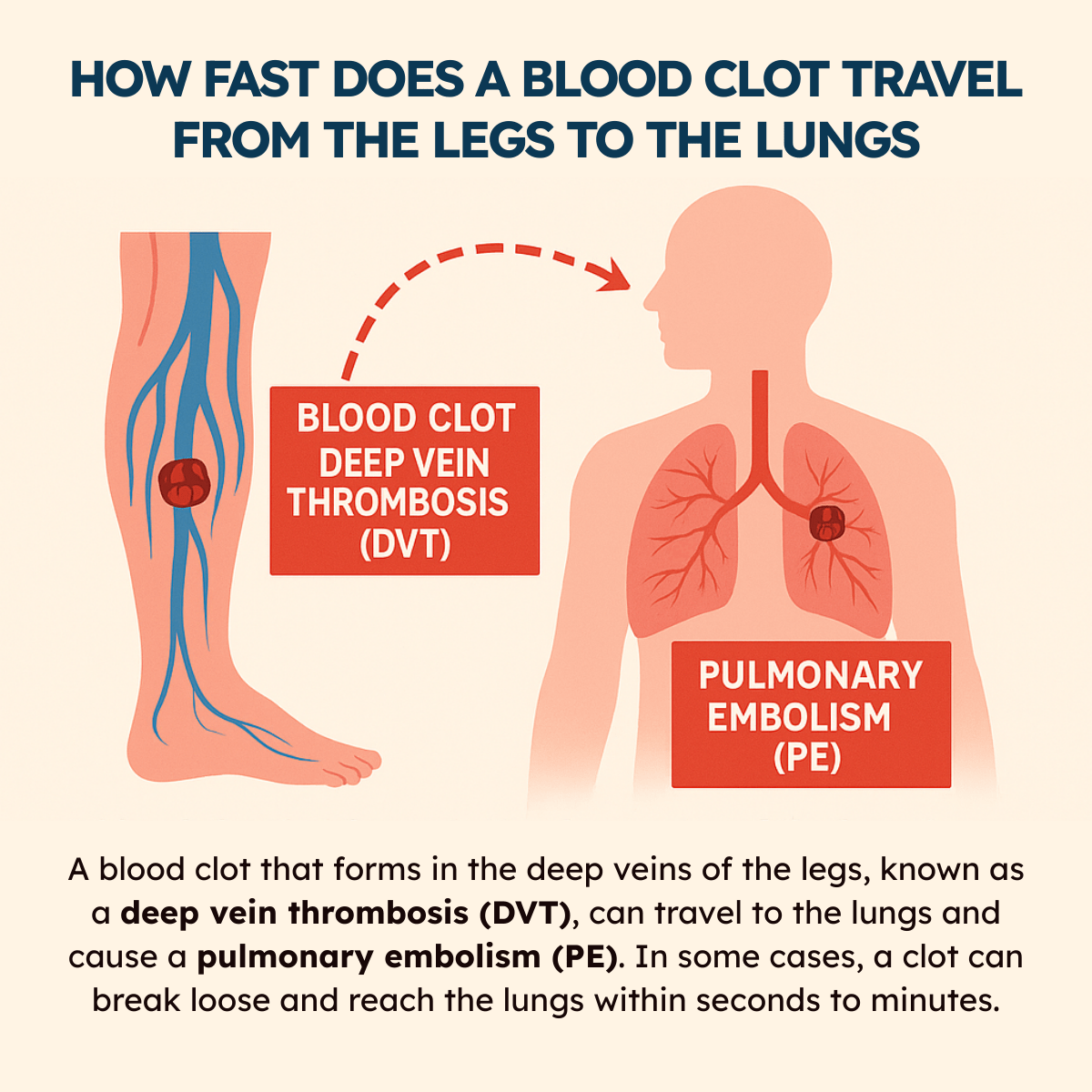
When a blood clot forms in the deep veins of the legs, a condition known as deep vein thrombosis (DVT), one of the most serious risks is that the clot can break loose and travel to the lungs, causing a pulmonary embolism (PE).
This journey from the legs to the lungs happens through the body’s circulatory system, and while it may sound like a slow process, in reality, it can occur in just seconds to minutes once the clot dislodges.
Because pulmonary embolisms can be life-threatening, understanding how quickly a clot can move, the factors that influence its travel, and the warning signs to watch for is critical for timely recognition and treatment.
Download our free guide that has over 100+ of the best tips for healthy lungs.
How Fast Does a Blood Clot Travel from the Legs to the Lungs?
A blood clot that forms in the deep veins of the legs, known as a deep vein thrombosis (DVT), can travel to the lungs and cause a pulmonary embolism (PE). The speed at which this happens varies and depends on several factors, including the size of the clot, blood flow, and the person’s activity level.
In some cases, a clot can break loose and reach the lungs within seconds to minutes, as blood is continuously circulated through the venous system to the heart and then pumped to the lungs. However, clots can also remain in the leg for days or weeks before dislodging. This unpredictability makes DVT a medical emergency that requires prompt diagnosis and treatment.
Understanding Blood Clots in the Legs
Blood clots in the legs form when blood thickens and clumps together, potentially blocking the veins. These clots can vary in type, develop due to specific risk factors, and cause distinct symptoms that signal medical attention is needed.
Types of Blood Clots
The most common type of blood clot in the legs is deep vein thrombosis (DVT). DVT occurs when a clot forms in a deep vein, usually in the calf or thigh. Superficial vein thrombosis affects veins closer to the skin and is generally less dangerous but can still cause discomfort.
Clots can be either stationary or have the potential to break free. The risk increases if the clot travels toward the lungs, causing a pulmonary embolism, which is life-threatening. Prompt diagnosis is important to prevent complications.
Risk Factors for Deep Vein Thrombosis
Several factors increase the chance of developing DVT. Prolonged immobility, such as long flights or bed rest, slows blood flow in the legs. Surgery, especially hip or knee replacement, raises the risk due to vessel injury and reduced mobility during recovery.
Other risks include obesity, smoking, pregnancy, certain cancers, and genetic clotting disorders. Age also plays a role, with the risk of developing the condition rising after the age of 60. People using hormone replacement therapy or birth control pills may face a higher chance of clot formation.
Common Symptoms
Symptoms of blood clots in the legs include swelling, usually in one leg, and localized pain or tenderness. The skin over the affected area might feel warm and appear red or discolored. Some patients report a heavy or aching sensation, especially when standing or walking.
Note: If symptoms appear suddenly or worsen quickly, it may indicate a moving clot. Immediate medical intervention is critical to prevent travel to the lungs or other complications.
Mechanisms of Blood Clot Movement
Blood clots that form in the legs can break free and move through the circulatory system due to specific physical and biological processes. The dynamics of blood flow and the structure of veins play critical roles in how these clots travel.
How Clots Detach and Travel
Blood clots, or thrombi, typically form in deep veins of the legs when blood flow slows or vessels are damaged. Clots can detach when the forces acting on them, such as muscle contractions and blood pressure, overcome the clot’s adhesion to the vessel wall.
Once detached, the clot becomes an embolus, traveling through the venous system. Its movement is affected by size and shape; larger clots may lodge earlier, while smaller ones can reach the lungs. The clot moves through the vena cava into the right heart and then into the pulmonary arteries where it can obstruct blood flow.
Role of Blood Flow and Vein Structure
Blood flow velocity in the veins affects how quickly a clot forms and moves. Venous valves, which prevent backflow, can temporarily trap clots but also create pockets where clots can form. Muscle contractions in the legs push blood upward, propelling clots forward.
Vein walls are thinner and less muscular than arteries, making them more susceptible to damage and clot formation. The structure of the venous system, including narrow areas such as the pulmonary arteries, can affect where clots become lodged, thereby impacting the severity of a pulmonary embolism.
Speed of Blood Clot Travel from Legs to Lungs
Blood clots that form in the legs can reach the lungs quickly due to the dynamics of blood flow. The time varies depending on physiological factors and the characteristics of the clot.
Average Travel Time
A blood clot originating in deep veins of the legs may reach the lungs within minutes to a few hours. The venous blood flow from the legs moves upward through large veins like the femoral and iliac veins into the inferior vena cava, then the right side of the heart, and finally to the pulmonary arteries.
Typically, travel time ranges from 1 to 30 minutes, depending largely on the clot’s size and the individual’s circulatory conditions. Small clots tend to travel faster due to less friction and resistance in the bloodstream, while larger clots may move more slowly or get lodged earlier.
Factors Influencing Speed
Several factors influence the speed of clot travel, including clot size, blood flow rate, and the individual’s cardiovascular health. Increased heart rate and higher blood pressure can accelerate the movement of clots.
Obstructions in veins, like varicose veins or vessel narrowing, may slow or stop the clot. Additionally, blood viscosity and clot composition (firmness and shape) impact how smoothly it travels. Medications such as anticoagulants can alter clot stability and indirectly influence travel speed by preventing the growth or fragmentation of clots.
Consequences of a Blood Clot Reaching the Lungs
When a blood clot travels to the lungs, it can block blood flow and put significant strain on the cardiovascular and respiratory systems. This can lead to serious complications that require immediate medical attention to prevent lasting damage or death.
Pulmonary Embolism Explained
A blood clot that reaches the lungs is called a pulmonary embolism (PE). It occurs when the clot lodges in one or more pulmonary arteries, blocking blood flow to lung tissue. The size and location of the clot determine the severity of the embolism.
PE reduces oxygen levels in the blood by preventing proper gas exchange. This forces the heart to work harder to pump blood through narrowed arteries, which can strain or damage the heart muscle. Without treatment, large or multiple clots can cause sudden cardiac arrest.
Immediate Health Risks
The most urgent risks of a pulmonary embolism include difficulty breathing, chest pain, and rapid heart rate. These symptoms reflect compromised lung function and reduced oxygen delivery.
If untreated, PE can lead to shock, where organs do not receive enough oxygen, causing failure. In severe cases, it may cause sudden death within minutes to hours after the clot reaches the lungs. Prompt diagnosis and treatment are essential to minimize these risks and improve survival chances.
Diagnosis and Detection of Migrating Blood Clots
Detecting a blood clot moving from the legs to the lungs requires precise methods. Both imaging and clinical evaluation play crucial roles in confirming the presence and risk of these clots.
Imaging Techniques
Imaging is essential for visualizing clots in veins and lungs. Doppler ultrasound is the primary tool for identifying deep vein thrombosis (DVT) in the legs. It uses sound waves to detect blood flow obstructions caused by clots.
For clots that may have traveled to the lungs, CT pulmonary angiography (CTPA) is the most accurate method. CTPA provides clear images of the pulmonary arteries and can pinpoint blockages caused by emboli.
Note: Other techniques include ventilation-perfusion (V/Q) scans, which assess mismatches in air and blood flow in the lungs. These scans are useful when CTPA is contraindicated.
Clinical Signs and Testing
Clinical evaluation involves recognizing symptoms such as leg swelling, pain, and redness, which suggest DVT. Sudden shortness of breath, chest pain, and rapid heartbeat raise suspicion of pulmonary embolism (PE).
Blood tests measuring D-dimer levels support diagnosis by indicating active clot breakdown. Elevated D-dimer can prompt further imaging but is not specific enough alone. Physicians also assess risk factors like recent surgery, immobility, or previous clots. Together, clinical signs and laboratory results guide decisions on urgent testing and treatment.
Prevention and Treatment Options
Effective management of blood clots requires both medical intervention and changes in daily habits. Combining treatments helps reduce clot formation and prevents complications like pulmonary embolism.
Medication Approaches
Anticoagulants are the primary drugs used to prevent and treat blood clots. Common medications include heparin, warfarin, and direct oral anticoagulants (DOACs) such as apixaban and rivaroxaban. These drugs work by thinning the blood to stop existing clots from growing and to prevent new clots.
Treatment duration varies but often lasts several months. In some cases, patients require long-term anticoagulation due to recurring clot risk. Monitoring is essential, especially with warfarin, to maintain therapeutic levels and avoid bleeding complications.
Thrombolytic drugs might be used in severe cases to dissolve clots rapidly. However, these carry higher bleeding risks and are reserved for life-threatening situations like massive pulmonary embolism.
Lifestyle Modifications
Physical activity is crucial in preventing blood clots. Regular walking or leg exercises improve circulation, especially during long periods of immobility like flights or bed rest. Avoiding prolonged sitting reduces venous stasis, a major clot risk factor.
Hydration supports blood flow by preventing blood thickening. Patients are advised to drink enough fluids daily. Additionally, weight management and smoking cessation lower clot risks by improving vascular health.
Compression stockings can be beneficial for people prone to deep vein thrombosis. They help maintain venous pressure and prevent pooling of blood in the legs. These stockings are often recommended after clot diagnosis or for those with limited mobility.
Complications and Long-Term Effects
Blood clots traveling from the legs to the lungs can lead to serious health issues beyond the immediate danger. These complications may involve repeated clotting as well as ongoing damage to lung and heart function.
Risks of Recurrence
Patients who experience a blood clot in the leg or lungs have a significant risk of developing additional clots. Recurrence rates vary but can be as high as 30% within the first 10 years after the initial event.
Risk factors for recurrence include prolonged immobility, certain genetic clotting disorders, cancer, and inadequate anticoagulant treatment.
Preventive measures usually involve long-term blood thinners, but the duration depends on individual risk. Without proper management, repeated clot formation increases the chance of chronic complications or fatal outcomes.
Chronic Health Issues
Long-term consequences of blood clots reaching the lungs often involve chronic thromboembolic pulmonary hypertension (CTEPH). This condition causes high blood pressure in the lungs, leading to persistent shortness of breath and reduced exercise capacity.
Other possible chronic effects include post-thrombotic syndrome (PTS), which results in leg swelling, pain, and skin changes after deep vein thrombosis. These conditions reduce quality of life and may require ongoing treatment or surgery in severe cases.
Note: Early diagnosis and treatment are crucial to minimize lasting damage and improve long-term health outcomes.
FAQs About Blood Clots Traveling From the Legs to the Lungs
What Are the First Signs of a Blood Clot in the Leg?
The earliest signs of a blood clot in the leg, or deep vein thrombosis (DVT), often include swelling, warmth, redness, and tenderness in the affected area. Pain may feel like cramping or soreness, usually in the calf or thigh, and it often worsens when standing or walking.
Some people also notice the skin becoming tight or slightly discolored. Because these symptoms can resemble other conditions, it’s important to seek medical evaluation promptly to confirm whether a clot is present.
How to Know if a Blood Clot Is Traveling?
If a blood clot breaks loose and begins traveling toward the lungs, symptoms can appear suddenly. Warning signs may include sudden shortness of breath, chest pain that worsens with deep breathing or coughing, lightheadedness, rapid heartbeat, and coughing up blood.
These are signs of a pulmonary embolism, which is a life-threatening emergency. Because a clot can move without warning, any abrupt change in breathing or chest discomfort in someone with suspected DVT should be treated as a medical emergency.
Does a Blood Clot in the Leg Hurt Constantly?
A blood clot in the leg does not always cause constant pain. For some, discomfort may come and go, while for others it may feel persistent, often described as a deep ache or cramp.
Pain typically worsens when standing, walking, or flexing the foot, and it is often accompanied by swelling and warmth in the affected leg.
Note: The intensity of pain varies depending on the size and location of the clot. Even mild or intermittent symptoms should not be ignored.
How Long Does It Take for a Blood Clot to Become Fatal?
The time it takes for a blood clot to become fatal varies widely and depends on whether it stays in place or travels. A clot in the leg (DVT) itself is not usually fatal, but if it breaks free and reaches the lungs, it can cause a pulmonary embolism within seconds to minutes.
Note: A large embolism may block blood flow suddenly, leading to collapse or death. Prompt diagnosis and treatment of DVT greatly reduce the risk of such outcomes.
How Do You Know if a Blood Clot Went to Your Lungs?
When a blood clot reaches the lungs, it causes a pulmonary embolism, which has distinct warning signs. These include sudden shortness of breath, sharp chest pain that worsens with deep breaths, rapid heartbeat, lightheadedness, and sometimes coughing up blood.
Some people may also feel anxious or faint. Because these symptoms overlap with other medical emergencies, immediate medical evaluation is crucial. Diagnostic tests like CT scans, chest X-rays, or blood work help confirm the presence of a pulmonary embolism.
What Are the Chances of Surviving a Blood Clot in the Lungs?
Survival rates for a pulmonary embolism (PE) vary depending on its size, location, and how quickly it is treated. With prompt medical care, the majority of patients survive and recover well. However, untreated PE can be fatal in up to one-third of cases.
Modern treatments, such as anticoagulant medications, clot-busting drugs, or surgical removal, have greatly improved outcomes. Long-term survival also depends on addressing underlying risk factors, such as immobility, smoking, or chronic health conditions. Early detection is critical.
Is It Possible to Prevent a Blood Clot from Traveling?
Yes, medical treatment can prevent a blood clot from traveling. Doctors often prescribe anticoagulant medications (blood thinners) to stop existing clots from growing and to reduce the risk of them breaking off.
In some cases, compression stockings or pneumatic devices are used to improve blood flow in the legs. For patients at very high risk, a filter may be placed in the inferior vena cava (IVC) to trap clots before they reach the lungs. Lifestyle changes, like staying active, also help.
Can a Blood Clot Go Away on Its Own?
Some small blood clots may dissolve naturally as the body’s fibrinolytic system breaks them down over time. However, larger or more dangerous clots often require medical treatment to reduce serious risks.
Anticoagulant therapy helps prevent new clots from forming while the body works to dissolve the existing one. Without treatment, clots may grow, dislodge, and cause a pulmonary embolism.
Note: Because it is difficult to know which clots will resolve safely, all suspected clots require professional evaluation and treatment.
What Are the Complications of a Pulmonary Embolism?
A pulmonary embolism can cause both short- and long-term complications. Immediately, it may block blood flow in the lungs, leading to low oxygen levels, heart strain, or sudden death in severe cases. Survivors may develop pulmonary hypertension, a condition in which high pressure in lung arteries damages the heart over time.
Recurrent embolisms are also possible if underlying risk factors are not managed. Prompt treatment reduces complications, but ongoing monitoring and preventive care are often necessary to protect long-term health.
Can a Pulmonary Embolism Be Prevented?
Yes, prevention is possible, especially for people at higher risk. Regular movement, especially during long periods of sitting or travel, helps improve circulation. Wearing compression stockings, staying hydrated, and avoiding smoking can also reduce risk.
In hospital settings, patients may receive blood-thinning medications or leg compression devices to prevent clot formation. Identifying and managing underlying conditions such as obesity, cancer, or hormonal therapy use further lowers risk.
Note: Prevention strategies are tailored to each patient’s situation and medical history.
Do All Blood Clots Travel and Become Dangerous?
Not all blood clots travel or cause serious harm. Some remain small, stable, and confined to superficial veins, where they may cause discomfort but are less likely to become life-threatening. However, clots in deep veins (DVTs) have a higher risk of dislodging and traveling to the lungs, leading to a pulmonary embolism.
Note: Because it’s difficult to predict which clots will move, all clots should be taken seriously. Timely medical evaluation ensures proper treatment and lowers the risk of complications.
Final Thoughts
A blood clot in the legs can become life-threatening if it travels to the lungs, and the speed at which this happens underscores the importance of early detection and intervention. While a clot may remain stable in the leg for days or weeks, once it dislodges, it can reach the lungs within seconds to minutes, causing a pulmonary embolism.
Recognizing risk factors, paying attention to warning signs like swelling or sudden shortness of breath, and seeking prompt medical care are essential steps in preventing serious complications. By understanding how fast blood clots can travel, individuals and healthcare providers can act quickly to protect health and save lives.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Waheed SM, Kudaravalli P, Hotwagner DT. Deep Venous Thrombosis. [Updated 2023 Jan 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025.
- Office of the Surgeon General (US); National Heart, Lung, and Blood Institute (US). The Surgeon General’s Call to Action to Prevent Deep Vein Thrombosis and Pulmonary Embolism. Rockville (MD): Office of the Surgeon General (US); 2008.


