exams.
99. What clue suggests cardiac tamponade rather than lung disease?
Hypotension with clear lung fields.
100. What scenario can possibly worsen tamponade findings?
The initiation of positive-pressure ventilation.
Final Thoughts
Cardiac tamponade is a critical condition that sits at the intersection of cardiology and respiratory care. Although it originates in the pericardium, its effects on breathing, oxygenation, and hemodynamics make it highly relevant to respiratory therapists.
Early recognition of abnormal respiratory patterns, pulsus paradoxus, and jugular venous distension can significantly impact patient outcomes. By understanding the pathophysiology and respiratory implications of cardiac tamponade, respiratory therapists play a vital role in early detection, appropriate intervention, and lifesaving care.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Stashko E, Meer JM. Cardiac Tamponade. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.

