Tachycardia is a condition in which the heart beats faster than normal, generally defined as a resting heart rate above 100 beats per minute in adults. While it may occur temporarily in response to exercise, stress, or fever, persistent or severe tachycardia can signal underlying health problems that demand medical attention.
For respiratory therapists, recognizing tachycardia is essential because it is often linked to hypoxemia, respiratory distress, or medication effects. This article explains what tachycardia is, why it matters, and its relevance in the field of respiratory care.
What is Tachycardia?
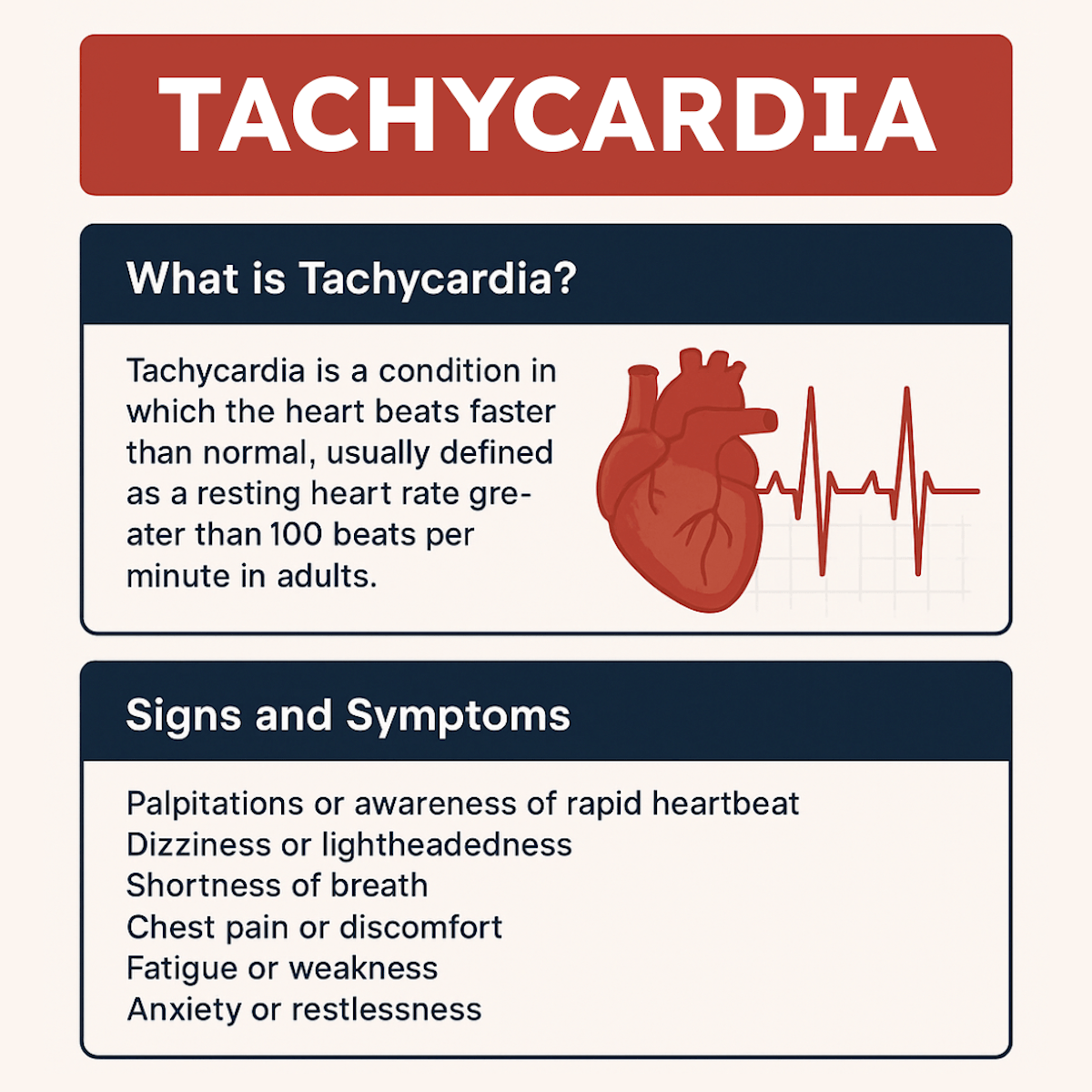
Tachycardia is a condition in which the heart beats faster than normal, usually defined as a resting heart rate greater than 100 beats per minute in adults. It occurs when the electrical signals in the heart that control the heartbeat misfire or become overly active. Tachycardia can originate in different areas of the heart, such as the atria, ventricles, or the sinoatrial (SA) node.
While mild or temporary tachycardia may be a normal response to exercise, stress, or fever, persistent or severe cases can indicate underlying health problems.
Potential causes include hypoxemia, anemia, dehydration, electrolyte imbalances, thyroid disorders, or cardiac disease. If untreated, tachycardia may reduce cardiac efficiency, decrease oxygen delivery, and increase the risk of complications like ischemia or cardiac arrest.
Signs and Symptoms
- Palpitations or awareness of rapid heartbeat
- Dizziness or lightheadedness
- Shortness of breath
- Chest pain or discomfort
- Fatigue or weakness
- Anxiety or restlessness
Note: Severe or sustained tachycardia can result in hypotension, syncope, or progression to life-threatening arrhythmias.
Why is Tachycardia Relevant to Respiratory Therapists?
Respiratory therapists frequently encounter patients with tachycardia in acute and critical care settings. It is a vital sign that reflects the body’s response to stress, hypoxemia, or other systemic issues.
Understanding tachycardia is crucial in the following ways:
1. Indicator of Hypoxemia
One of the earliest responses to hypoxemia is tachycardia, as the body attempts to compensate for reduced oxygen levels by increasing cardiac output. For respiratory therapists, this highlights the importance of timely oxygen therapy, airway management, and ventilatory support.
2. Procedural Triggers
During suctioning, intubation, or patient agitation on mechanical ventilation, tachycardia may develop due to stress, pain, or sympathetic stimulation. Respiratory therapists must anticipate these responses and ensure proper monitoring and intervention.
3. Monitoring in Emergencies
In cardiac arrest and resuscitation, tachycardia may present as pulseless ventricular tachycardia, requiring immediate recognition and advanced life support measures. Respiratory therapists, as part of the resuscitation team, must be prepared to manage the airway and provide effective ventilation during these events.
4. Medication Considerations
Certain drugs, including bronchodilators like beta-agonists, may cause tachycardia as a side effect. Respiratory therapists should recognize medication-induced tachycardia and differentiate it from other underlying causes.
Clinical Relevance in Respiratory Care
Tachycardia is an important clinical finding across multiple areas of respiratory therapy. Recognizing it allows respiratory therapists to respond appropriately and prevent complications.
Here are some key clinical contexts where tachycardia is significant:
- Hypoxemic Respiratory Failure: Tachycardia often develops as the body compensates for low oxygen levels.
- Critical Care: Sustained tachycardia may indicate sepsis, worsening hypoxemia, or complications with ventilation.
- Transport and Emergencies: Patients in unstable conditions frequently show tachycardia as a stress response, requiring close monitoring.
Note: Identifying tachycardia in these settings ensures early interventions that can stabilize the patient and improve outcomes.
Tachycardia Practice Questions
1. What condition can low oxygen levels (hypoxemia) trigger in the cardiovascular system?
Tachycardia
2. Tachycardia is defined as a heart rate greater than how many beats per minute in adults?
100 bpm
3. A heart rate exceeding 150 beats per minute is most likely due to what cardiac issue?
An arrhythmia
4. In managing any form of tachycardia, what must be assessed first?
Whether the patient has a pulse
5. What intervention is generally not indicated for stable sinus tachycardia?
Cardioversion
6. Which arterial blood gas abnormalities can cause tachycardia?
Low PaO₂ or high PaCO₂
7. Which of the following is a common physiological trigger of tachycardia?
Anxiety, pain, fever, or trauma
8. Name three medications that can cause tachycardia.
Beta agonists, atropine, stimulants like caffeine or cocaine
9. What is the typical heart rate range for tachycardia in adults seen on ECG?
100–180 beats per minute
10. On ECG, what P wave pattern is usually seen with sinus tachycardia?
There is one P wave for every QRS complex
11. In tachycardia, what is the usual duration of the PR interval?
Less than 0.2 seconds
12. What does a shortened R-R interval (less than 0.60 seconds) indicate on ECG?
Tachycardia
13. What is the term for tachycardia that originates above the ventricles?
Supraventricular tachycardia (SVT)
14. What does the prefix “supra-” in supraventricular tachycardia refer to?
Above the ventricles (e.g., atria)
15. What type of tachycardia originates in the atria?
Supraventricular tachycardia
16. What are two lower chambers of the heart that may be involved in ventricular tachycardia?
The ventricles
17. Which type of drug may be prescribed to slow a fast heart rate caused by tachycardia?
Negative chronotropic agents (e.g., beta-blockers, calcium channel blockers)
18. What medical condition involving low red blood cell count can lead to tachycardia?
Anemia
19. What thyroid condition may result in tachycardia due to increased metabolism?
Hyperthyroidism
20. What should a respiratory therapist evaluate if tachycardia is seen in a ventilated patient?
Patient–ventilator synchrony and ABG results
21. What should be done if a patient develops tachycardia and is failing to wean from the ventilator?
Return to previous ventilator settings and reassess
22. Why might fever cause an increased heart rate?
Due to elevated metabolic demand and sympathetic stimulation
23. What illicit drugs are known to cause tachycardia?
Amphetamines and cocaine
24. Which type of medication used during respiratory treatment can inadvertently cause tachycardia?
Beta-2 agonists (e.g., albuterol)
25. What can relieve tachycardia caused by anxiety or pain?
Treating the underlying cause (e.g., pain management, anti-anxiety measures)
26. What is the most common form of supraventricular tachycardia (SVT)?
Atrioventricular nodal re-entry tachycardia (AVNRT)
27. What structure in the heart functions as its natural pacemaker?
The sinoatrial (SA) node
28. In normal rhythm, where do electrical impulses originate to set the heart rate?
The SA node
29. In SVT, where do the electrical impulses that drive the heart rate originate?
From a site other than the SA node
30. What analogy describes the loss of SA node control in SVT?
It’s like a car speeding up on its own without driver input
31. Where is the atrioventricular (AV) node located?
Between the atria and ventricles
32. What is the AV node often compared to due to its signal-slowing function?
A speed bump for electrical signals
33. In which part of the heart does AV nodal re-entry tachycardia (AVNRT) occur?
The AV node
34. What electrical loop causes AVNRT to produce tachycardia?
A signal travels from atria to ventricles and re-enters the atria through the AV node repeatedly
35. What is the second most common type of SVT?
Wolff-Parkinson-White (WPW) syndrome
36. What congenital condition causes WPW syndrome?
An accessory pathway between the atria and ventricles
37. What is the name of the abnormal electrical pathway seen in WPW syndrome?
The bundle of Kent
38. Why is the AV node bypassed in WPW syndrome?
The accessory pathway allows signals to reach the ventricles without delay
39. What is the third most common type of SVT?
Atrial tachycardia
40. What is the cause of atrial tachycardia?
An ectopic focus in the atria fires rapidly and independently
41. In atrial tachycardia, does the SA node maintain control of the heart rate?
No, it loses control to the ectopic atrial focus
42. What is a common description of SVT in terms of rhythm?
Fast but regular heart rhythm
43. Where does atrial fibrillation originate?
In the pulmonary veins
44. How is the rhythm of atrial fibrillation described?
Irregular and rapid
45. List the three most common types of SVT in order.
AV nodal re-entry tachycardia, WPW syndrome, atrial tachycardia
46. Atrial tachycardia originates in which part of the heart?
The atria
47. What is the term for tachycardia that originates in the ventricles?
Ventricular tachycardia
48. What is the most common cause of ventricular tachycardia?
Ischemic heart disease
49. What condition results in the heart not receiving enough oxygen due to blocked arteries?
Ischemic heart disease
50. What are ventricular premature complexes (VPCs) also known as?
Premature ventricular contractions (PVCs)
51. PVCs (premature ventricular contractions) are classified as what type of heartbeat?
An ectopic beat arising outside of the sinoatrial (SA) node
52. What type of medication is commonly used to treat tachycardia by slowing heart rate?
Calcium channel blockers or beta blockers
53. Which of the following is a potential treatment option for tachycardia?
Implantation of a pacemaker
54. Which two medication classes are most often used to manage tachycardia?
Calcium channel blockers and beta blockers
55. What distinguishes supraventricular tachycardia (SVT) from atrial fibrillation?
SVT is fast but regular; atrial fibrillation is fast and irregular
56. The most common form of SVT is caused by what mechanism?
A re-entry circuit looping through the AV node
57. Which of the following is considered the first-line treatment for many types of tachycardia?
Anti-arrhythmic medications
58. Where does supraventricular tachycardia originate?
Above the ventricles
59. A fast and irregular heart rhythm is most characteristic of which condition?
Atrial fibrillation
60. Why does WPW syndrome cause tachycardia?
The electrical signal bypasses the AV node and re-enters the atria through an accessory pathway
61. Which three features are used to classify types of tachycardia on an ECG?
QRS complex appearance, heart rate, and rhythm regularity
62. Which three arrhythmias typically present with a narrow QRS complex?
Sinus tachycardia, atrial fibrillation, atrial flutter
63. What duration defines a narrow QRS complex on an ECG?
Less than 0.12 seconds
64. What duration defines a wide QRS complex on an ECG?
Greater than 0.12 seconds
65. Which of the following are examples of tachycardias with wide QRS complexes?
Monomorphic VT, Polymorphic VT, SVT with aberrancy
66. When heart rate becomes excessively high, what physiological effect is most concerning?
Reduction in cardiac output
67. What are potential consequences of reduced cardiac output caused by tachycardia?
Pulmonary edema, coronary ischemia, and hypotension
68. How does reduced cardiac output affect vital organ perfusion?
It leads to decreased blood flow and oxygen delivery to vital organs
69. Why does excessive tachycardia lower cardiac output?
The ventricles don’t have enough time to fill properly between beats
70. What visual analogy helps explain the effect of tachycardia on cardiac output?
The heart is beating so fast, it’s like a pump cycling without enough fluid to push out
71. Which form of SVT is characterized by a bypass tract known as the bundle of Kent?
Wolff-Parkinson-White (WPW) syndrome
72. What does the AV node do during normal conduction?
Slows down the electrical signal before it reaches the ventricles
73. Which arrhythmia may lead to thrombus formation due to irregular contraction of the atria?
Atrial fibrillation
74. What heart rhythm is characterized by sawtooth-like flutter waves on the ECG?
Atrial flutter
75. Which type of tachycardia is most likely to require electrical cardioversion?
Unstable ventricular tachycardia
76. What type of tachycardia is defined by ongoing symptoms despite supplemental oxygen and airway support?
Unstable tachycardia
77. What is the first-line emergency treatment for unstable tachycardia?
Synchronized cardioversion
78. Which term refers to a heart rate >100 bpm with no significant symptoms?
Stable tachycardia
79. What is a common cause of stable tachycardia related to the heart’s conduction system?
Cardiac electrical abnormalities
80. What diagnostic test should be performed immediately in a patient with stable tachycardia?
An ECG
81. What is the normal duration of a QRS complex on an ECG?
0.12 seconds or less
82. What defines a wide QRS complex on an ECG?
Greater than 0.12 seconds
83. What defines a narrow QRS complex on an ECG?
Less than 0.12 seconds
84. What two interventions are used for a patient with a narrow QRS and regular rhythm?
Vagal maneuvers and adenosine
85. What clinical sign suggests unstable tachycardia that does not improve with oxygen?
Persistent hypotension
86. What is the definitive treatment for unstable tachycardia?
Cardioversion
87. How would you classify a tachycardia with a QRS of 0.10 seconds and no visible P waves?
Narrow complex tachycardia
88. What type of tachycardia is known for sudden onset and sudden termination?
Supraventricular tachycardia (SVT)
89. Which type of tachycardia typically stays within 100–130 bpm?
Sinus tachycardia
90. What tachycardia is usually triggered by external factors like fever or blood loss?
Sinus tachycardia
91. What is the recommended goal when treating sinus tachycardia?
Identify and correct the underlying systemic cause
92. Which treatment may worsen a patient’s condition by reducing cardiac output too much?
Beta blockers
93. How is cardiac output (CO) calculated?
Stroke Volume × Heart Rate
94. What happens if you try to lower the heart rate in a patient with compensatory tachycardia?
Cardiac output falls, worsening the condition
95. What type of tachycardia occurs when the heart increases its rate to make up for impaired ventricular function, such as in large myocardial infarctions?
Compensatory tachycardia
96. What are four initial treatment options for narrow complex tachycardias?
Vagal maneuvers, adenosine, calcium channel blockers, beta blockers
97. What physical maneuvers can terminate approximately 25% of SVT episodes?
Valsalva maneuver or carotid sinus massage
98. What is the first recommended treatment for stable narrow complex tachycardia?
Vagal maneuvers
99. What procedure requires a patient to bear down or exhale forcefully against a closed glottis to slow the heart rate?
Valsalva maneuver
100. If vagal maneuvers are ineffective, what is the next recommended treatment for SVT?
Adenosine 6 mg IV with arm elevation
Final Thoughts
Tachycardia is a common finding that often reflects underlying changes in a patient’s condition. For respiratory therapists, awareness of its causes and implications is an important part of monitoring and providing care.
Whether it develops in response to hypoxemia, stress during procedures, or as a side effect of medication, recognizing tachycardia allows for timely adjustments to treatment and closer observation. This helps support safe and effective management of patients in both acute and critical care settings.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Gopinathannair R, Olshansky B. Management of tachycardia. F1000Prime Rep. 2015.