Pleural diseases are a group of conditions that affect the pleura, the thin, double-layered membrane that surrounds the lungs and lines the chest cavity. Although often overshadowed by primary lung diseases, pleural disorders can significantly impair breathing, gas exchange, and overall respiratory mechanics.
They frequently present with symptoms such as chest pain, dyspnea, and cough, and may develop suddenly or progress gradually.
For respiratory therapists and other healthcare professionals, a solid understanding of pleural diseases is essential, as these conditions commonly influence diagnostic decisions, respiratory interventions, and patient outcomes across a wide range of clinical settings.
What Are Pleural Diseases?
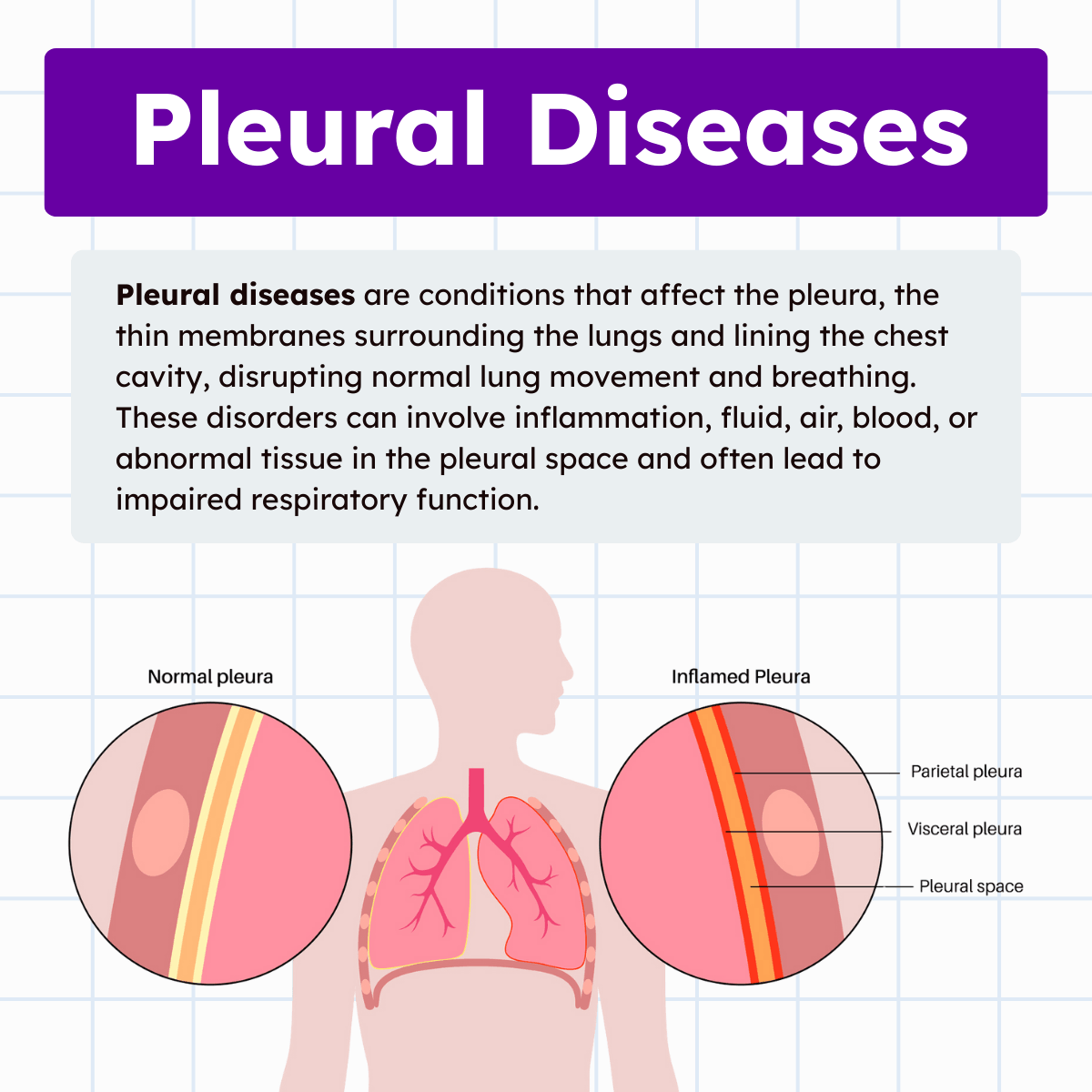
Pleural diseases refer to any pathological condition involving the pleura or the pleural space. The pleura consists of two layers: the visceral pleura, which directly covers the lungs, and the parietal pleura, which lines the chest wall, diaphragm, and mediastinum. Between these layers is the pleural space, a thin cavity containing a small amount of lubricating fluid that allows smooth lung movement during respiration.
Under normal conditions, the pleural space maintains negative pressure, which keeps the lungs expanded. When disease disrupts this balance through inflammation, fluid accumulation, air entry, or tissue thickening, lung expansion becomes compromised. The result can be restricted ventilation, impaired oxygenation, increased work of breathing, and, in severe cases, respiratory failure.
Why Pleural Diseases Matter in Respiratory Care
Pleural diseases are highly relevant to respiratory therapy because they directly affect lung mechanics and gas exchange. Many of these conditions require prompt recognition and intervention to prevent deterioration. Respiratory therapists are often among the first clinicians to assess changes in breath sounds, oxygenation status, respiratory effort, and patient comfort.
In both acute and chronic care settings, pleural disorders influence decisions related to oxygen therapy, ventilatory support, airway management, and patient positioning. Therapists also play a key role in monitoring patients before and after procedures such as thoracentesis or chest tube placement. Understanding pleural pathology helps ensure safe, effective care and improves collaboration with physicians and the broader healthcare team.
Common Types of Pleural Diseases
Pleurisy (Pleuritis)
Pleurisy is inflammation of the pleural layers, often caused by infection, autoimmune disease, pulmonary embolism, or trauma. As the inflamed pleura rub against each other during breathing, patients experience sharp, localized chest pain that worsens with deep inspiration, coughing, or sneezing.
From a respiratory care perspective, pleurisy may lead to shallow breathing patterns as patients attempt to minimize pain. This can increase the risk of atelectasis and hypoventilation. Therapists must balance pain-limited breathing with the need to maintain adequate ventilation and lung expansion.
Pleural Effusion
Pleural effusion occurs when excess fluid accumulates in the pleural space. This fluid may be classified as transudative or exudative, depending on its underlying cause and composition. Common causes include heart failure, pneumonia, malignancy, liver disease, and inflammatory conditions.
As fluid volume increases, lung expansion becomes restricted, leading to dyspnea, reduced lung volumes, and impaired oxygenation. Breath sounds are often diminished over the affected area, and percussion may reveal dullness. Respiratory therapists frequently identify these changes during bedside assessment and play a role in monitoring respiratory status before and after fluid drainage.
Pneumothorax
A pneumothorax occurs when air enters the pleural space, disrupting the negative pressure required for lung expansion. This results in partial or complete lung collapse. Pneumothorax may be spontaneous, traumatic, or iatrogenic, such as following invasive procedures or mechanical ventilation.
Symptoms often include sudden chest pain, dyspnea, tachypnea, and decreased oxygen saturation. Respiratory therapists must rapidly recognize signs of pneumothorax, especially in mechanically ventilated patients, where tension pneumothorax can become life-threatening. Management may involve oxygen therapy, close monitoring, and assisting with chest tube care.
Hemothorax
Hemothorax refers to the accumulation of blood in the pleural space, most commonly due to chest trauma, surgery, or malignancy. The presence of blood restricts lung expansion and may lead to hypovolemia in severe cases.
For respiratory therapists, hemothorax presents challenges similar to pleural effusion, including reduced ventilation and oxygenation. Monitoring respiratory effort, breath sounds, and oxygen requirements is critical, particularly in trauma or postoperative patients.
Empyema
Empyema is an infected pleural effusion characterized by the presence of pus in the pleural space. It often develops as a complication of pneumonia, lung abscess, or thoracic surgery. Empyema can cause severe systemic illness, including fever, sepsis, and respiratory distress.
Effective management typically requires antibiotics and drainage. Respiratory therapists are involved in secretion management, lung expansion strategies, and monitoring the patient’s response to treatment. Failure to manage empyema appropriately can result in long-term pleural scarring and restrictive lung disease.
Chylothorax
Chylothorax is the accumulation of lymphatic fluid in the pleural space due to damage or obstruction of the thoracic duct. Causes include trauma, malignancy, and surgical complications. The presence of chyle interferes with lung expansion and may lead to nutritional and immunologic complications.
From a respiratory care standpoint, chylothorax requires careful monitoring of respiratory status while underlying causes are addressed. Persistent cases may necessitate surgical intervention.
Pleural Thickening and Plaques
Pleural thickening and plaques involve fibrous changes in the pleura, often related to asbestos exposure or prior inflammation. While pleural plaques are usually benign and asymptomatic, extensive thickening can restrict lung expansion and reduce lung compliance.
Respiratory therapists may encounter patients with chronic dyspnea and reduced exercise tolerance related to restrictive changes. Pulmonary function testing often reveals reduced lung volumes, reinforcing the importance of understanding pleural contributions to respiratory limitation.
Diagnostic Considerations in Pleural Diseases
Diagnosing pleural diseases relies on a combination of clinical assessment, imaging, and laboratory analysis. Chest radiographs are commonly used to identify pleural effusions, pneumothorax, and pleural thickening. Ultrasound and CT imaging provide greater detail and are often used to guide procedures.
Respiratory therapists contribute valuable bedside information, including auscultation findings, oxygenation trends, respiratory patterns, and response to interventions. These observations often prompt further diagnostic evaluation and guide treatment decisions.
Treatment and Management Principles
Management of pleural diseases focuses on relieving symptoms, restoring lung expansion, and addressing the underlying cause. Treatment may include oxygen therapy, analgesia, antibiotics, diuretics, drainage procedures, or surgical intervention.
Respiratory therapists are essential in supporting ventilation and oxygenation throughout treatment. They assist with chest tube management, monitor for complications, encourage lung expansion, and adjust respiratory support as the patient’s condition evolves. Education and reassurance provided by therapists also help reduce patient anxiety and improve cooperation with care.
Clinical Importance for Respiratory Therapists
Pleural diseases highlight the close relationship between lung mechanics and respiratory function. Even when the lung tissue itself is relatively healthy, pleural pathology can severely impair breathing. Respiratory therapists must understand how pleural conditions alter compliance, ventilation-perfusion relationships, and work of breathing.
In both acute and long-term care settings, early recognition and appropriate intervention can significantly improve patient outcomes. Knowledge of pleural diseases enhances clinical judgment, improves interdisciplinary communication, and reinforces the respiratory therapist’s role as a key contributor to patient care.
Pleural Disease Practice Questions
1. What are the two most common pleural diseases that you should know about as a respiratory therapist?
Pleural effusion and pneumothorax
2. When do pleural effusions form?
When excess pleural fluid is produced by the lung or chest wall in sufficient quantities to overcome the resorptive capacity of the pleural lymphatic vessels
3. Pleural fluid analysis is the key to what?
It is the key to understanding the specific cause of any pleural effusion.
4. Transudates have a pleural fluid total protein level of what?
Less than 0.5 and an LDH level of less than 0.6 of the respective serum values
5. What are the common causes of a transudative effusion?
The common causes include CHF, nephrosis, and cirrhosis.
6. Pleural fluid drainage returns approximately one-third of the lung volume as measured by what?
FVC; the other two-thirds of fluid drainage allows the diaphragm to rise and the chest wall to normalize.
7. Is a pneumothorax size underestimated or overestimated with a one-dimensional view of the chest?
It is underestimated. Measurement accuracy requires a three-dimensional perspective.
8. Are the risk factors for a pneumothorax and pneumomediastinum the same?
Yes, air ruptures a pleural membrane in a pneumothorax, and air passes through the lung hilum in a pneumomediastinum.
9. Pleural effusions associated with CHF are usually bilateral or unilateral?
Bilateral
10. What does chest tube flow depend on?
It depends on tube size, stopcock size, and collection system resistance.
11. Breath-by-breath measurement of an air leak can be approximated by what?
By the difference between inspired and expired volumes (in the absence of endotracheal cuff leaks)
12. The mode of ventilation that produces the least fistula airflow is the most likely to produce what?
Healing
13. What are the methods to decrease bronchopleural fistula airflow?
Lowering the tidal volume, respiratory rate, PEEP, and avoiding auto-PEEP. In more severe cases, positioning the affected lung down, double-lumen tube ventilation, adding PEEP valves to the chest tube, inspiratory chest tube occlusion, or thoracic surgery should be considered
14. What is a bronchopleural fistula?
Any air communication from the lungs to pleural space
15. What is an empyema?
A collection of pus in the pleural space
16. What is an exudative pleural effusion?
Any pleural effusion high in protein or lactate dehydrogenase, which implies inflammation or vascular injury on the pleural surface
17. What is a hemothorax?
Presence of blood within the pleural space
18. What is the parietal pleura?
A membrane covering the surface of the chest wall, mediastinum, and diaphragm that is continuous with the visceral pleura around the lung hilum.
19. What is a pleural effusion?
Abnormal collection of fluid within the pleural space
20. What is used to remove fluid from a pleural effusion?
Chest tube and thoracentesis
21. What is a primary spontaneous pneumothorax?
A pneumothorax that occurs without underlying lung disease
22. What is re-expansion pulmonary edema?
Pulmonary edema that forms after rapid re-expansion of a lung that has been compressed with pleural fluid or pneumothorax
23. What is a secondary spontaneous pneumothorax?
A pneumothorax that occurs because of underlying lung disease
24. What is a stomata?
Small holes within the parietal pleura that are the main route for pleural fluid to exit
25. What is a thoracentesis?
Surgical perforation of the chest wall and pleural space with a needle for diagnostic or therapeutic purposes or for removal of a specimen for biopsy
26. What is a transudative pleural effusion?
Pleural effusion low in protein or lactate dehydrogenase, usually caused by congestive heart failure, nephrosis, or cirrhosis
27. What is ascites?
The accumulation of fluid in the abdomen
28. What is atelectasis?
When segments of the lung collapse, intrapleural pressure becomes more negative and can produce small effusions
29. What is the primary cause of a transudative pleural effusion?
CHF
30. How is chest radiography used for pleural diseases?
It is most common in detecting a pleural effusion obtained best in the upright position to show a pleural fluid meniscus at the costophrenic angles.
31. How is CHF relevant to pleural diseases?
It is the most common cause of a clinical pleural effusion. It stems from the elevation of pressure in the left atrium and pulmonary veins.
32. How is computed tomography relevant to pleural diseases?
CT scanning of the chest is the most sensitive study for the identification of a pleural effusion.
33. Which side are pleural effusions more common on?
Right
34. Can a pleural effusion cause atelectasis?
Yes, because the fluid limits the ability of the thorax to expand.
35. What unit are chest tubes measured in?
French (Fr)
36. Where is the needle for a thoracentesis inserted?
Just above the rib
37. What is lateral decubitus chest radiography used for?
It can help define the presence or absence of pleural effusion.
38. How many bottles are in a standard chest tube drainage system?
3
39. What does it mean if tidaling does not occur in the water seal chamber?
It means that there could be a kink, clamp, or occlusion in the tubing.
40. What are the common causes of penetrating chest trauma?
Gunshot wounds and knife punctures
41. What is pleurisy?
A respiratory condition characterized by pain and inflammation in the pleura that usually results from a viral infection
42. What is pleurodesis?
A procedure that is performed to obliterate the pleural space
43. How would you describe chest pain from a pneumothorax?
Sharp and abrupt
44. What are the findings of a tension pneumothorax?
Mediastinal shift, decreased venous return, decreased cardiac output, hypotension, tachycardia, and hypoxemia
45. What is the treatment for a tension pneumothorax?
Emergency decompression of the chest
46. Chest palpitation during pleural diseases would reveal what?
Dull percussion note
47. What is the most common type of traumatic pneumothorax?
Iatrogenic pneumothorax
48. What are the risk factors of a Thoracentesis?
Intercostal artery laceration, infection, and pneumothorax
49. Which pleura surrounds the surface of the lungs and interlobar fissures?
Visceral pleura
50. Which pleura covers the entire surface of the diaphragm and thoracic cavity?
Parietal pleura
51. What symptom commonly prompts evaluation for a pleural effusion?
Progressive dyspnea, especially with exertion.
52. Why do small pleural effusions often go unnoticed clinically?
They may not significantly impair lung expansion or gas exchange.
53. What physical exam finding is classically associated with a large pleural effusion?
Decreased breath sounds with dullness to percussion over the affected area.
54. How does a pleural effusion affect lung mechanics?
It restricts lung expansion, leading to a restrictive ventilatory defect.
55. What is the normal volume of pleural fluid in healthy adults?
Approximately 5 to 15 mL per hemithorax.
56. Which pleural disease is most commonly associated with malignancy?
Exudative pleural effusion
57. Why is LDH elevated in exudative pleural effusions?
Because of inflammation and increased cellular breakdown.
58. What pleural disease is most likely to cause pleuritic chest pain?
Pleurisy
59. What auscultatory finding may be heard with pleural inflammation?
A pleural friction rub.
60. Why is ultrasound useful in pleural disease assessment?
It helps detect small effusions and guides thoracentesis safely.
61. What complication can occur if pleural fluid is removed too rapidly?
Re-expansion pulmonary edema.
62. What is the hallmark sign of a pneumothorax on auscultation?
Absent or markedly diminished breath sounds on the affected side.
63. How does intrapleural pressure change during a pneumothorax?
It becomes less negative or positive relative to atmospheric pressure.
64. What type of pneumothorax is associated with mechanical ventilation?
Barotrauma-induced pneumothorax.
65. Why are patients with COPD at higher risk for pneumothorax?
Due to ruptured blebs from hyperinflated lungs.
66. What pleural condition involves infected pleural fluid?
Empyema
67. Why is empyema considered a serious pleural disease?
It can lead to sepsis, lung entrapment, and long-term fibrosis.
68. What imaging finding suggests loculated pleural effusion?
Non-layering fluid collections on chest imaging.
69. What does pleural thickening indicate?
Chronic inflammation or previous pleural disease.
70. How does pleural disease affect oxygenation?
By impairing ventilation-perfusion matching.
71. What pleural disorder results from blood clotting within the pleural space?
Clotted hemothorax
72. Why may chest tube drainage be ineffective in loculated effusions?
Fibrous septations prevent free fluid drainage.
73. What is the primary goal of treating pleural diseases?
Restore lung expansion and adequate ventilation.
74. What finding suggests a resolving pleural effusion?
Improving breath sounds and increased chest expansion.
75. Why is patient positioning important in pleural disease management?
Proper positioning can improve ventilation and comfort.
76. What pleural disease commonly develops as a complication of pneumonia?
Parapneumonic pleural effusion
77. How does a complicated parapneumonic effusion differ from an uncomplicated one?
It is infected, loculated, or associated with low pH and requires drainage.
78. What pleural fluid pH suggests the need for chest tube drainage?
Less than 7.20
79. Why can pleural disease cause referred shoulder pain?
Because the parietal pleura is innervated by the phrenic nerve.
80. What finding on chest X-ray suggests free-flowing pleural fluid?
Blunting of the costophrenic angle with a meniscus sign.
81. What pleural condition is associated with asbestos exposure?
Malignant pleural mesothelioma
82. How does pleural fibrosis affect lung function?
It restricts lung expansion and reduces compliance.
83. What is a trapped lung?
A condition where the lung cannot fully expand due to fibrous pleural restriction.
84. Why may patients with pleural effusion prefer to sit upright?
This position reduces dyspnea by improving lung expansion.
85. What pleural disorder is characterized by air and fluid in the pleural space?
Hydropneumothorax
86. What bedside sign may suggest pleural effusion without imaging?
Asymmetric chest expansion
87. Why are pleural diseases often associated with restrictive lung patterns?
Because lung expansion is mechanically limited.
88. What pleural condition results from lymphatic obstruction?
Chylothorax
89. What type of pleural fluid is seen in chylothorax?
Milky fluid rich in triglycerides.
90. Why is early treatment of pleural infections important?
To prevent fibrosis and permanent lung restriction.
91. What pleural disease can result from pancreatitis?
Exudative pleural effusion.
92. How does pleural disease affect ventilation-perfusion relationships?
It worsens V/Q mismatch by compressing ventilated lung tissue.
93. What pleural finding is common after thoracic surgery?
Small reactive pleural effusions.
94. Why are chest tubes measured in French units?
Because tube size corresponds to outer diameter.
95. What pleural disease is associated with systemic lupus erythematosus?
Pleuritis with pleural effusion.
96. What clinical sign may indicate worsening pleural disease?
Increasing dyspnea at rest.
97. Why can pleural effusions reduce exercise tolerance?
They limit lung expansion and increase work of breathing.
98. What pleural disorder is most likely to recur without definitive treatment?
Malignant pleural effusion.
99. What role does pleural pressure play in normal breathing?
It keeps the lungs expanded against the chest wall.
100. Why does air in the pleural space cause lung collapse?
It eliminates the negative pressure needed to keep the lung inflated.
Final Thoughts
Pleural diseases encompass a diverse group of conditions that directly affect lung expansion, ventilation, and oxygenation. From pleural effusions and pneumothorax to empyema and pleural thickening, these disorders present unique challenges that require prompt recognition and thoughtful management.
For respiratory therapists, understanding pleural anatomy and pathology is essential for accurate assessment, effective intervention, and safe monitoring of patients.
By recognizing how pleural disease alters respiratory mechanics and supporting patients through both acute and chronic phases of illness, respiratory therapists play a vital role in optimizing outcomes and advancing quality respiratory care.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Gowing SD, Madani A. Pleural Disorders. Pocket Manual of General Thoracic Surgery. 2015.