Acute respiratory distress syndrome (ARDS) is a life-threatening condition characterized by sudden and severe inflammation in the lungs, leading to widespread alveolar damage and impaired gas exchange.
Often triggered by trauma, pneumonia, sepsis, or other critical illnesses, ARDS can rapidly progress to respiratory failure, requiring intensive medical intervention such as mechanical ventilation. Despite advances in critical care, ARDS remains associated with high morbidity and mortality.
Understanding its causes, clinical features, and treatment options is crucial for timely recognition and management, ultimately improving patient outcomes and reducing complications.
Take our free course to master essential pathology concepts with TMC/CSE exam tips and helpful practice questions.
What is ARDS?
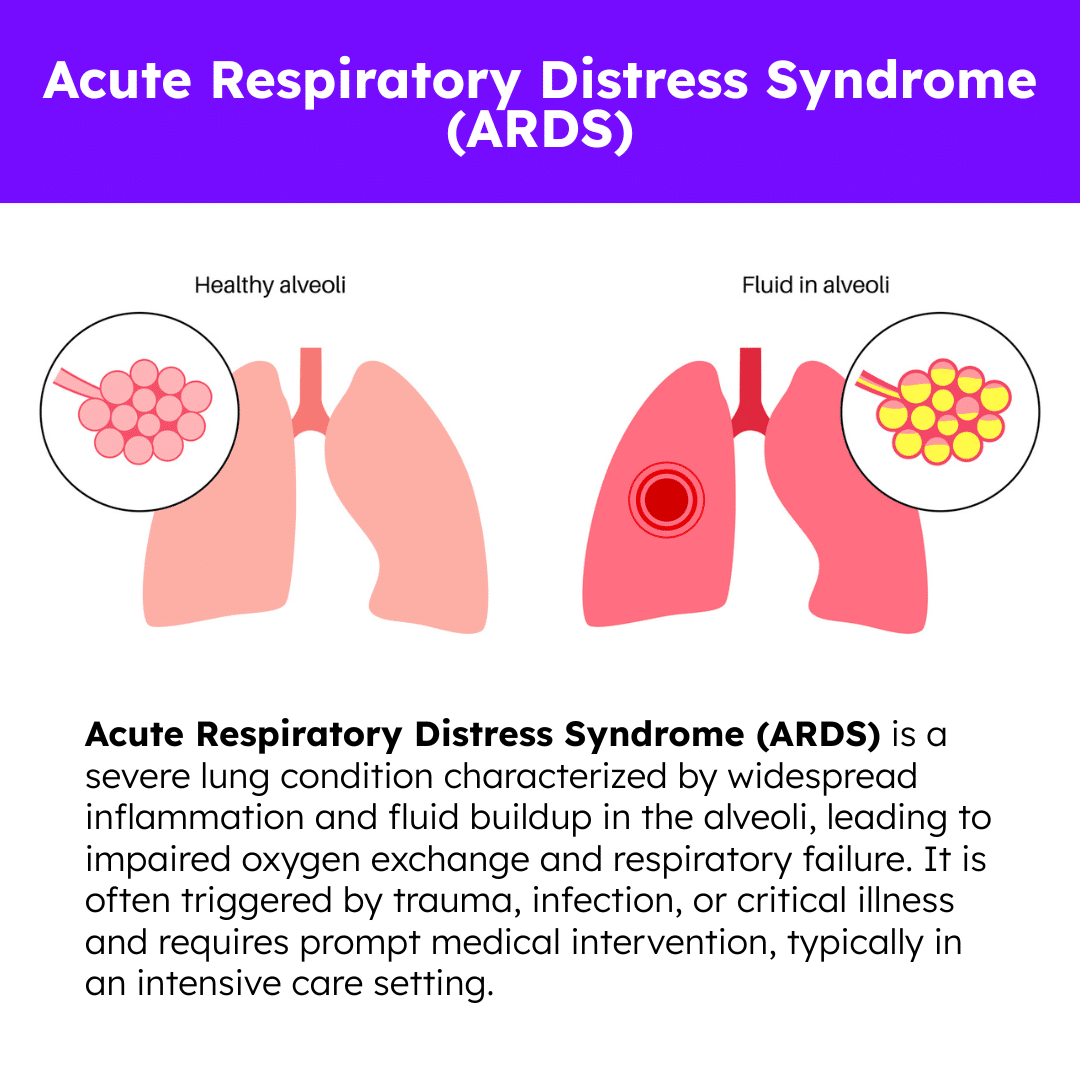
Acute respiratory distress syndrome (ARDS) is a serious medical condition in which fluid builds up in the tiny air sacs (alveoli) of the lungs, preventing oxygen from effectively entering the bloodstream. It typically occurs in response to a severe illness or injury, such as pneumonia, sepsis, trauma, or inhalation of harmful substances.
ARDS causes inflammation and increased permeability of the lung’s blood vessels, leading to respiratory failure and low blood oxygen levels. Symptoms include rapid breathing, severe shortness of breath, and low oxygen saturation.
Treatment usually requires intensive care, including oxygen therapy or mechanical ventilation. ARDS can develop quickly and is often life-threatening, but recovery is possible with prompt and appropriate medical support.
Causes
ARDS can develop in response to various severe health events or injuries that trigger widespread inflammation in the lungs. Common causes include:
- Infections: Severe pneumonia and systemic infections like sepsis are leading contributors to ARDS.
- Inhalation of Harmful Substances: Breathing in smoke, toxic chemicals, or stomach contents (aspiration) can cause direct lung injury.
- Trauma: Serious physical injuries, including blunt chest trauma or major accidents, can initiate an inflammatory response.
- Medical Complications: Certain procedures, including major surgeries or multiple blood transfusions, may increase ARDS risk.
- Severe Inflammatory Conditions: Illnesses like pancreatitis or autoimmune diseases can lead to systemic inflammation and lung involvement.
Note: These triggers can damage the alveoli, leading to fluid leakage, poor gas exchange, and respiratory failure.
Symptoms
The onset of ARDS is usually rapid and can quickly progress to a medical emergency. Common symptoms include:
- Severe Shortness of Breath: Often the earliest and most noticeable symptom due to impaired oxygen exchange.
- Labored and Rapid Breathing: The body attempts to compensate for low oxygen levels by increasing breathing rate and effort.
- Hypoxemia: Blood oxygen levels drop dangerously low, even with supplemental oxygen therapy.
- Cough: May be dry or produce minimal sputum.
- Fatigue and Weakness: Reduced oxygen delivery to muscles and tissues leads to overall exhaustion.
- Confusion or Agitation: Low oxygen levels can impair brain function, especially in older adults.
- Fever: Often present when infection is the underlying cause.
Note: ARDS symptoms require urgent evaluation and treatment in a hospital or intensive care setting.
Diagnosis
Diagnosing ARDS involves a combination of clinical evaluation and diagnostic testing to confirm lung dysfunction and rule out other conditions. Steps may include:
- Medical History and Physical Exam: Doctors assess respiratory symptoms and examine for signs of fluid buildup and decreased breath sounds.
- Blood Tests: Help detect infections, inflammation, and oxygenation status.
- Chest X-ray: Reveals diffuse infiltrates or white-out patterns consistent with fluid in the lungs.
- CT Scan: Provides a more detailed view of lung structure and areas of damage.
- Arterial Blood Gas (ABG) Test: Measures oxygen and carbon dioxide levels to assess lung function and severity of hypoxemia.
- Echocardiogram: Evaluates heart function and helps exclude cardiac causes of pulmonary edema.
- Bronchoscopy: Occasionally used to inspect the airways and collect samples for further analysis.
Note: ARDS is diagnosed based on clinical criteria and exclusion of other potential causes, as outlined by the Berlin Definition and supported by research guidelines.
Treatment
Managing ARDS requires supportive care in an intensive care unit and addressing the root cause of the condition. Treatment strategies include:
- Mechanical Ventilation: Used to support breathing, reduce the work of respiration, and deliver precise oxygen levels while minimizing lung injury.
- Oxygen Therapy: Administered to correct low blood oxygen and maintain adequate oxygenation.
- Prone Positioning: Turning patients onto their stomachs helps improve lung expansion and oxygen exchange in many cases.
- Fluid Management: Carefully balancing fluid intake and output prevents fluid overload and reduces pulmonary edema.
- Medications: Treatment may include antibiotics for infections, corticosteroids to reduce inflammation, and sedatives for ventilated patients.
- Treating Underlying Causes: Prompt management of the condition that triggered ARDS is essential for recovery.
- Supportive Care: Nutritional support, blood clot prevention, physical therapy, and close monitoring are vital to reduce complications and promote healing.
Note: ARDS treatment often involves a team approach, including pulmonologists, intensivists, nurses, and respiratory therapists. Recovery may take weeks to months, and some patients require long-term rehabilitation.
What is the ARDSnet Protocol?
The ARDSnet protocol refers to a set of evidence-based guidelines developed by the ARDS Network, a collaborative group of U.S. research centers dedicated to improving the care of patients with Acute Respiratory Distress Syndrome (ARDS).
This protocol is most widely recognized for revolutionizing mechanical ventilation strategies in ARDS, particularly through its focus on lung-protective ventilation. Its core aim is to reduce ventilator-induced lung injury (VILI) and improve patient outcomes.
- Low Tidal Volume Ventilation: The protocol recommends delivering smaller tidal volumes—approximately 6 mL per kilogram of predicted body weight—instead of traditional higher volumes. This lung-protective approach helps minimize ventilator-induced lung injury.
- Limiting Plateau Pressure: To protect delicate lung tissue, plateau pressures are kept at or below 30 cm H2O, reducing the risk of barotrauma and overdistension.
- Oxygenation and Ventilation Goals: The protocol sets specific targets for arterial oxygen (PaO2) and carbon dioxide (PaCO2) levels, promoting adequate gas exchange while avoiding the complications of overventilation.
- Conservative Fluid Management: Fluid balance is carefully managed to prevent pulmonary edema while ensuring adequate perfusion to vital organs.
- Additional Supportive Strategies: The protocol includes guidance on the use of prone positioning, neuromuscular blockade during early ARDS, and other adjunctive therapies as part of comprehensive critical care.
Note: The ARDSnet protocol, especially the use of low tidal volume ventilation, has been shown in clinical trials to significantly reduce mortality in ARDS patients. It remains a cornerstone of evidence-based ARDS management in intensive care settings.
ARDS Practice Questions
1. What is acute respiratory distress syndrome (ARDS) characterized by?
ARDS is characterized by rapid-onset, severe inflammation in the lungs, leading to fluid accumulation and significant breathing difficulties.
2. What are the clinical hallmarks of ARDS?
Hypoxemia, bilateral radiographic opacities, and diffuse alveolar damage.
3. What should a respiratory therapist monitor in patients with ARDS?
Cardiovascular compromise (decreased carbon dioxide), changes in blood pressure, decreased pulse intensity, oxygen saturation, mental status changes, and laboratory values.
4. What can be seen in the chest imaging of patients with ARDS?
Bilateral opacities that are not fully explained by effusions, lobar/lung collapse, or nodules.
5. What is the origin of edema in ARDS?
Respiratory failure that is not fully explained by cardiac failure or fluid overload. If no risk factors are present, echocardiography can be used to exclude hydrostatic edema.
6. What are the most common risk factors for ARDS?
Severe sepsis, pneumonia, aspiration, trauma (including pulmonary contusion), multiple transfusions, pancreatitis, near-drowning, medical prescription overdose, hyper transfusion, burns, infections, post-resuscitation, and cardiopulmonary bypass.
7. What are the signs and symptoms of ARDS?
This disease has a rapid onset, occurring 12-48 hours after insult/injury, respiratory distress, and multi-organ dysfunction syndrome.
8. How do you diagnose ARDS?
Diagnosis happens simultaneously with interventions, chest x-ray, CT scan of the chest with or without contrast, CBC count, comprehensive metabolic panel, CE, lactate, and urine drug testing. The medical history is important to consider (i.e., what occurred within 48 hours), type of work, drug use, medications, and the patient’s past medical history.
9. What can be observed on the chest x-ray of a patient with ARDS?
It is indistinguishable from those of cardiogenic pulmonary edema. Bilateral opacities consistent with pulmonary edema with diffuse bilateral infiltrates (i.e., white-out). Bilateral infiltrates may be patchy or asymmetric and may include pleural effusions.
10. What are some treatment methods for ARDS?
Oxygen therapy, prone positioning, administration of Nitric oxide and steroids, inverse ratio ventilation, and high-frequency oscillatory ventilation.
11. What are the pathologic or structural changes with ARDS?
Interstitial and intra-alveolar edema and hemorrhage, alveolar consolidation, intra-alveolar hyaline membrane, and pulmonary surfactant deficiency or abnormality atelectasis
12. What is another name for ARDS?
“Shock Lung Syndrome”
13. What etiologic factors can produce ARDS?
These include aspiration, disseminated intravascular coagulation, drug overdose, fat or air emboli, fluid overload, infection, inhalation of toxins and irritants, immunologic reaction, massive blood transfusion, oxygen toxicity, and pulmonary ischemia. Also, radiation-induced lung injury, shock, systemic reactions to processes initiated outside the lungs, thoracic trauma (i.e., pneumothorax), and uremia.
14. What are the clinical manifestations of ARDS?
Atelectasis, alveolar consolidation, and increased alveolar-capillary membrane thickness.
15. What clinical data can be obtained at the bedside of patients with ARDS?
Patients manifest increased RR (respiratory rate), HR (heart rate), BP (blood pressure, and CO (carbon monoxide). The chest has a dull percussion note, bronchial breath sounds, and crackles.
16. What are the typical ABG results for a patient with ARDS?
Mild to moderate-acute alveolar hyperventilation with hypoxemia. In severe cases, acute ventilatory failure with hypoxemia.
17. What are the general radiologic findings for ARDS?
Increased opacity
18. What are the ideal ventilator settings for ARDS patients?
Low tidal volumes (4-6 mL/kg) and high respiratory rates (as high as 35 bpm).
19. Which white blood cell is most commonly implicated in the inflammatory process of ARDS?
Neutrophils
20. What is the mortality rate for ARDS?
The mortality rate for ARDS is not definite and depends on the severity of the condition. Mortality correlates with the driving pressure, the difference between plateau and positive end-expiratory pressure (PEEP).
21. What clinical features are seen in both ARDS and CHF patients?
They both have diffused alveolar and interstitial infiltrates on a chest radiograph.
22. What time frame does ARDS typically occur?
Between one and three days.
23. What is not a common finding in the exudative phase of ARDS?
Bradypnea
24. What mode of mechanical ventilation is designed to optimize ventilation by recruiting alveolar units while minimizing ventilator-induced barotrauma in patients with ARDS?
Airway pressure release ventilation (APRV)
25. What organ plays a major role in the induction and modulation of the systemic inflammatory response?
Liver
26. What is a secondary risk factor for ARDS?
Sepsis
27. What treatment is not recommended for patients with ARDS?
The routine use of extracorporeal membrane oxygenation (ECMO) is not recommended.
28. What mode of mechanical ventilation is designed to optimize ventilation by reducing alveolar collapse while using small tidal volumes in patients with ARDS?
High-frequency ventilation (HFV)
29. What can be observed in the physical size of the lungs of patients suffering from ARDS?
The lungs are reduced by 20-30% of their normal size.
30. What is the indication that inhaled nitric oxide may be useful for patients with ARDS?
Severe elevation of the pulmonary vascular resistance.
Access our quiz with sample TMC practice questions and detailed explanations to help you master the key concepts of pathology.
31. What mechanisms ultimately lead to ARDS regardless of the etiology?
Disruption of the endothelial and epithelial barriers.
32. What assessment tool is most useful in distinguishing ARDS from CHF?
Swan-Ganz catheter
33. What is considered an experimental therapy for patients with ARDS?
Inhaled nitric oxide (NO)
34. What tidal volume range is recommended for patients with ARDS?
4-6 mL/kg
35. What parameter is important in determining the optimal level of PEEP for a patient with ARDS?
Oxygen delivery
36. What frequent assessments should be completed by a respiratory therapist in the treatment of a patient with ARDS?
Arterial blood gas, hemodynamic parameters, and evaluation of the effectiveness of treatment.
37. What ventilatory strategy has been found to be useful for avoiding barotrauma in the treatment of patients with ARDS?
Permissive hypercapnia
38. What drug therapy is available for ARDS?
Antibiotics, diuretics, and sedation in mechanically ventilated patients.
39. What parameters are important in the management of patients with ARDS?
Keep hemoglobin saturation above 90%, ensure adequate urine output, and keep the mean arterial pressure above 60 mmHg.
40. What lung protective strategies can be used during mechanical ventilation?
Low tidal volume (i.e., 4-6 mL/kg) and low to moderately high PEEP (i.e., 5-20 cmH20) to keep alveoli open and diminish the negative effects of high-pressure settings.
41. What is the benefit of prone positioning when treating ARDS?
It produces transient improvement of gas exchange.
42. What is the maximal inspiratory pressure that should be targeted when using pressure control ventilation in patients with ARDS?
30-35 cmH2O
43. What benefit has not been associated with the use of PEEP when treating ARDS?
Improved venous return
44. What complication has been associated with the use of PEEP in patients with ARDS?
Reduced cardiac output
45. What is the name of the period that follows the exudative phase of ARDS?
Fibroproliferative
46. What test provides useful information in making the diagnosis of ARDS for patients with inconclusive results on traditional tests?
Examination of bronchoalveolar lavage fluid.
47. What is the difference between acute lung injury (ALI) and acute respiratory distress syndrome (ARDS)?
Acute lung injury is when the P/F ratio is 200-300. The alveoli fill with fluid resulting in severe dyspnea, hypoxemia refractory to supplemental oxygen, reduced lung compliance, and diffuse pulmonary infiltrates. On the other hand, ARDS is a sudden and progressive form of acute respiratory failure in which the alveolar-capillary interface becomes damaged and more permeable to intravascular fluid. The P/F ratio for ARDS is less than 200.
48. What are the most common causes of ARDS?
ARDS is caused by aspiration of gastric contents or other substances, viral or bacterial pneumonia, sepsis, and severe massive trauma. Other cause includes chest trauma, embolism, near-drowning, oxygen toxicity, DIC (disseminated intravascular coagulation), pancreatitis, severe head injury, and shock.
49. What are pulmonary insults that can cause ARDS?
These are inhaled or aspirated noxious agents that induce the inflammatory response in the lung and result in alveolar collapse and endothelial damage, which leads to hyaline membrane formation.
50. What are the most important causes of ARDS?
Pneumonia, aspiration, sepsis, and trauma.
51. What is the result of both pulmonary and systematic causes of ARDS?
Increased permeability of the alveolar-capillary membrane leading to pulmonary edema.
52. What is the result of a lung scan in patients with ARDS?
There will be a ventilation/perfusion (V/Q) mismatch.
53. What causes arterial hypoxemia in ARDS?
Shunting and mixing of unoxygenated blood.
54. What manifestation can be seen in the blood oxygen level of patients with ARDS?
Severe arterial hypoxemia
55. Does ARDS result in increased or decreased compliance?
Decreased compliance
56. In ARDS, will the lungs increase or decrease in stiffness?
ARDS causes increased lung stiffness.
57. What is the typical onset time of ARDS after a triggering event?
Within 72 hours or 7 days after a triggering event.
58. What are the severity levels of ARDS?
ARDS is classified as mild, 200-300 mmHg; moderate, 100-200 mmHg; and severe, less than 100 mmHg, based on the PaO2/FiO2 ratio.
59. What is the summary of the clinical assessment of ARDS?
Hyperventilation, respiratory alkalosis, dyspnea, hypoxemia, metabolic acidosis, respiratory acidosis, hypotension, decreased carbon dioxide, and death.
60. What is not required as a component in the diagnosis of ARDS?
Heart failure
61. What is the basic pathogenesis of ARDS?
Initiation (includes triggering/injuring event), amplification, and injury.
62. What happens in the initiation phase of the pathogenesis of ARDS?
A precipitating event and inflammatory response.
63. What is the amplification phase of the pathogenesis of ARDS?
Immune cells (e.g., neutrophils) are recruited and activated, then migrate into the pulmonary parenchyma.
64. What is the injury phase of the pathogenesis of ARDS?
Immune cells (e.g., neutrophils) release damaging substances that injure the lung tissue.
65. What are the clinical presentations of ARDS?
Decreased pulmonary compliance, increased work of breathing, fatigue, decreased tidal volume, and diminished gas exchange.
66. What happens to the lung parenchyma as ARDS worsens?
End-stage fibrosis, remodeling of lung architecture, and “honeycomb lung.”
67. What lung field does ARDS affect?
ARDS typically affects most lung fields.
68. How does oxygen therapy affect patients with ARDS?
Hypoxemia may occur despite oxygen administration because of the shunting and mixing of unoxygenated blood.
69. What are the clinical phases of ARDS?
Phase 1 (acute injury), Phase 2 (latent phase), Phase 3 (acute respiratory failure), and Phase 4 (severe abnormalities).
70. What happens in Phase 1 of ARDS?
Phase 1, or the “acute injury” phase, is characterized by edema and thickening of the alveolar-capillary membrane. The chest x-ray will be normal. Early changes in this phase result in dyspnea and tachypnea. Intervention for this is to provide oxygen therapy and support.
71. What happens in Phase 2 of ARDS?
Phase 2, or the “latent phase”, happens 6-38 hours after the injury. The manifestation of increasing edema, right-to-left pulmonary shunting, V/Q mismatch, hyperventilation that leads to hypocapnia, and increased work of breathing can be observed. Patchy infiltrates form from pulmonary edema is an early stage change of this phase. It can be intervened through mechanical ventilation and prevention of complications.
72. What happens in Phase 3 of ARDS?
Phase 3, or the “acute respiratory failure” phase, involves inflammatory damage of type II alveolar cells, which results in the inhibition of surfactant production. This inhibition causes decreased compliance that leads to increased work of breathing such as tachypnea, dyspnea, high-pitched, and diffuse crackles. Phase 3 occurs over 2-10 days with an early-stage change of progressive hypoxemia that can be managed by maintaining oxygenation and supporting the failing lung until it can heal.
73. What happens in Phase 4 of ARDS?
Phase 4, or the “severe abnormalities phase,” is considered a chronic phase with characteristics of late effects that develop over time. It includes fibrin deposition resulting in fibrosis, permanent alveolar damage, severe hypoxemia that is unresponsive to therapy, and metabolic and respiratory acidosis. Phase 4 occurs after 10 days and can lead to pulmonary fibrosis pneumonia. At this stage, ARDS may be irreversible.
74. How should you treat ARDS?
While there is no known cure for ARDS, treatment involves managing the symptoms.
75. What does “alveolar recruitment” mean?
It involves the opening of closed alveoli (i.e., recruiting more alveoli to hold air).
76. Does ARDS affect all parts of the lung?
No, even in this condition, there are patches of normal lung.
77. What can affect ARDS symptoms?
Position; patients should be turned periodically to improve oxygenation.
78. What is the prognosis for acute respiratory failure with ARDSnet?
26-44% mortality
79. What is a characteristic of ARDS?
Severe hypoxemia that can rapidly lead to acute respiratory failure.
80. Is ARDS difficult to diagnose, and if not promptly treated, can it be fatal?
Yes, diagnosing this disease is difficult and can be fatal within 48 hours of onset.
81. What mortality rate is highest for patients with ARDS?
Patients 65 years and older with coexisting organ failure.
82. What are the lasting effects that can occur from severe cases of ARDS?
Persistent pulmonary fibrosis, symptoms of restrictive lung diseases with decreased expansion, increased work of breathing (WOB), and inadequate ventilation.
83. The acute phase of ARDS may cause a rapid onset of what?
There is a rapid onset of severe dyspnea that occurs 12-48 hours after the initial injury.
84. What is a characteristic of ARDS when dealing with supplemental oxygen?
ARDS causes arterial hypoxemia that doesn’t respond to supplemental oxygen.
85. What are some other signs and symptoms of ARDS?
Rapid, shallow breathing; intercostal retractions; rhonchi and crackles; tachycardia; decreased urine output; respiratory alkalosis; cyanosis; altered mental status due to low oxygen levels and hypotension.
86. What phase of ARDS involves hyaline membrane formation and alveolar damage?
The exudative phase.
87. What is the hallmark feature of ARDS on a chest X-ray?
Bilateral diffuse pulmonary infiltrates without signs of cardiac enlargement.
88. What is the Berlin definition criteria for diagnosing ARDS?
Acute onset within 1 week of known insult, bilateral opacities on imaging, non-cardiogenic origin, and PaO₂/FiO₂ ratio ≤ 300 mmHg.
89. Which of the following is a direct cause of ARDS?
Pneumonia
90. Which of the following is an indirect cause of ARDS?
Sepsis
91. What happens to lung compliance in ARDS?
Lung compliance decreases due to stiff, fluid-filled alveoli.
92. What is the most appropriate initial ventilator strategy for a patient with ARDS?
Low tidal volume ventilation (4–6 mL/kg of predicted body weight).
93. Why is PEEP used in patients with ARDS?
To prevent alveolar collapse and improve oxygenation by keeping alveoli open during exhalation.
94. What is the typical appearance of ARDS on CT imaging?
Ground-glass opacities and dependent consolidation.
95. What is the primary goal of ARDS management?
To maintain adequate oxygenation while minimizing ventilator-induced lung injury.
96. Which gas exchange abnormality is most commonly associated with ARDS?
Refractory hypoxemia
97. Why is fluid management important in ARDS treatment?
To reduce pulmonary edema and improve oxygenation without compromising perfusion.
98. What is prone positioning and how does it help in ARDS?
Turning the patient onto their abdomen to improve ventilation-perfusion matching and oxygenation.
99. What is the mortality rate of severe ARDS despite optimal treatment?
Approximately 40–50%.
100. Which lab value is most helpful in identifying hypoxemia severity in ARDS?
PaO₂/FiO₂ ratio (P/F ratio).
Final Thoughts
Acute respiratory distress syndrome (ARDS) is a complex and critical condition that demands prompt recognition and aggressive medical management. Its rapid onset and potential for severe respiratory failure make it one of the most challenging complications in critical care.
While advances in supportive therapies, such as protective mechanical ventilation and prone positioning, have improved outcomes, ARDS still carries significant risks of long-term complications and mortality.
Early intervention, addressing the underlying cause, and providing comprehensive supportive care are essential to improving survival and recovery. As research continues to evolve, a better understanding of ARDS may lead to more targeted treatments and improved patient outcomes in the future.
Written by:
John Landry is a registered respiratory therapist from Memphis, TN, and has a bachelor's degree in kinesiology. He enjoys using evidence-based research to help others breathe easier and live a healthier life.
References
- Faarc, Kacmarek Robert PhD Rrt, et al. Egan’s Fundamentals of Respiratory Care. 12th ed., Mosby, 2020.
- Diamond M, Peniston HL, Sanghavi DK, et al. Acute Respiratory Distress Syndrome. [Updated 2023 Apr 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023.
- Fernando SM, Ferreyro BL, Urner M, Munshi L, Fan E. Diagnosis and management of acute respiratory distress syndrome. CMAJ. 2021.



